Search Results for: climate
Climate Change
This topic area covers statistics and information relating to climate change in Hull including local strategic need and service provision. Further information is also available about Hull and the environment can be found under Geographical Area within Place, and under Air Pollution within Health and Wellbeing Influences.
Headlines
- Humans interact with the environment constantly. These interactions affect quality of life, years of healthy life lived, and health disparities.
- The Intergovernmental Panel on Climate Change state that we are currently experiencing the greatest change in the natural environment in human history.
- Climate change impacts on biodiversity strips with a decline of global biodiversity of 69% between 1970 and 2018.
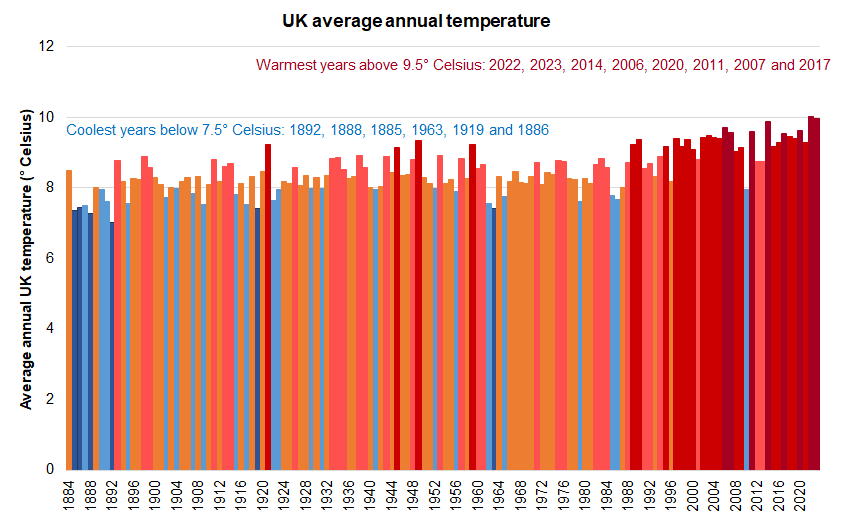
- The hottest eight years since records began in 1884 were between 2006 and 2023 and all had an average annual temperature above 9.5° Celsius with the latest two years 2022 and 2023 having the highest average annual temperature of 10.0° Celsius. In contrast, four of the six coolest years were between 1885 and 1892 which all had an average annual temperature of below 7.5° Celsius (as did 1919 and 1963).
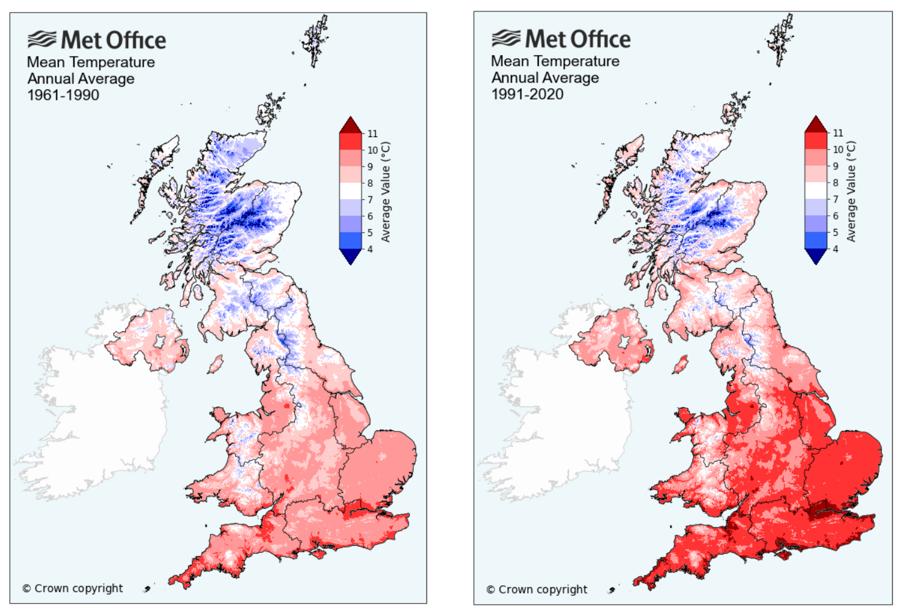
- The average annual temperature in Hull has increased from between 9° Celsius and 10° Celsius for the period 1961 to 1990 to between 10° Celsius and 11° Celsius for the period 1991 to 2020.
- There were severe flooding events in Hull in 2007 and 2013 which had a significant impact on individuals and communities. The likelihood of these flooding events has increased because of global heating.
- In July 2019, Hull had a new temperature record of 35° Celsius, and only three years later in July 2022, this was broken with a new record of 37° Celsius. These high temperature records are the consequences of only a 1.1° Celsius increase in global temperatures.
- The number of climate risks requiring adaptation are increasing with significant impacts on people’s health, life support systems, and health and care providers.
- There is the potential for measures introduced to resolve one problem to be detrimental to other strategies, so full consultation and engagement between the different areas and an assessment of the impacts of any council actions is essential to ensure strategies complement each other.
The Population Affected – Why Is It Important?
Climate change is the greatest threat faced by humanity and the natural world. Emissions from the burning of fossil fuels has seen global temperature increase by 1.1° Celsius since the industrial revolution and under current “business as usual” we are on course for a global temperature increase of 3° Celsius.
The Paris Agreement set a global target to limit global heating to not more than 2° Celsius with an aim to keep temperature increase to no more than 1.5° Celsius. The science indicates that at global temperatures of 2° Celsius there is an increased danger of feedback loops in the natural world and the risk of cascade effects. For example, the melting of permafrost releases methane into the atmosphere which drives further temperature increase which drives increased permafrost melting.
The science of climate change clearly shows that actions by humans are driving these changes through a robust evidence contained in a number of reports published in 2021 and 2022 by the United Nations.
As a result of this the world is passing a number of tipping points for planetary boundaries covering air quality, climate change, water, and natural environment and other life supporting systems provided by earth. More information on planetary boundaries can be found here https://www.stockholmresilience.org/research/planetary-boundaries.html
The Intergovernmental Panel on Climate Change state that we are currently experiencing the greatest change in the natural environment in human history. The threat of climate change as a result of the increase of greenhouse gases by human activity is pushing known planetary boundaries in areas such as species loss, air quality, natural resources and extreme weather events. The increasing global population expansion and dietary change to a more meat-based diet is putting pressure on agriculture and land use.
Climate change impacts on biodiversity (trees, plants, birds, animals, oceans, fish, corals, etc) with a decline of global biodiversity of 69% between 1970 and 2018.
Climate change is affecting the frequency and intensity of extreme weather events such as flooding, storms, forest and moorland fires and heat waves. These weather events impact the most vulnerable in society for example the young and old, and this with lifelong limiting illness, and those most economically disadvantaged, who are least able to recover from such events. We are seeing increased global carbon dioxide concentrations each year and even during the global COVID-19 pandemic concentrations in 2020 set a new record. This is driving increased temperature and new records being set for warmest years on record. Current scientific evidence published by the United Nations Intergovernmental Panel on Climate Change show that the climate impacts we are experiencing are a result of only a 1.1° Celsius rise in global temperatures and the Paris Agreement has set a target to restrict global heating to well below 2° Celsius with an ambition to restrict to 1.5° Celsius.
In the 140 years from 1884 to 2023 inclusive, there has been a clear increase in the average annual temperature in the UK as a result of human activity.
There have been six years where the average annual temperature was below 7.5° Celsius. The lowest three temperatures all occurred in the 1800s (7.02° Celsius in 1892, 7.28° Celsius in 1888 and 7.36° Celsius in 1885) with the most recent year being 1963 which had the fourth coolest temperature since records began in 1884 (7.42° Celsius in 1919 and 7.45° Celsius in 1886 complete the list of the lowest six average annual UK temperatures).
There have been eight years where the average annual temperature was greater than 9.5° Celsius. All eight of these years were between 2006 and 2023 with the latest two years 2022 and 2023 having the highest average annual temperatures recorded at 10.03° Celsius for 2022 and 9.97° Celsius for 2023 (9.88° Celsius in 2014, 9.70° Celsius in 2006, 9.62° Celsius in 2020, 9.61° Celsius in 2011, 9.56° Celsius in 2007 and 9.53° Celsius in 2017 were the remaining years where the temperature was above 9.5° Celsius).
The averages of the average annual temperatures were:
- 7.95° Celsius for the 16 years from 1884 to 1899 (range 7.02° Celsius to 8.88° Celsius)
- 8.29° Celsius for the 50 years from 1900 to 1949 (range 7.42° Celsius to 9.34° Celsius)
- 8.43° Celsius for the 50 years from 1950 to 1999 (range 7.41° Celsius to 9.41° Celsius)
- 9.32° Celsius for the 24 years from 2000 to 2023 (range 7.94° Celsius to 10.03° Celsius).
The average annual temperature varies throughout the UK depending on numerous factors such as latitude (the average annual temperature ranges from about 7° Celsius in the Shetlands to over 11° Celsius in Cornwall and the Channel Islands), altitude (decrease of about 0.5° Celsius for each 100 metres increase in altitude), and to some extent proximity to the coast. There is also a seasonal variation (over the year) and diurnal variation (over the day).
The average annual temperatures have increased between 1961-1990 and 1991-2020 for most areas of the UK.
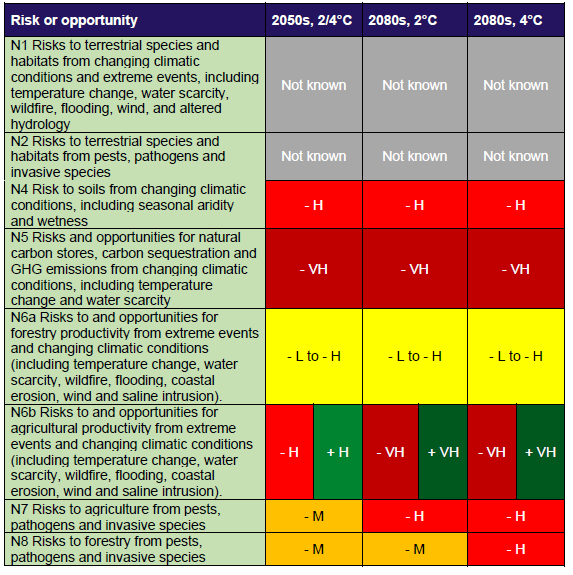
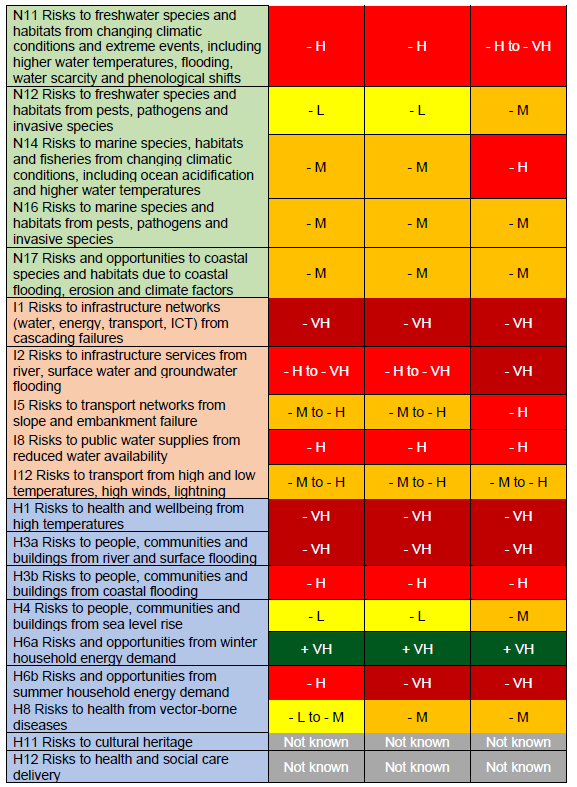
The UK Climate Change Act 2008 (2050 Target Amendment) Order 2019 has set a target to reduce carbon emissions by 100% by 2050 (from a 1990 baseline). In 2020 the UK’s average surface temperature had risen by 1.2° Celsius. Further, in 2022 the Government published the latest Climate Change Risk Assessment following advice from the Committee on Climate Change. The risk assessment looked at the impact of the risks and opportunities from climate change under a 2° Celsius and 4° Celsius global heating scenario.
This identified sixty-one risks and opportunities with thirty-four of them requiring more action within the next five years, to 2027. Twenty-two where more research was needed, four where we needed to sustain current action and three where we needed to maintain a watching brief.
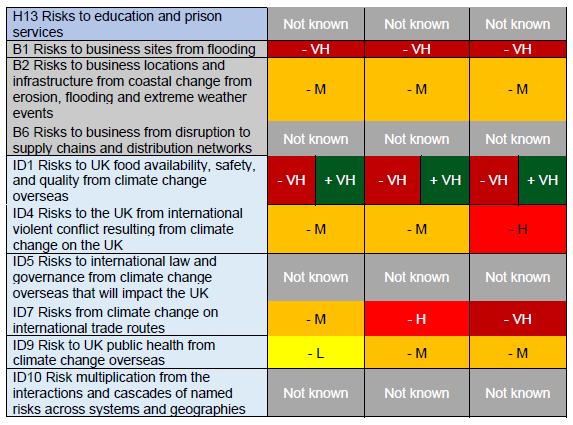
Many of the risks either have a direct effect on people’s health such as heatwaves, flooding and increase in pathogens, or an indirect impact through affecting health functions to operate such as flooding of roads, buildings etc. The table below from the UK Climate Change Risk Assessment 2022 provides a good starting point to understand the risks over the rest of the century.
The potential costs and damages (economic costs or forgone opportunities) are denoted with a negative sign, and possible opportunities are denoted with a positive sign. Where uncertainty exists over the category, the range has been indicated. For some of the risks and opportunities, there are both potential costs and benefits. The risks and benefits are denoted as follows:
- Very High (VH) is over £1 billion per year.
- High (H) is over hundreds of millions of pounds per year.
- Medium (M) is over tens of millions of pounds per year.
- Low (L) is less than ten million pounds per year.
There is therefore an imperative to increase the scale and pace of action to reduce carbon emissions, and to significantly increase adaptation activity to prepare for the inevitable consequences of climate change.
A third National Adaptation Programme was published in July 2023 that provides the action plan to address the risks identified, and covers the period 2024-2028. This risk assessment and Programme provide a sound strategic focus for joint strategic needs action.
In 2014, the Joseph Rowntree Foundation produced an evidence review of climate change and social justice. Their review identified five different forms of climate injustice in the UK context, and found that lower income and other disadvantaged groups contributed the least to causing climate change yet they were the most likely to be negatively impacted by its effects. They were also less able to participate in decision-making around policy responses.
In 2018, a revised webtool developed by the Joseph Rowntree Foundation and University of Manchester, Climate Just, demonstrated that residents who were already vulnerable due to age, long term life limiting illnesses and poverty are least able to be resilient to the impacts of climate change and are more adversely affected than the average resident.
The Hull Picture
The city of Hull has experienced several extreme weather events over the last twenty years that have put increased pressure on public health services. The floods in 2007 affected significant parts of the city with some families not being able to return to their homes for up to two years. The tidal surge in December 2013 closed the A63 and the Transpennine rail line, and the snow and ice winters in 2010 and 2011 affected roads with some impassable for weeks and increased the number of people suffering falls. Hull has experienced significant heatwaves in July 2019 with a new temperature record of 35° Celsius and only three years later in July 2022 this was broken with a new record of 37° Celsius. These heatwaves are likely to increase in intensity and frequency as the century progresses with increased pressure on health and care services.
The impacts of climate change will disproportionately affect the most vulnerable and therefore put increased pressure on public health and health services in Hull.
In response to the increasing impacts of climate change and global heating Hull City Council declared a Climate Emergency in 2019 and produced the Hull 2030 Carbon Neutral Strategy in 2020 setting out the key challenges faced and an initial suite of actions.
In 2022 the Council agreed a 2045 net zero target for the city and a 2040 net zero target for the Council to bring the cities and Council’s ambitions in line with national climate action. This followed extensive research with the Carbon Trust to establish a science-based target for the city under a high ambition reduction scenario. This includes several carbon pathways for key sectors to meet the net zero target.
Strategic Need and Service Provision
Since January 2013, Hull City Council has held the highest Green Accreditation for its environmental management system, Investors in the Environment and undertaken work to reduce its carbon emissions in line with its corporate targets.
There is a need to better understand the extent of climate risk to public health and the wider health services in the City. The development of effective climate adaptation for services and facilities would ensure that they are more resilient to extreme weather events and therefore reduce the emergency impact on public health services.
It is necessary to work with partners to reduce the impact of extreme weather events and wider emergency events and seek assurance of preparedness, response and recovery when events happen. To create a natural and physical environment that is resilient to climate change.
The cost of extreme weather events to public health services is not well understood and there is a need to better understand the financial and human impacts so that this can support timely and effective climate adaptation investment. The experience of the significant flooding events have shaped how we build homes, support vulnerable residents and business and undertake resilience work at the city and community level. We have a greater understanding of how we interact with our environment and the key role it plays in improving public health as well as how it can affect people’s life chances. We also have a greater understanding and working relationship across service providers in how our actions impact each other and how through greater project integration we can build a whole system approach to the challenges.
Resources
Climate Change Explained. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1163722/climate-change-explained.pdf
The Paris Agreement. United Nations, Climate Change. https://unfccc.int/process-and-meetings/the-paris-agreement/the-paris-agreement
Climate Action. United Nations. https://www.un.org/en/climatechange/reports
Average annual temperatures in the UK. Met Office, 1884 to 2023. https://www.metoffice.gov.uk/pub/data/weather/uk/climate/datasets/Tmean/date/UK.txt
UK climate averages. Average maps. Met Office, 1961-1990 and 1991-2020. https://www.metoffice.gov.uk/research/climate/maps-and-data/uk-climate-averages/gcxdqnhwn
Climate change impacts on biodiversity strips. https://biodiversitystripes.info/global/
UK Climate Change Risk Assessment 2022. UK Government. https://www.gov.uk/government/publications/uk-climate-change-risk-assessment-2022
Independent Assessment of UK Climate Risk. Climate Change Committee, 2021. https://www.theccc.org.uk/publication/independent-assessment-of-uk-climate-risk/
Climate change: second national adaptation programme (2018 to 2023). UK Government, 2018. https://www.gov.uk/government/publications/climate-change-second-national-adaptation-programme-2018-to-2023
Climate change: Atmospheric Carbon Dioxide. https://www.climate.gov/news-features/understanding-climate/climate-change-atmospheric-carbon-dioxide#:~:text=October%207%2C%202021-,Highlights,2020%3A%20412.5%20parts%20per%20million
2021 Tied for 6th Warmest Year in Continued Trend, NASA Analysis Shows. Global Climate Change, 2022. https://climate.nasa.gov/news/3140/2021-tied-for-6th-warmest-year-in-continued-trend-nasa-analysis-shows/
What is climate change? Met Office. https://www.metoffice.gov.uk/weather/climate-change/what-is-climate-change
The Climate Change Act 2008 (2050 Target Amendment) Order 2019. https://www.legislation.gov.uk/uksi/2019/1056/contents/made
Intergovernmental Panel on Climate Change. Climate Change 2023: Synthesis Report – Summary for Policymakers. https://www.ipcc.ch/report/ar6/syr/downloads/report/IPCC_AR6_SYR_SPM.pdf
Climate Change 2021: The Physical Science Basis. Intergovernmental Panel on Climate Change. https://www.ipcc.ch/report/ar6/wg1/downloads/report/IPCC_AR6_WGI_Full_Report.pdf
Climate change and social justice: an evidence review. Joseph Rowntree Foundation, 2014. https://www.jrf.org.uk/climate-change-and-social-justice-an-evidence-review
Climate Just. Climate UK, Joseph Rowntree Foundation, Environmental Agency, University of Manchester, 2018.
National Adaptation Programme 2023. HM Government https://www.gov.uk/government/publications/third-national-adaptation-programme-nap3
Updates
This page was last updated / checked on 16 September 2025.
This page is due to be updated / checked in September 2026.
Infectious Diseases
This topic area covers statistics and information relating to infectious diseases in Hull including local strategic need and service provision. This section of the JSNA only includes statistics and information from a small number of infectious diseases where data is available on Office for Health Improvement & Disparities’ Fingertips. There are many more infectious diseases, but information is not necessarily available on these. Further information on some other infectious diseases within this JSNA can be found under Coronavirus (COVID-19), Respiratory Diseases and Sexually Transmitted Infectious under Health Factors within Adults. Information relating to vaccinations can be found within Vaccinations under Prevention for Adults, and within Screening and Vaccinations under Health Factors for Children and Young People.
This page includes information on the number of new laboratory confirmed cases of escherichia coli (e coli), methicillin-resistant staphylococcus aureus (MRSA), clostridium difficile (c difficile), klebsiella and pseudomonas aeruginosa (p aeruginosa) as well as information on tuberculosis (TB), mortality from communicable diseases, and antibiotic prescribing in primary care in order to reduce antimicrobial resistance.
If you need to report an infectious diseases, contact your local Health Protection Team.
This page contains information from the Office for Health Improvement & Disparities’ Fingertips. Information is taken ‘live’ from the site so uses the latest available data from Fingertips and displays it on this page. As a result, some comments on this page may relate to an earlier period of time until this page is next updated (see review dates at the end of this page). This is particularly the case for this JSNA page, as the indicators relating to infections are updated more regularly on Fingertips than the update schedule for this page.
Headlines
- Some infectious diseases can cause high levels of mortality and disability whereas the effects from others can be relatively mild. However, there are available measures to reduce spread such as limiting contact with others, making occupied spaces well ventilated, maintaining good hygiene, taking up vaccinations, and reporting infectious diseases where appropriate so potential outbreaks can be managed. A communicable disease is a contagious infectious disease.
- In 2023/24, there were 269 laboratory confirmed cases of Escherichia coli (E. coli) in Hull which equates to a rate of 100 cases per 100,000 population. This was higher than England (74 cases per 100,000 population). The majority of the cases (208; 77%) were community-onset cases. There has been a relatively sharp increase in the number of infections in Hull in the last year.
- The number of laboratory confirmed cases of methicillin-resistant straphylococcus aureus (MRSA) are low in Hull as they are across England and the region. In 2023/24, there were three laboratory confirmed cases and the confirmed case rate slightly lower than England (1.1 versus 1.6 cases per 100,000 population). None of these cases were community-onset in Hull in 2023/24. The rate in Hull has generally been lower than England.
- During 2023/24, there were 43 laboratory confirmed cases of Clostridium difficile (C. difficle) in Hull, which was much lower than England (16.0 versus 29.5 cases per 100,000 population). Seven of these cases were community-onset healthcare associated cases and seven were community-onset cases community associated cases. The rate in Hull has been consistently lower than England.
- During 2023/24, there were 79 laboratory cases of Klebsiella Spp. and the rate was higher in Hull than England (29.3 versus 22.9 cases per 100,000 population. Overall, 52 (66%) of these cases were community-onset. There is year-on-year variability in the confirmed infection rate in Hull, but the rate has increased quite sharply in Hull in the last year.
- During 2023/24, there were 27 laboratory confirmed cases of pseudomonas aeurginosa (P. aeruginosa) in Hull. The infection rate was higher in Hull compared to England (10.0 versus 7.8 per 100,000 population). There has been some year-on-year variability, but on the whole, the rate in Hull has been higher than England. In 2023/24, 15 (56%) of these cases were community-onset.
- Over the three year period 2021 to 2023, there were 52 new cases of tuberculosis (TB) in Hull which gave an incidence rate of 6.4 per 100,000 population. In 2001-03, the incidence rate in Hull was more than half that of England (5.1 versus 13.1 per 100,000 population), but has increased over time in Hull as the make up of Hull’s population has changed. For the period 2001-03 to 2016-18, the rate in Hull was statistically significantly lower than England but since then there has been no statistically significant difference between Hull and England (although the rate in Hull has continued to be lower than England). The number of people in Hull with drug sensitive TB is relatively low, and there is considerable variability in the percentages who completed a full course of treatment within 12 months. For the last three years (2020 to 2022), 23 out of 49 (47%) did not complete the full course of treatment in Hull compared to around 15% of cases in England.
- There were 92 deaths among Hull residents from communicable diseases (certain infectious and parasitic diseases and influenza) that were registered during the three year period 2021-23 which gave a mortality rate of 14.2 deaths per 100,000 population. The mortality rate in Hull was higher than England at 13.0 deaths per 100,000 population. The rate in Hull over the last decade or so has been around 10-11 deaths per 100,000 population, so the latest rate of 14.2 deaths per 100,000 population represents an increase in Hull. The mortality rates illustrate year-on-year variability in Hull with a higher number of deaths from sepsis for some years. Whilst the number of deaths from communicable diseases reduced considerably for 2020 due to the COVID-19 pandemic, the total numbers have increased slightly since then with a higher number from flu, although the flu deaths have only made up around 18% of all communicable deaths in Hull in the last six years (2018 to 2023).
- Reduction in antibiotic consumption is a well-recognised target in antimicrobial resistance (AMR) policies both nationally and internationally. In Hull, for 2023, after adjusting for the population, there was a marginally higher rate of antibiotic prescribing in primary care within the NHS compared to England (0.90 versus 0.88 annual total items per STAR PU (Specific Therapeutic group Age sex weightings Related Prescribing Units – using these ‘weighted units’ is a way in which the measure takes into account the differences in the population). For 2015, the rate in Hull was 11% higher than England (1.22 versus 1.10 annual total items per STAR PU) and is currently only 2% higher than England. Thus the antibiotic prescribing rate has reduced in Hull and at a faster rate than the prescribing rate for England.
The Population Affected – Why Is It Important?
From Very Well Health, an infectious disease is an infection, when a microorganism enters the body. For bacteria or fungi, this means dividing and growing new cells at an exponential rate. Viruses have the added hurdle of entering human cells and taking over their control centres so they can make more of themselves. While all communicable diseases are infectious, not all infections are communicable, for example, tetanus can cause an infection, but a person with tetanus cannot spread it to other people. A communicable disease is a contagious one. If someone catches the illness, they can get ill and spread the pathogen onto the next person. This can be transmitted through respiratory droplets from coughing or sneezing, sexual activity, contact with blood, from mother to child during pregnancy, birth or breastfeeding, or ingestion of toxins usually from spoilt and contaminated food. Active illness where a person is coughing or sneezing a lot can give the microbe more opportunities to spread, but a person can still be contagious without symptoms. For instance, measles can be transmitted up to four days before the rash develops, and the virus can stay in the air for as long as two hours after an infected person leaves the room. Other microbes spread through an intermediatory, for instance, malaria is spread by mosquitoes who become infected after biting someone with the disease, and then they, in turn, pass the parasite onto the next person they bite. Some diseases can remain on surfaces such as door handles, and food poisoning in particular can be spread through the faecal-oral route when people don’t wash hands after using the toilet and touch surfaces, that others touch later.
From the World Health Organisation, infectious diseases are caused by pathogenic microorganisms, such as bacteria, viruses, parasites or fungi; the diseases can be spread, directly or indirectly, from one person to another. These diseases can be grouped in three categories: diseases which cause high levels of mortality; diseases which place on populations heavy burdens of disability; and diseases which owing to the rapid and unexpected nature of their spread can have serious global repercussions. Many of the key determinants of health and the causes of infectious diseases lie outside the direct control of the health sector. Other sectors involved are those dealing with sanitation and water supply, environmental and climate change, education, agriculture, trade, tourism, transport, industrial development and housing.
Therefore, it is important to prevent the spread of infectious diseases as much as possible, particularly those infections that have a higher likelihood of causing death and disability.
From the UK Health Security Agency, the general advice for managing outbreaks of infectious diseases in a particular setting or establishment is to encourage people who are unwell to not attend or remain separate from others, ensuring all eligible groups are enabled and supported to take up the offer of vaccinations, ensuring occupied spaces are well ventilated, reinforcing good hygiene practice, and requesting that infectious diseases are reported to the setting or establishment. There are recommendations on how long people should remain away from a setting such as work, school or nursery for specific diseases, and certain infections need to be reported to the Health Protection Teams. The UK Health Security Agency also has advice for Managing Specific Infectious Diseases.
This section of the JSNA only includes statistics and information from a small number of infectious diseases where data is available on Office for Health Improvement & Disparities’ Fingertips. There are many more infectious diseases, but information is not necessarily available on these. Further information on some other infectious diseases within this JSNA can be found under Coronavirus (COVID-19), Respiratory Diseases and Sexually Transmitted Infectious under Health Factors within Adults. Information relating to vaccinations can be found within Vaccinations under Prevention for Adults, and within Screening and Vaccinations under Health Factors for Children and Young People.
E. Coli (Escherichia Coli) Bacteraemia
Escherichia coli (abbreviated as E. coli) bacteria are frequently found in the intestines of humans and animals. There are many different types of E. coli, and while some live in the intestine quite harmlessly, others may cause a variety of diseases.
The bacterium is found in faeces and can survive in the environment. E. coli bacteria can cause a range of infections including urinary tract infection, cystitis (infection of the bladder), and intestinal infection. E. coli bacteraemia (blood stream infection) may be caused by primary infections spreading to the blood.
MRSA (Methicillin-Resistant Staphylococcus Aureus)
Staphylococcus aureus (S. aureus) is a bacterium that commonly colonises human skin and mucosa without causing any problems. It can also cause disease, particularly if there is an opportunity for the bacteria to enter the body, for example through broken skin or a medical procedure.
If the bacteria enter the body, illnesses which range from mild to life-threatening may then develop. These include skin and wound infections, infected eczema, abscesses or joint infections, infections of the heart valves (endocarditis), pneumonia and bacteraemia (blood stream infection).
Most strains of S. aureus are sensitive to the more commonly used antibiotics, and infections can be effectively treated. Some S. aureus bacteria are more resistant. Those resistant to the antibiotic meticillin are termed meticillin resistant Staphylococcus aureus (MRSA) and often require different types of antibiotic to treat them. Those that are sensitive to meticillin are termed meticillin susceptible Staphylococcus aureus (MSSA). MRSA and MSSA only differ in their degree of antibiotic resistance: other than that there is no real difference between them.
Clostridium Difficile (C. Difficile) Infection
Clostridioides difficile (C. difficile) is a bacterium that’s found in people’s intestines. It can be found in healthy people, where it causes no symptoms (up to 3% of adults and 66% of babies).
C. difficile causes disease when the normal bacteria in the gut are disadvantaged, usually by someone taking antibiotics. This allows C. difficile to grow to unusually high levels. It also allows the toxin that some strains of C. difficile produce to reach levels where it attacks the intestines and causes mild to severe diarrhoea.
C. difficile can lead to more serious infections of the intestines with severe inflammation of the bowel (pseudomembranous colitis). C. difficile is the biggest cause of infectious diarrhoea in hospitalised patients.
You can become infected with C. difficile if you ingest the bacterium (through contact with a contaminated environment or person). People who become infected with C. difficile are usually those who’ve taken antibiotics, particularly the elderly and people whose immune systems are compromised.
Klebsiella Spp. Bacteraemia
Klebsiella species are a Gram-negative rod shaped bacteria belonging to the Enterobacteriaceae family. They are commonly found in the environment and in the human intestinal tract (where they do not normally cause disease).
These species can cause a range of healthcare-associated infections, including pneumonia, bloodstream infections, wound or surgical site infections and meningitis. Acquired endogenously (from the patient’s own gut flora) or exogenously from the healthcare environment.
Patient to patient spread occurs through contaminated hands of healthcare workers or less commonly by contamination of the environment. Vulnerable patients, like the immune compromised, are most at risk. Infections can be associated with use of invasive devices or medical procedures.
Klebsiella spp. can become resistant to a wide range of antibiotics through a variety of mechanisms.
Pseudomonas Aeruginosa (P. Aeruginosa) Bacteraemia
Pseudomonas aeruginosa (P. aeruginosa) is a Gram-negative bacterium often found in soil and ground water. P. aeruginosa is an opportunistic pathogen and it rarely affects healthy individuals. It can cause a wide range of infections, particularly in those with a weakened immune system, for example cancer patients, newborns and people with severe burns, diabetes mellitus or cystic fibrosis.
P. aeruginosa infections are sometimes associated with contact with contaminated water. In hospitals, the organism can contaminate devices that are left inside the body, such as respiratory equipment and catheters. P. aeruginosa is resistant to many commonly-used antibiotics.
Tuberculosis (TB)
From the World Health Organisation, tuberculosis (TB) is caused by bacteria (Mycobacterium tuberculosis) and it most often affects the lungs. TB is spread through the air when people with lung TB cough, sneeze or spit. A person needs to inhale only a few germs to become infected. Every year, 10 million people fall ill with TB. Despite being a preventable and curable disease, 1.5 million people die from TB each year – making it the world’s top infectious killer. TB is the leading cause of death of people with HIV and also a major contributor to antimicrobial resistance. Most of the people who fall ill with TB live in low- and middle-income countries, but TB is present all over the world. About half of all people with TB can be found in eight countries: Bangladesh, China, India, Indonesia, Nigeria, Pakistan, Philippines and South Africa. About a quarter of the global population is estimated to have been infected with TB bacteria, but most people will not go on to develop TB disease and some will clear the infection. Those who are infected but not (yet) ill with the disease cannot transmit it. People infected with TB bacteria have a 5–10% lifetime risk of falling ill with TB. Those with compromised immune systems, such as people living with HIV, malnutrition or diabetes, or people who use tobacco, have a higher risk of falling ill.
From the NHS, the main treatment for TB is to take antibiotics for at least six months (or 3-6 months if the person does not have symptoms and has latent TB). If TB has spread to the brain, spinal cord or the area around the heart, then steroid medicine may also be necessary for a few weeks. If the person does not take the antibiotics correctly and complete the full course of treatment, TB can come back. There is a vaccination available for TB called the BCG (Bacillus Calmette-Guérin) vaccine and it is recommended for some people who are at a higher risk of catching TB or getting seriously ill from it.
Data Considerations
Data is available on the Office for Health Improvement & Disparities’ Fingertips for the rate of laboratory confirmed cases of various bacteraemia. For some specific bacteraemia, the numbers are small and in some cases very small with only a handful of cases each year. This means that there will be month-to-month and year-to-year variability in the trends over time, particularly for smaller geographical areas like Hull relative to larger geographical areas like the region or England. It can also mean that it is more tricky to interpret the trends over time as it is possible that a ‘blip’ of one or two fewer or additional cases can impact on the overall rate by a relatively large degree. See Small Numbers in the Glossary for more information.
The rates are given as laboratory confirmed cases, and will not include all cases of the infection. It is also possible that numbers increase over time if there is better detection, testing and/or recording of the specific infection over time. This appears to be the case for some bacteraemia where there were few cases in early 2017 and a more constant number of cases within a year or two (particularly for England where the trends in the infection rates are more stable over time).
On Fingertips, the number of reported cases of infections are given as as a total over a financial year and as a rolling 12-month rate of the number of cases by month for each sub-Integrated Care Board. Hull is within the Humber and North Yorkshire Integrated Care Board, and is coded as ’03F’. Both rates are given as the number of laboratory confirmed cases per 100,000 population.
The 12 month rolling rate is calculated as the total number of cases which occurred in the specified month and the preceding 11 months divided by population of the sub-ICB for the current month and the preceding 11 months. This rate is then multiplied by 100,000 to present as the number of laboratory confirmed cases per 100,000 population.
With the figures quoted as 12-month rolling count, it does mean that a new case will remain in the ‘count’ for a whole 12 month period. For instance, in the case of Methicillin-Resistant Staphylococcus aureus (MRSA), there were three cases in Hull for the year November 2017 to October 2018, and these occurred in November 2017, March 2018 and October 2018 (as the counts increased by one for each of these months). In the year prior to this covering the period, November 2016 to October 2017, there had been no cases in the previous 12 months in Hull. There were two cases in the year December 2017 to November 2018 and these occurred during November 2017 and March 2018 (the case in November 2017 was more than a year ago so dropped out of the 12-month rolling count). There was a new case in January 2019 which increased the annual count to three again. Therefore, the counts for each month should not be summed as this has already been done and this would result in ‘double counting’.
The Hull Picture
E. Coli (Escherichia Coli) Bacteraemia
Cases by Financial Year
The number of laboratory confirmed cases of E. coli is given below for Hull (03F) over a financial year compared to the others within the Humber and North Yorkshire Integrated Care Board, as well as the rate based on those that were community-onset. The rates are given as the number of cases over the year per 100,000 population.
The rate of cases of E. coli over the year for 2023/24 was 35% higher than England and 30% higher than England for community-onset cases.
Compared with benchmark
| Indicator | Period | England | NHS Humber and North Yorkshire Integrated Care Board - QOQ | Humber and North Yorkshire ICB - 02Y | Humber and North Yorkshire ICB - 03F | Humber and North Yorkshire ICB - 03H | Humber and North Yorkshire ICB - 03K | Humber and North Yorkshire ICB - 03Q | Humber and North Yorkshire ICB - 42D |
|---|---|---|---|---|---|---|---|---|---|
E. coli bacteraemia case counts and rates by Sub ICB locations (SICBL) and financial year (Persons All ages) | 2023/24 | 73.8 | 89.2 | 92.4 | 99.8 | 63.9 | 77.5 | 79.9 | 102.1 |
E. coli bacteraemia case counts and rates of community-onset, by sub ICB location (SICBL) and financial year (Persons All ages) | 2023/24 | 59.5 | 73.6 | 75.1 | 77.2 | 53.8 | 61.0 | 70.1 | 85.6 |
| Indicator | Period | England | NHS Humber and North Yorkshire Integrated Care Board - QOQ | Humber and North Yorkshire ICB - 02Y | Humber and North Yorkshire ICB - 03F | Humber and North Yorkshire ICB - 03H | Humber and North Yorkshire ICB - 03K | Humber and North Yorkshire ICB - 03Q | Humber and North Yorkshire ICB - 42D |
|---|---|---|---|---|---|---|---|---|---|
E. coli bacteraemia case counts and rates by Sub ICB locations (SICBL) and financial year (Persons All ages) | 2023/24 | 73.8 | 89.2 | 92.4 | 99.8 | 63.9 | 77.5 | 79.9 | 102.1 |
E. coli bacteraemia case counts and rates of community-onset, by sub ICB location (SICBL) and financial year (Persons All ages) | 2023/24 | 59.5 | 73.6 | 75.1 | 77.2 | 53.8 | 61.0 | 70.1 | 85.6 |
The rate of E. coli cases in Hull had been increasing between 2014/15 and 2019/20 from 70 to 96 cases per 100,000 population, although this might have occurred by chance as there is some year-on-year variability and the rate in 2014/15 was particularly low (the rate in 2013/14 was nearly as high as the peak in 2018/19). The rate decreased to 76 per 100,000 population in 2020/21 due to the pandemic and presumably fewer hospital-onset cases due to the lower admission rates for non-COVID conditions. The rate has increased slightly between 2020/21 and 2022/23 from 76 to 80 cases per 100,000 population with a sharp increase between 2022/23 and 2023/24 to 100 cases. The rate in 2023/24 for Hull is the highest it has been since 2012/13.
Between 2012/13 and 2022/23, the rate of E. coli cases has followed a similar pattern in England, although there has been less variability and the rate in Hull has been consistently higher than England. However, in the last year, the rate of infection increased across England, but the rate of increase was markedly higher in Hull.
Over the year 2023/24, there were 269 cases of E. coli reported in Hull.
Compared with benchmark
E. coli bacteraemia case counts and rates by Sub ICB locations (SICBL) and financial year (Persons All ages)
|
Period
|
Humber and North Yorkshire ICB - 03F |
NHS Humber and North Yorkshire Integrated Care Board - QOQ
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2012/13 | • | 197 | 76.8 | - | - | 73.0 | 60.4 |
| 2013/14 | • | 242 | 94.1 | - | - | 78.4 | 63.5 |
| 2014/15 | • | 179 | 69.5 | - | - | 78.0 | 65.8 |
| 2015/16 | • | 210 | 80.9 | - | - | 80.8 | 69.6 |
| 2016/17 | • | 235 | 90.5 | - | - | 88.2 | 73.6 |
| 2017/18 | • | 237 | 90.9 | - | - | 88.6 | 73.8 |
| 2018/19 | • | 256 | 98.3 | - | - | 93.2 | 77.2 |
| 2019/20 | • | 250 | 96.1 | - | - | 92.7 | 76.9 |
| 2020/21 | • | 195 | 74.9 | - | - | 78.1 | 65.2 |
| 2021/22 | • | 204 | 76.4 | - | - | 76.8 | 67.1 |
| 2022/23 | • | 214 | 79.6 | - | - | 83.3 | 67.9 |
| 2023/24 | • | 269 | 99.8 | - | - | 89.2 | 73.8 |
Source: UK Health Security Agency
As around three-quarters of E. coli cases were community-onset, the trends over time for community-onset E. coli follow a similar pattern with an increase between 2014/15 and 2019/20 with a decrease in 2020/21 due to the pandemic and less population mixing, and an increase subsequently, with the latest rate around the same as the peak prior to the pandemic.
A reasonably similar pattern of change has occurred for England, but again the rate of variability has been much greater in Hull. The infection rate has increased since the low of 2020/21 for both Hull and England, but the rate of increase has been higher particularly in the last year.
Over the year 2023/24, there were 208 cases of E. coli reported in Hull which were community-onset, which is 77% of all cases reported.
Compared with benchmark
E. coli bacteraemia case counts and rates of community-onset, by sub ICB location (SICBL) and financial year (Persons All ages)
|
Period
|
Humber and North Yorkshire ICB - 03F |
NHS Humber and North Yorkshire Integrated Care Board - QOQ
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2012/13 | • | 154 | 60.0 | - | - | 54.1 | 46.3 |
| 2013/14 | • | 182 | 70.8 | - | - | 58.8 | 49.5 |
| 2014/15 | • | 136 | 52.8 | - | - | 60.3 | 52.3 |
| 2015/16 | • | 155 | 59.7 | - | - | 63.7 | 55.6 |
| 2016/17 | • | 196 | 75.5 | - | - | 71.5 | 59.4 |
| 2017/18 | • | 185 | 71.0 | - | - | 71.6 | 60.1 |
| 2018/19 | • | 206 | 79.1 | - | - | 76.0 | 63.6 |
| 2019/20 | • | 198 | 76.1 | - | - | 75.5 | 63.0 |
| 2020/21 | • | 144 | 55.3 | - | - | 64.9 | 53.7 |
| 2021/22 | • | 156 | 58.4 | - | - | 62.8 | 54.6 |
| 2022/23 | • | 157 | 58.4 | - | - | 66.7 | 54.1 |
| 2023/24 | • | 208 | 77.2 | - | - | 73.6 | 59.5 |
Source: UK Health Security Agency
Cases by Month (12-Month Rolling Total)
The 12-month rolling total count of the number of laboratory confirmed cases of E. coli is given below for Hull (03F) compared to the others within the Humber and North Yorkshire Integrated Care Board, as well as the rate based on those that were hospital-onset or community-onset.
For April 2025, the rates in Hull are considerably higher than England particularly for hospital-onset and overall.
Compared with benchmark
| Indicator | Period | England | NHS Humber and North Yorkshire Integrated Care Board - QOQ | Humber and North Yorkshire ICB - 02Y | Humber and North Yorkshire ICB - 03F | Humber and North Yorkshire ICB - 03H | Humber and North Yorkshire ICB - 03K | Humber and North Yorkshire ICB - 03Q | Humber and North Yorkshire ICB - 42D |
|---|---|---|---|---|---|---|---|---|---|
E. coli bacteraemia 12-month rolling case counts and rates, by Sub ICB Location (SICBL) and month (Persons All ages) | Jun 2025 | 77.0 | 93.7 | 99.3 | 100.0 | 52.1 | 92.5 | 93.5 | 101.5 |
E. coli bacteraemia 12-month rolling case counts and rates of hospital-onset, by Sub ICB Location (SICBL) and month (Persons All ages) | Jun 2025 | 14.7 | 18.3 | 26.8 | 26.5 | 12.1 | 13.0 | 14.3 | 14.7 |
E. coli bacteraemia 12-month rolling case counts and rates of community-onset, by Sub ICB Location (SICBL) and month (Persons All ages) | Jun 2025 | 62.3 | 75.4 | 72.6 | 73.5 | 40.0 | 79.5 | 79.2 | 86.8 |
| Indicator | Period | England | NHS Humber and North Yorkshire Integrated Care Board - QOQ | Humber and North Yorkshire ICB - 02Y | Humber and North Yorkshire ICB - 03F | Humber and North Yorkshire ICB - 03H | Humber and North Yorkshire ICB - 03K | Humber and North Yorkshire ICB - 03Q | Humber and North Yorkshire ICB - 42D |
|---|---|---|---|---|---|---|---|---|---|
E. coli bacteraemia 12-month rolling case counts and rates, by Sub ICB Location (SICBL) and month (Persons All ages) | Jun 2025 | 77.0 | 93.7 | 99.3 | 100.0 | 52.1 | 92.5 | 93.5 | 101.5 |
E. coli bacteraemia 12-month rolling case counts and rates of hospital-onset, by Sub ICB Location (SICBL) and month (Persons All ages) | Jun 2025 | 14.7 | 18.3 | 26.8 | 26.5 | 12.1 | 13.0 | 14.3 | 14.7 |
E. coli bacteraemia 12-month rolling case counts and rates of community-onset, by Sub ICB Location (SICBL) and month (Persons All ages) | Jun 2025 | 62.3 | 75.4 | 72.6 | 73.5 | 40.0 | 79.5 | 79.2 | 86.8 |
During early 2015, there were around 200 cases of E. coli per year when examining the rolling 12-monthly figures equating to around 17 cases on average per month. This gradually increased to reach a peak of around 260 cases per year (so around 22 per month) prior to the COVID-19 pandemic (lockdown commenced March 2020). The rates fell quite sharply during 2020 and early 2021 to reach a low of around 190 cases per year (around 16 per month). However, rates have gradually increased over time to reach to around 250-270 cases for October 2023 to September 2024 (around 21 cases per month).
The rates in Hull have been consistently higher than those across England, and consistently higher than the regional average since May 2023. The rates have increased for both England and the region since the low rates during the pandemic, but the rate of increase has been greater in Hull particularly since May 2023.
This has increased the inequalities gap between Hull and England. The infection rate for the 2024 and up to April 2025 has been just under 100 cases per 100,000 population is only just below the peak prior to the pandemic for the period March 2019 to February 2020 at 102 cases per 100,000 population.
In the latest period, May 2024 to April 2025, there were 249 cases of E. coli bacteraemia in Hull.
Compared with benchmark
E. coli bacteraemia 12-month rolling case counts and rates, by Sub ICB Location (SICBL) and month (Persons All ages)
|
Period
|
Humber and North Yorkshire ICB - 03F |
NHS Humber and North Yorkshire Integrated Care Board - QOQ
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| Dec 2014 | • | 202 | 77.4 | - | - | 78.9 | 65.6 |
| Jan 2015 | • | 192 | 73.5 | - | - | 78.3 | 65.6 |
| Feb 2015 | • | 188 | 72.0 | - | - | 78.3 | 65.7 |
| Mar 2015 | • | 179 | 68.5 | - | - | 78.1 | 65.8 |
| Apr 2015 | • | 179 | 68.5 | - | - | 77.9 | 65.8 |
| May 2015 | • | 184 | 70.3 | - | - | 78.0 | 65.8 |
| Jun 2015 | • | 188 | 71.8 | - | - | 79.2 | 66.2 |
| Jul 2015 | • | 185 | 70.6 | - | - | 78.9 | 66.4 |
| Aug 2015 | • | 182 | 69.4 | - | - | 77.7 | 66.6 |
| Sep 2015 | • | 184 | 70.2 | - | - | 78.0 | 67.1 |
| Oct 2015 | • | 192 | 73.2 | - | - | 79.4 | 67.5 |
| Nov 2015 | • | 200 | 76.2 | - | - | 78.9 | 67.9 |
| Dec 2015 | • | 205 | 78.0 | - | - | 78.1 | 68.3 |
| Jan 2016 | • | 214 | 81.4 | - | - | 79.6 | 68.9 |
| Feb 2016 | • | 208 | 78.9 | - | - | 80.5 | 69.1 |
| Mar 2016 | • | 210 | 79.6 | - | - | 81.0 | 69.6 |
| Apr 2016 | • | 218 | 82.6 | - | - | 81.1 | 69.8 |
| May 2016 | • | 218 | 82.5 | - | - | 80.2 | 70.4 |
| Jun 2016 | • | 218 | 82.4 | - | - | 80.3 | 70.7 |
| Jul 2016 | • | 218 | 82.4 | - | - | 82.6 | 71.2 |
| Aug 2016 | • | 225 | 85.0 | - | - | 85.5 | 71.9 |
| Sep 2016 | • | 226 | 85.3 | - | - | 86.1 | 72.0 |
| Oct 2016 | • | 228 | 86.0 | - | - | 86.2 | 72.4 |
| Nov 2016 | • | 235 | 88.6 | - | - | 87.6 | 72.6 |
| Dec 2016 | • | 233 | 87.7 | - | - | 86.9 | 73.0 |
| Jan 2017 | • | 232 | 87.3 | - | - | 86.1 | 72.9 |
| Feb 2017 | • | 231 | 87.1 | - | - | 87.8 | 73.3 |
| Mar 2017 | • | 235 | 88.6 | - | - | 88.5 | 73.6 |
| Apr 2017 | • | 232 | 87.4 | - | - | 89.4 | 74.0 |
| May 2017 | • | 231 | 86.9 | - | - | 90.8 | 74.0 |
| Jun 2017 | • | 240 | 90.2 | - | - | 91.6 | 74.1 |
| Jul 2017 | • | 239 | 89.8 | - | - | 90.2 | 74.2 |
| Aug 2017 | • | 238 | 89.4 | - | - | 89.8 | 74.2 |
| Sep 2017 | • | 242 | 90.8 | - | - | 90.5 | 74.2 |
| Oct 2017 | • | 231 | 86.6 | - | - | 90.7 | 74.3 |
| Nov 2017 | • | 218 | 81.7 | - | - | 89.9 | 74.5 |
| Dec 2017 | • | 221 | 82.7 | - | - | 91.1 | 74.4 |
| Jan 2018 | • | 231 | 86.4 | - | - | 91.9 | 74.4 |
| Feb 2018 | • | 241 | 90.1 | - | - | 90.0 | 74.1 |
| Mar 2018 | • | 237 | 88.5 | - | - | 88.9 | 73.9 |
| Apr 2018 | • | 245 | 91.5 | - | - | 89.7 | 74.0 |
| May 2018 | • | 243 | 90.7 | - | - | 89.9 | 74.4 |
| Jun 2018 | • | 241 | 90.0 | - | - | 89.9 | 74.7 |
| Jul 2018 | • | 249 | 92.9 | - | - | 91.6 | 74.9 |
| Aug 2018 | • | 244 | 91.0 | - | - | 91.1 | 75.2 |
| Sep 2018 | • | 244 | 91.0 | - | - | 91.4 | 75.6 |
| Oct 2018 | • | 244 | 91.0 | - | - | 90.4 | 75.9 |
| Nov 2018 | • | 248 | 92.5 | - | - | 90.3 | 75.9 |
| Dec 2018 | • | 252 | 94.0 | - | - | 90.5 | 76.1 |
| Jan 2019 | • | 243 | 90.6 | - | - | 90.6 | 76.5 |
| Feb 2019 | • | 241 | 89.8 | - | - | 91.3 | 76.8 |
| Mar 2019 | • | 256 | 95.4 | - | - | 93.8 | 77.3 |
| Apr 2019 | • | 254 | 94.7 | - | - | 93.4 | 77.6 |
| May 2019 | • | 259 | 96.5 | - | - | 93.6 | 77.8 |
| Jun 2019 | • | 263 | 98.0 | - | - | 93.2 | 77.7 |
| Jul 2019 | • | 257 | 95.8 | - | - | 91.9 | 77.8 |
| Aug 2019 | • | 262 | 97.6 | - | - | 93.7 | 78.1 |
| Sep 2019 | • | 256 | 95.4 | - | - | 93.2 | 77.9 |
| Oct 2019 | • | 264 | 98.4 | - | - | 94.4 | 77.9 |
| Nov 2019 | • | 268 | 99.9 | - | - | 95.8 | 77.9 |
| Dec 2019 | • | 262 | 97.7 | - | - | 96.2 | 77.9 |
| Jan 2020 | • | 268 | 99.9 | - | - | 96.7 | 78.1 |
| Feb 2020 | • | 266 | 98.9 | - | - | 96.3 | 78.1 |
| Mar 2020 | • | 250 | 92.9 | - | - | 93.3 | 77.0 |
| Apr 2020 | • | 242 | 90.0 | - | - | 91.5 | 75.0 |
| May 2020 | • | 235 | 87.4 | - | - | 90.3 | 73.4 |
| Jun 2020 | • | 228 | 84.9 | - | - | 89.6 | 72.4 |
| Jul 2020 | • | 228 | 84.9 | - | - | 89.4 | 71.3 |
| Aug 2020 | • | 221 | 82.3 | - | - | 86.9 | 70.2 |
| Sep 2020 | • | 219 | 81.6 | - | - | 86.0 | 69.6 |
| Oct 2020 | • | 210 | 78.3 | - | - | 84.4 | 68.6 |
| Nov 2020 | • | 202 | 75.4 | - | - | 81.8 | 67.9 |
| Dec 2020 | • | 205 | 76.5 | - | - | 80.3 | 67.2 |
| Jan 2021 | • | 194 | 72.5 | - | - | 78.8 | 65.8 |
| Feb 2021 | • | 187 | 70.1 | - | - | 77.1 | 65.0 |
| Mar 2021 | • | 195 | 73.1 | - | - | 78.7 | 65.4 |
| Apr 2021 | • | 198 | 74.2 | - | - | 80.1 | 66.8 |
| May 2021 | • | 200 | 75.0 | - | - | 80.4 | 67.3 |
| Jun 2021 | • | 193 | 72.3 | - | - | 80.9 | 67.6 |
| Jul 2021 | • | 193 | 72.3 | - | - | 80.5 | 67.8 |
| Aug 2021 | • | 199 | 74.6 | - | - | 79.9 | 67.5 |
| Sep 2021 | • | 202 | 75.7 | - | - | 80.4 | 67.3 |
| Oct 2021 | • | 206 | 77.2 | - | - | 80.0 | 66.9 |
| Nov 2021 | • | 203 | 76.0 | - | - | 80.1 | 66.9 |
| Dec 2021 | • | 197 | 73.8 | - | - | 79.8 | 66.9 |
| Jan 2022 | • | 201 | 75.3 | - | - | 78.3 | 67.3 |
| Feb 2022 | • | 202 | 75.6 | - | - | 78.0 | 67.4 |
| Mar 2022 | • | 204 | 76.4 | - | - | 76.8 | 67.1 |
| Apr 2022 | • | 207 | 77.5 | - | - | 77.5 | 66.9 |
| May 2022 | • | 207 | 77.4 | - | - | 77.2 | 66.8 |
| Jun 2022 | • | 213 | 79.6 | - | - | 76.6 | 66.7 |
| Jul 2022 | • | 211 | 78.9 | - | - | 76.1 | 66.6 |
| Aug 2022 | • | 208 | 77.7 | - | - | 76.7 | 66.8 |
| Sep 2022 | • | 211 | 78.8 | - | - | 76.8 | 67.2 |
| Oct 2022 | • | 205 | 76.5 | - | - | 78.1 | 67.5 |
| Nov 2022 | • | 212 | 79.1 | - | - | 79.0 | 67.8 |
| Dec 2022 | • | 212 | 79.0 | - | - | 80.0 | 67.5 |
| Jan 2023 | • | 214 | 79.7 | - | - | 82.3 | 67.4 |
| Feb 2023 | • | 220 | 81.9 | - | - | 83.5 | 67.7 |
| Mar 2023 | • | 214 | 79.6 | - | - | 83.3 | 67.9 |
| Apr 2023 | • | 222 | 82.6 | - | - | 82.9 | 68.1 |
| May 2023 | • | 227 | 84.5 | - | - | 83.1 | 68.6 |
| Jun 2023 | • | 232 | 86.4 | - | - | 84.7 | 69.1 |
| Jul 2023 | • | 233 | 86.7 | - | - | 85.2 | 69.8 |
| Aug 2023 | • | 233 | 86.7 | - | - | 84.3 | 70.2 |
| Sep 2023 | • | 233 | 86.8 | - | - | 84.6 | 70.4 |
| Oct 2023 | • | 246 | 91.6 | - | - | 85.7 | 71.0 |
| Nov 2023 | • | 249 | 92.7 | - | - | 86.2 | 71.2 |
| Dec 2023 | • | 251 | 93.5 | - | - | 86.7 | 72.2 |
| Jan 2024 | • | 250 | 93.1 | - | - | 87.4 | 72.9 |
| Feb 2024 | • | 262 | 97.3 | - | - | 88.7 | 73.3 |
| Mar 2024 | • | 269 | 99.9 | - | - | 89.2 | 73.8 |
| Apr 2024 | • | 263 | 97.7 | - | - | 89.4 | 74.4 |
| May 2024 | • | 255 | 94.7 | - | - | 90.3 | 74.7 |
| Jun 2024 | • | 249 | 92.5 | - | - | 90.9 | 75.1 |
| Jul 2024 | • | 262 | 97.4 | - | - | 91.7 | 75.1 |
| Aug 2024 | • | 262 | 97.4 | - | - | 93.1 | 75.5 |
| Sep 2024 | • | 257 | 95.5 | - | - | 93.1 | 75.6 |
| Oct 2024 | • | 256 | 95.2 | - | - | 91.9 | 75.9 |
| Nov 2024 | • | 254 | 94.4 | - | - | 92.2 | 76.2 |
| Dec 2024 | • | 265 | 98.5 | - | - | 92.8 | 76.3 |
| Jan 2025 | • | 267 | 99.3 | - | - | 92.3 | 76.4 |
| Feb 2025 | • | 257 | 95.8 | - | - | 92.7 | 76.4 |
| Mar 2025 | • | 247 | 92.1 | - | - | 93.2 | 76.6 |
| Apr 2025 | • | 249 | 92.9 | - | - | 93.3 | 76.7 |
| May 2025 | • | 255 | 95.1 | - | - | 93.4 | 77.0 |
| Jun 2025 | • | 268 | 100.0 | - | - | 93.7 | 77.0 |
Source: UK Health Security Agency
There is more month-to-month variability in the rate of hospital-onset cases of E. coli bacteraemia as the total number of cases are smaller. However, there is an overall slight increasing trend in the hospital-onset infection rate between 2015 and 2024. The rate has consistently been higher than England.
The number of hospital-onset cases of E. coli has tended to vary in Hull from around 15 to around 25 cases per 100,000 population with the highest value of 25.3 cases per 100,000 for the year January to December 2023. Since then the number of cases decreased to reach 17.4 cases per 100,000 population for the year December 2023 to November 2024, but has since been increasing at a relatively fast rate to reach 23.4 cases per 100,000 population for the latest period May 2024 to April 2025.
In the latest period, May 2024 to April 2025, there were 63 cases of E. coli bacteraemia in Hull that were hospital-onset. One-quarter of all E. coli cases that were laboratory confirmed were hospital-onset.
Compared with benchmark
E. coli bacteraemia 12-month rolling case counts and rates of hospital-onset, by Sub ICB Location (SICBL) and month (Persons All ages)
|
Period
|
Humber and North Yorkshire ICB - 03F |
NHS Humber and North Yorkshire Integrated Care Board - QOQ
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| Dec 2014 | • | 43 | 16.5 | - | - | 18.5 | 13.6 |
| Jan 2015 | • | 46 | 17.6 | - | - | 18.2 | 13.6 |
| Feb 2015 | • | 46 | 17.6 | - | - | 18.0 | 13.5 |
| Mar 2015 | • | 43 | 16.5 | - | - | 17.7 | 13.5 |
| Apr 2015 | • | 43 | 16.4 | - | - | 17.0 | 13.6 |
| May 2015 | • | 45 | 17.2 | - | - | 16.6 | 13.5 |
| Jun 2015 | • | 49 | 18.7 | - | - | 17.5 | 13.6 |
| Jul 2015 | • | 48 | 18.3 | - | - | 16.6 | 13.6 |
| Aug 2015 | • | 49 | 18.7 | - | - | 16.7 | 13.7 |
| Sep 2015 | • | 51 | 19.4 | - | - | 16.8 | 13.8 |
| Oct 2015 | • | 53 | 20.2 | - | - | 17.3 | 13.9 |
| Nov 2015 | • | 56 | 21.3 | - | - | 16.8 | 14.0 |
| Dec 2015 | • | 56 | 21.3 | - | - | 16.6 | 13.9 |
| Jan 2016 | • | 56 | 21.3 | - | - | 16.6 | 14.0 |
| Feb 2016 | • | 55 | 20.9 | - | - | 17.4 | 14.0 |
| Mar 2016 | • | 55 | 20.8 | - | - | 17.2 | 14.1 |
| Apr 2016 | • | 54 | 20.4 | - | - | 17.1 | 14.0 |
| May 2016 | • | 55 | 20.8 | - | - | 17.1 | 14.1 |
| Jun 2016 | • | 53 | 20.0 | - | - | 16.9 | 14.3 |
| Jul 2016 | • | 52 | 19.7 | - | - | 17.3 | 14.4 |
| Aug 2016 | • | 46 | 17.4 | - | - | 17.5 | 14.4 |
| Sep 2016 | • | 41 | 15.5 | - | - | 17.5 | 14.4 |
| Oct 2016 | • | 39 | 14.7 | - | - | 16.9 | 14.3 |
| Nov 2016 | • | 39 | 14.7 | - | - | 17.4 | 14.3 |
| Dec 2016 | • | 41 | 15.4 | - | - | 17.3 | 14.3 |
| Jan 2017 | • | 40 | 15.1 | - | - | 16.9 | 14.3 |
| Feb 2017 | • | 39 | 14.7 | - | - | 16.9 | 14.3 |
| Mar 2017 | • | 39 | 14.7 | - | - | 16.8 | 14.3 |
| Apr 2017 | • | 40 | 15.1 | - | - | 16.8 | 14.3 |
| May 2017 | • | 35 | 13.2 | - | - | 16.8 | 14.3 |
| Jun 2017 | • | 38 | 14.3 | - | - | 17.1 | 14.2 |
| Jul 2017 | • | 39 | 14.7 | - | - | 16.8 | 14.1 |
| Aug 2017 | • | 44 | 16.5 | - | - | 16.4 | 14.0 |
| Sep 2017 | • | 47 | 17.6 | - | - | 16.3 | 14.1 |
| Oct 2017 | • | 46 | 17.2 | - | - | 16.6 | 14.0 |
| Nov 2017 | • | 45 | 16.9 | - | - | 16.7 | 14.1 |
| Dec 2017 | • | 43 | 16.1 | - | - | 17.0 | 14.0 |
| Jan 2018 | • | 48 | 18.0 | - | - | 17.5 | 14.0 |
| Feb 2018 | • | 52 | 19.4 | - | - | 16.6 | 13.9 |
| Mar 2018 | • | 52 | 19.4 | - | - | 17.0 | 13.8 |
| Apr 2018 | • | 54 | 20.2 | - | - | 17.5 | 13.8 |
| May 2018 | • | 57 | 21.3 | - | - | 17.3 | 13.7 |
| Jun 2018 | • | 57 | 21.3 | - | - | 16.8 | 13.7 |
| Jul 2018 | • | 60 | 22.4 | - | - | 17.2 | 13.6 |
| Aug 2018 | • | 58 | 21.6 | - | - | 17.5 | 13.7 |
| Sep 2018 | • | 55 | 20.5 | - | - | 17.3 | 13.7 |
| Oct 2018 | • | 52 | 19.4 | - | - | 16.8 | 13.6 |
| Nov 2018 | • | 51 | 19.0 | - | - | 16.4 | 13.6 |
| Dec 2018 | • | 53 | 19.8 | - | - | 16.9 | 13.6 |
| Jan 2019 | • | 47 | 17.5 | - | - | 16.4 | 13.6 |
| Feb 2019 | • | 43 | 16.0 | - | - | 17.0 | 13.5 |
| Mar 2019 | • | 50 | 18.6 | - | - | 17.4 | 13.6 |
| Apr 2019 | • | 51 | 19.0 | - | - | 17.2 | 13.6 |
| May 2019 | • | 48 | 17.9 | - | - | 17.4 | 13.7 |
| Jun 2019 | • | 47 | 17.5 | - | - | 17.0 | 13.6 |
| Jul 2019 | • | 42 | 15.7 | - | - | 16.7 | 13.7 |
| Aug 2019 | • | 43 | 16.0 | - | - | 16.7 | 13.7 |
| Sep 2019 | • | 51 | 19.0 | - | - | 17.2 | 13.7 |
| Oct 2019 | • | 56 | 20.9 | - | - | 17.4 | 13.8 |
| Nov 2019 | • | 58 | 21.6 | - | - | 17.7 | 13.8 |
| Dec 2019 | • | 56 | 20.9 | - | - | 17.0 | 13.9 |
| Jan 2020 | • | 57 | 21.2 | - | - | 17.8 | 14.0 |
| Feb 2020 | • | 57 | 21.2 | - | - | 17.3 | 14.0 |
| Mar 2020 | • | 52 | 19.3 | - | - | 17.3 | 13.9 |
| Apr 2020 | • | 47 | 17.5 | - | - | 16.8 | 13.5 |
| May 2020 | • | 50 | 18.6 | - | - | 16.4 | 13.0 |
| Jun 2020 | • | 48 | 17.9 | - | - | 16.2 | 12.9 |
| Jul 2020 | • | 50 | 18.6 | - | - | 16.6 | 12.6 |
| Aug 2020 | • | 53 | 19.7 | - | - | 16.4 | 12.4 |
| Sep 2020 | • | 48 | 17.9 | - | - | 15.7 | 12.2 |
| Oct 2020 | • | 48 | 17.9 | - | - | 15.6 | 12.0 |
| Nov 2020 | • | 45 | 16.8 | - | - | 14.9 | 11.9 |
| Dec 2020 | • | 47 | 17.5 | - | - | 14.4 | 11.8 |
| Jan 2021 | • | 48 | 17.9 | - | - | 13.9 | 11.7 |
| Feb 2021 | • | 48 | 18.0 | - | - | 13.5 | 11.6 |
| Mar 2021 | • | 51 | 19.1 | - | - | 13.2 | 11.6 |
| Apr 2021 | • | 54 | 20.2 | - | - | 13.5 | 11.8 |
| May 2021 | • | 52 | 19.5 | - | - | 13.3 | 12.0 |
| Jun 2021 | • | 52 | 19.5 | - | - | 13.8 | 12.1 |
| Jul 2021 | • | 53 | 19.9 | - | - | 13.4 | 12.2 |
| Aug 2021 | • | 52 | 19.5 | - | - | 13.5 | 12.3 |
| Sep 2021 | • | 51 | 19.1 | - | - | 14.0 | 12.4 |
| Oct 2021 | • | 52 | 19.5 | - | - | 14.4 | 12.3 |
| Nov 2021 | • | 53 | 19.9 | - | - | 14.5 | 12.4 |
| Dec 2021 | • | 51 | 19.1 | - | - | 14.6 | 12.5 |
| Jan 2022 | • | 50 | 18.7 | - | - | 14.2 | 12.5 |
| Feb 2022 | • | 52 | 19.5 | - | - | 14.5 | 12.5 |
| Mar 2022 | • | 48 | 18.0 | - | - | 14.1 | 12.5 |
| Apr 2022 | • | 48 | 18.0 | - | - | 14.3 | 12.7 |
| May 2022 | • | 50 | 18.7 | - | - | 14.5 | 12.8 |
| Jun 2022 | • | 54 | 20.2 | - | - | 15.1 | 12.9 |
| Jul 2022 | • | 53 | 19.8 | - | - | 15.2 | 13.1 |
| Aug 2022 | • | 53 | 19.8 | - | - | 15.3 | 13.2 |
| Sep 2022 | • | 55 | 20.5 | - | - | 15.2 | 13.3 |
| Oct 2022 | • | 50 | 18.7 | - | - | 15.0 | 13.5 |
| Nov 2022 | • | 50 | 18.6 | - | - | 14.9 | 13.5 |
| Dec 2022 | • | 51 | 19.0 | - | - | 15.5 | 13.6 |
| Jan 2023 | • | 54 | 20.1 | - | - | 15.8 | 13.6 |
| Feb 2023 | • | 55 | 20.5 | - | - | 15.9 | 13.7 |
| Mar 2023 | • | 57 | 21.2 | - | - | 16.6 | 13.8 |
| Apr 2023 | • | 59 | 22.0 | - | - | 16.9 | 13.9 |
| May 2023 | • | 56 | 20.8 | - | - | 16.9 | 14.1 |
| Jun 2023 | • | 57 | 21.2 | - | - | 16.5 | 14.0 |
| Jul 2023 | • | 57 | 21.2 | - | - | 16.1 | 14.1 |
| Aug 2023 | • | 54 | 20.1 | - | - | 15.8 | 14.0 |
| Sep 2023 | • | 54 | 20.1 | - | - | 15.7 | 14.0 |
| Oct 2023 | • | 63 | 23.5 | - | - | 15.9 | 14.0 |
| Nov 2023 | • | 66 | 24.6 | - | - | 16.6 | 14.1 |
| Dec 2023 | • | 68 | 25.3 | - | - | 16.2 | 14.1 |
| Jan 2024 | • | 63 | 23.5 | - | - | 16.2 | 14.1 |
| Feb 2024 | • | 62 | 23.0 | - | - | 16.0 | 14.2 |
| Mar 2024 | • | 61 | 22.7 | - | - | 15.6 | 14.3 |
| Apr 2024 | • | 60 | 22.3 | - | - | 15.6 | 14.4 |
| May 2024 | • | 62 | 23.0 | - | - | 16.4 | 14.4 |
| Jun 2024 | • | 57 | 21.2 | - | - | 16.4 | 14.3 |
| Jul 2024 | • | 56 | 20.8 | - | - | 16.7 | 14.3 |
| Aug 2024 | • | 56 | 20.8 | - | - | 16.6 | 14.5 |
| Sep 2024 | • | 53 | 19.7 | - | - | 17.0 | 14.5 |
| Oct 2024 | • | 50 | 18.6 | - | - | 16.6 | 14.6 |
| Nov 2024 | • | 47 | 17.5 | - | - | 16.6 | 14.5 |
| Dec 2024 | • | 53 | 19.7 | - | - | 17.0 | 14.5 |
| Jan 2025 | • | 53 | 19.7 | - | - | 17.1 | 14.7 |
| Feb 2025 | • | 59 | 22.0 | - | - | 18.1 | 14.7 |
| Mar 2025 | • | 59 | 22.0 | - | - | 18.4 | 14.7 |
| Apr 2025 | • | 63 | 23.5 | - | - | 18.7 | 14.7 |
| May 2025 | • | 65 | 24.2 | - | - | 18.0 | 14.7 |
| Jun 2025 | • | 71 | 26.5 | - | - | 18.3 | 14.7 |
Source: UK Health Security Agency
The rate of community-onset cases of E. coli has been consistently higher than the rate of hospital-onset cases, and with the majority of the cases having community-onset.
Between 2015 and 2025, the rate has varied from around 50 to just over 80 cases per 100,000 population. The rate increased from 2014 to 2019 reaching a peak of 84 cases per 100,000 population for the year September 2018 to August 2019. The rate remained around 80 cases per 100,000 population for the next few months, but fell sharply during the COVID-19 pandemic (lockdown commenced March 2020) to reach a low of 53 cases per 100,000 population for the year August 2020 to July 2021. Since then the rate has increased but at a gradual rate almost reaching the peak previously observed (for September 2018 to August 2019) with 79 cases per 100,000 population for the year February 2024 to January 2025. The rate has decreased slightly in the last couple of months with the latest rate being 69 cases per 100,000 population for the period May 2024 to April 2025.
In the latest period, May 2024 to April 2025, there were 186 cases of E. coli bacteraemia in Hull that were community-onset. Three-quarters of all E. coli cases that were laboratory confirmed were community-onset.
Compared with benchmark
E. coli bacteraemia 12-month rolling case counts and rates of community-onset, by Sub ICB Location (SICBL) and month (Persons All ages)
|
Period
|
Humber and North Yorkshire ICB - 03F |
NHS Humber and North Yorkshire Integrated Care Board - QOQ
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| Dec 2014 | • | 159 | 60.9 | - | - | 60.5 | 52.0 |
| Jan 2015 | • | 146 | 55.9 | - | - | 60.1 | 52.0 |
| Feb 2015 | • | 142 | 54.4 | - | - | 60.2 | 52.2 |
| Mar 2015 | • | 136 | 52.0 | - | - | 60.4 | 52.2 |
| Apr 2015 | • | 136 | 52.0 | - | - | 60.9 | 52.3 |
| May 2015 | • | 139 | 53.1 | - | - | 61.3 | 52.3 |
| Jun 2015 | • | 139 | 53.1 | - | - | 61.8 | 52.5 |
| Jul 2015 | • | 137 | 52.3 | - | - | 62.3 | 52.8 |
| Aug 2015 | • | 133 | 50.7 | - | - | 61.0 | 52.9 |
| Sep 2015 | • | 133 | 50.7 | - | - | 61.2 | 53.4 |
| Oct 2015 | • | 139 | 53.0 | - | - | 62.2 | 53.6 |
| Nov 2015 | • | 144 | 54.8 | - | - | 62.1 | 54.0 |
| Dec 2015 | • | 149 | 56.7 | - | - | 61.5 | 54.3 |
| Jan 2016 | • | 158 | 60.1 | - | - | 63.0 | 54.9 |
| Feb 2016 | • | 153 | 58.0 | - | - | 63.1 | 55.1 |
| Mar 2016 | • | 155 | 58.7 | - | - | 63.9 | 55.5 |
| Apr 2016 | • | 164 | 62.1 | - | - | 64.0 | 55.8 |
| May 2016 | • | 163 | 61.7 | - | - | 63.1 | 56.2 |
| Jun 2016 | • | 165 | 62.4 | - | - | 63.4 | 56.4 |
| Jul 2016 | • | 166 | 62.7 | - | - | 65.3 | 56.8 |
| Aug 2016 | • | 179 | 67.6 | - | - | 68.0 | 57.4 |
| Sep 2016 | • | 185 | 69.8 | - | - | 68.7 | 57.6 |
| Oct 2016 | • | 189 | 71.3 | - | - | 69.2 | 58.1 |
| Nov 2016 | • | 196 | 73.9 | - | - | 70.2 | 58.4 |
| Dec 2016 | • | 192 | 72.3 | - | - | 69.6 | 58.6 |
| Jan 2017 | • | 192 | 72.3 | - | - | 69.2 | 58.5 |
| Feb 2017 | • | 192 | 72.4 | - | - | 70.9 | 59.0 |
| Mar 2017 | • | 196 | 73.9 | - | - | 71.7 | 59.3 |
| Apr 2017 | • | 192 | 72.3 | - | - | 72.6 | 59.7 |
| May 2017 | • | 196 | 73.8 | - | - | 74.1 | 59.7 |
| Jun 2017 | • | 202 | 76.0 | - | - | 74.5 | 59.9 |
| Jul 2017 | • | 200 | 75.1 | - | - | 73.4 | 60.1 |
| Aug 2017 | • | 194 | 72.8 | - | - | 73.4 | 60.2 |
| Sep 2017 | • | 195 | 73.2 | - | - | 74.2 | 60.2 |
| Oct 2017 | • | 185 | 69.4 | - | - | 74.1 | 60.3 |
| Nov 2017 | • | 173 | 64.8 | - | - | 73.1 | 60.4 |
| Dec 2017 | • | 178 | 66.6 | - | - | 74.1 | 60.4 |
| Jan 2018 | • | 183 | 68.5 | - | - | 74.4 | 60.4 |
| Feb 2018 | • | 189 | 70.6 | - | - | 73.4 | 60.2 |
| Mar 2018 | • | 185 | 69.1 | - | - | 71.9 | 60.1 |
| Apr 2018 | • | 191 | 71.3 | - | - | 72.3 | 60.1 |
| May 2018 | • | 186 | 69.4 | - | - | 72.5 | 60.7 |
| Jun 2018 | • | 184 | 68.7 | - | - | 73.1 | 61.0 |
| Jul 2018 | • | 189 | 70.5 | - | - | 74.4 | 61.2 |
| Aug 2018 | • | 186 | 69.4 | - | - | 73.6 | 61.5 |
| Sep 2018 | • | 189 | 70.5 | - | - | 74.0 | 61.9 |
| Oct 2018 | • | 192 | 71.6 | - | - | 73.6 | 62.3 |
| Nov 2018 | • | 197 | 73.5 | - | - | 73.9 | 62.3 |
| Dec 2018 | • | 199 | 74.2 | - | - | 73.6 | 62.5 |
| Jan 2019 | • | 196 | 73.1 | - | - | 74.1 | 63.0 |
| Feb 2019 | • | 198 | 73.8 | - | - | 74.3 | 63.3 |
| Mar 2019 | • | 206 | 76.8 | - | - | 76.4 | 63.7 |
| Apr 2019 | • | 203 | 75.6 | - | - | 76.2 | 64.0 |
| May 2019 | • | 211 | 78.6 | - | - | 76.2 | 64.1 |
| Jun 2019 | • | 216 | 80.5 | - | - | 76.2 | 64.0 |
| Jul 2019 | • | 215 | 80.1 | - | - | 75.2 | 64.1 |
| Aug 2019 | • | 219 | 81.6 | - | - | 77.0 | 64.4 |
| Sep 2019 | • | 205 | 76.4 | - | - | 76.0 | 64.2 |
| Oct 2019 | • | 208 | 77.5 | - | - | 77.0 | 64.1 |
| Nov 2019 | • | 210 | 78.3 | - | - | 78.0 | 64.0 |
| Dec 2019 | • | 206 | 76.8 | - | - | 79.1 | 64.0 |
| Jan 2020 | • | 211 | 78.6 | - | - | 79.0 | 64.1 |
| Feb 2020 | • | 209 | 77.7 | - | - | 79.0 | 64.0 |
| Mar 2020 | • | 198 | 73.6 | - | - | 76.0 | 63.1 |
| Apr 2020 | • | 195 | 72.5 | - | - | 74.7 | 61.5 |
| May 2020 | • | 185 | 68.8 | - | - | 74.0 | 60.4 |
| Jun 2020 | • | 180 | 67.0 | - | - | 73.4 | 59.6 |
| Jul 2020 | • | 178 | 66.3 | - | - | 72.9 | 58.8 |
| Aug 2020 | • | 168 | 62.6 | - | - | 70.4 | 57.9 |
| Sep 2020 | • | 171 | 63.7 | - | - | 70.2 | 57.4 |
| Oct 2020 | • | 162 | 60.4 | - | - | 68.8 | 56.6 |
| Nov 2020 | • | 157 | 58.6 | - | - | 66.9 | 56.0 |
| Dec 2020 | • | 158 | 59.0 | - | - | 65.8 | 55.3 |
| Jan 2021 | • | 146 | 54.5 | - | - | 64.9 | 54.1 |
| Feb 2021 | • | 139 | 52.1 | - | - | 63.6 | 53.4 |
| Mar 2021 | • | 144 | 54.0 | - | - | 65.4 | 53.8 |
| Apr 2021 | • | 144 | 54.0 | - | - | 66.5 | 54.9 |
| May 2021 | • | 148 | 55.5 | - | - | 67.1 | 55.3 |
| Jun 2021 | • | 141 | 52.8 | - | - | 67.1 | 55.6 |
| Jul 2021 | • | 140 | 52.5 | - | - | 67.1 | 55.6 |
| Aug 2021 | • | 147 | 55.1 | - | - | 66.4 | 55.2 |
| Sep 2021 | • | 151 | 56.6 | - | - | 66.5 | 54.9 |
| Oct 2021 | • | 154 | 57.7 | - | - | 65.6 | 54.6 |
| Nov 2021 | • | 150 | 56.2 | - | - | 65.6 | 54.5 |
| Dec 2021 | • | 146 | 54.7 | - | - | 65.1 | 54.4 |
| Jan 2022 | • | 151 | 56.6 | - | - | 64.1 | 54.8 |
| Feb 2022 | • | 150 | 56.2 | - | - | 63.5 | 54.9 |
| Mar 2022 | • | 156 | 58.4 | - | - | 62.8 | 54.6 |
| Apr 2022 | • | 159 | 59.5 | - | - | 63.1 | 54.3 |
| May 2022 | • | 157 | 58.7 | - | - | 62.7 | 54.1 |
| Jun 2022 | • | 159 | 59.4 | - | - | 61.5 | 53.8 |
| Jul 2022 | • | 158 | 59.0 | - | - | 60.9 | 53.5 |
| Aug 2022 | • | 155 | 57.9 | - | - | 61.4 | 53.6 |
| Sep 2022 | • | 156 | 58.2 | - | - | 61.6 | 53.9 |
| Oct 2022 | • | 155 | 57.8 | - | - | 63.1 | 54.0 |
| Nov 2022 | • | 162 | 60.4 | - | - | 64.1 | 54.2 |
| Dec 2022 | • | 161 | 60.0 | - | - | 64.5 | 53.9 |
| Jan 2023 | • | 160 | 59.6 | - | - | 66.4 | 53.8 |
| Feb 2023 | • | 165 | 61.4 | - | - | 67.5 | 53.9 |
| Mar 2023 | • | 157 | 58.4 | - | - | 66.7 | 54.1 |
| Apr 2023 | • | 163 | 60.7 | - | - | 66.0 | 54.2 |
| May 2023 | • | 171 | 63.7 | - | - | 66.1 | 54.5 |
| Jun 2023 | • | 175 | 65.1 | - | - | 68.2 | 55.0 |
| Jul 2023 | • | 176 | 65.5 | - | - | 69.1 | 55.7 |
| Aug 2023 | • | 179 | 66.6 | - | - | 68.5 | 56.2 |
| Sep 2023 | • | 179 | 66.6 | - | - | 69.0 | 56.4 |
| Oct 2023 | • | 183 | 68.1 | - | - | 69.8 | 57.0 |
| Nov 2023 | • | 183 | 68.1 | - | - | 69.6 | 57.1 |
| Dec 2023 | • | 183 | 68.1 | - | - | 70.6 | 58.1 |
| Jan 2024 | • | 187 | 69.6 | - | - | 71.3 | 58.8 |
| Feb 2024 | • | 200 | 74.3 | - | - | 72.7 | 59.1 |
| Mar 2024 | • | 208 | 77.3 | - | - | 73.6 | 59.5 |
| Apr 2024 | • | 203 | 75.4 | - | - | 73.9 | 60.0 |
| May 2024 | • | 193 | 71.7 | - | - | 73.9 | 60.4 |
| Jun 2024 | • | 192 | 71.3 | - | - | 74.4 | 60.7 |
| Jul 2024 | • | 206 | 76.5 | - | - | 75.0 | 60.8 |
| Aug 2024 | • | 206 | 76.6 | - | - | 76.5 | 61.1 |
| Sep 2024 | • | 204 | 75.8 | - | - | 76.1 | 61.1 |
| Oct 2024 | • | 206 | 76.6 | - | - | 75.4 | 61.4 |
| Nov 2024 | • | 207 | 77.0 | - | - | 75.6 | 61.7 |
| Dec 2024 | • | 212 | 78.8 | - | - | 75.8 | 61.8 |
| Jan 2025 | • | 214 | 79.6 | - | - | 75.1 | 61.8 |
| Feb 2025 | • | 198 | 73.8 | - | - | 74.6 | 61.7 |
| Mar 2025 | • | 188 | 70.1 | - | - | 74.8 | 61.8 |
| Apr 2025 | • | 186 | 69.4 | - | - | 74.6 | 62.0 |
| May 2025 | • | 190 | 70.9 | - | - | 75.4 | 62.3 |
| Jun 2025 | • | 197 | 73.5 | - | - | 75.4 | 62.3 |
Source: UK Health Security Agency
MRSA (Methicillin-Resistant Staphylococcus Aureus)
The number of laboratory confirmed cases of MRSA are very low, and this impacts on trends over time and national comparisons as an increase of only one or two cases within the year can make a relatively large difference to the infection rate per 100,000 population. See Small Numbers within the Glossary for more information.
Cases by Financial Year
The number of laboratory confirmed cases of MRSA is given below for Hull (03F) over a financial year compared to the others within the Humber and North Yorkshire Integrated Care Board, as well as the rate based on those that were community-onset. The rates are given as the number of cases over the year per 100,000 population.
For 2023/24, the number of cases of MRSA was very low with 1.1 cases per 100,000 population over the year in Hull. There were no community-onset cases of MRSA.
The infection rate in Hull is lower than England.
Compared with benchmark
| Indicator | Period | England | NHS Humber and North Yorkshire Integrated Care Board - QOQ | Humber and North Yorkshire ICB - 02Y | Humber and North Yorkshire ICB - 03F | Humber and North Yorkshire ICB - 03H | Humber and North Yorkshire ICB - 03K | Humber and North Yorkshire ICB - 03Q | Humber and North Yorkshire ICB - 42D |
|---|---|---|---|---|---|---|---|---|---|
MRSA bacteraemia case counts and rates by sub ICB location (SICBL) and financial year (Persons All ages) | 2023/24 | 1.6 | 0.9 | 0.6 | 1.1 | 0.6 | 1.2 | 0.8 | 0.9 |
MRSA bacteraemia case counts and rates of community-onset, by sub ICB location (SICBL) and financial year (Persons All ages) | 2023/24 | 1.0 | 0.3 | 0.3 | 0.0 | 0.0 | 0.0 | 0.5 | 0.7 |
| Indicator | Period | England | NHS Humber and North Yorkshire Integrated Care Board - QOQ | Humber and North Yorkshire ICB - 02Y | Humber and North Yorkshire ICB - 03F | Humber and North Yorkshire ICB - 03H | Humber and North Yorkshire ICB - 03K | Humber and North Yorkshire ICB - 03Q | Humber and North Yorkshire ICB - 42D |
|---|---|---|---|---|---|---|---|---|---|
MRSA bacteraemia case counts and rates by sub ICB location (SICBL) and financial year (Persons All ages) | 2023/24 | 1.6 | 0.9 | 0.6 | 1.1 | 0.6 | 1.2 | 0.8 | 0.9 |
MRSA bacteraemia case counts and rates of community-onset, by sub ICB location (SICBL) and financial year (Persons All ages) | 2023/24 | 1.0 | 0.3 | 0.3 | 0.0 | 0.0 | 0.0 | 0.5 | 0.7 |
In 2009/10 and 2010/11 there were 12 and 16 cases of MRSA in Hull respectively, but since then the numbers have been much smaller with most years having only one or two cases in total. The exceptions were 2011/12 when there were five cases, and recently in 2021/22 and 2022/23 when there have been four cases of MRSA in Hull.
In the latest year 2023/24, there have been only three cases in Hull.
Compared with benchmark
MRSA bacteraemia case counts and rates by sub ICB location (SICBL) and financial year (Persons All ages)
|
Period
|
Humber and North Yorkshire ICB - 03F |
NHS Humber and North Yorkshire Integrated Care Board - QOQ
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2009/10 | • | 12 | 4.7 | - | - | 4.2 | 3.6 |
| 2010/11 | • | 16 | 6.2 | - | - | 3.7 | 2.8 |
| 2011/12 | • | 5 | 1.9 | - | - | 2.2 | 2.1 |
| 2012/13 | • | 1 | 0.4 | - | - | 1.7 | 1.7 |
| 2013/14 | • | 2 | 0.8 | - | - | 2.2 | 1.6 |
| 2014/15 | • | 2 | 0.8 | - | - | 1.4 | 1.5 |
| 2015/16 | • | 2 | 0.8 | - | - | 1.0 | 1.5 |
| 2016/17 | • | 1 | 0.4 | - | - | 1.2 | 1.5 |
| 2017/18 | • | 2 | 0.8 | - | - | 1.4 | 1.5 |
| 2018/19 | • | 2 | 0.8 | - | - | 1.5 | 1.4 |
| 2019/20 | • | 2 | 0.8 | - | - | 1.0 | 1.4 |
| 2020/21 | • | 1 | 0.4 | - | - | 0.4 | 1.2 |
| 2021/22 | • | 4 | 1.5 | - | - | 0.9 | 1.2 |
| 2022/23 | • | 4 | 1.5 | - | - | 1.1 | 1.4 |
| 2023/24 | • | 3 | 1.1 | - | - | 0.9 | 1.6 |
Source: UK Health Security Agency
Since 2012/13, there has been zero, one or two cases of community-onset MRSA each year in Hull with the exception being 2021/22 when there were four cases of community-onset MRSA in Hull. There were no cases of community-onset MRSA in Hull for the latest year 2023/24.
Compared with benchmark
MRSA bacteraemia case counts and rates of community-onset, by sub ICB location (SICBL) and financial year (Persons All ages)
|
Period
|
Humber and North Yorkshire ICB - 03F |
NHS Humber and North Yorkshire Integrated Care Board - QOQ
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2012/13 | • | 1 | 0.4 | - | - | 1.0 | 1.0 |
| 2013/14 | • | 1 | 0.4 | - | - | 1.6 | 0.9 |
| 2014/15 | • | 2 | 0.8 | - | - | 1.1 | 0.9 |
| 2015/16 | • | 1 | 0.4 | - | - | 0.5 | 1.0 |
| 2016/17 | • | 1 | 0.4 | - | - | 0.5 | 0.9 |
| 2017/18 | • | 2 | 0.8 | - | - | 1.0 | 1.0 |
| 2018/19 | • | - | 0.0 | - | - | 1.1 | 1.0 |
| 2019/20 | • | 1 | 0.4 | - | - | 0.6 | 1.0 |
| 2020/21 | • | 1 | 0.4 | - | - | 0.3 | 0.7 |
| 2021/22 | • | 4 | 1.5 | - | - | 0.7 | 0.8 |
| 2022/23 | • | - | 0.0 | - | - | 0.6 | 0.9 |
| 2023/24 | • | - | 0.0 | - | - | 0.3 | 1.0 |
Source: UK Health Security Agency
Cases by Month (12-Month Rolling Total)
The 12-month rolling total count of the number of laboratory confirmed cases of MRSA for September 2024 is lower in Hull (03F) compared to England. The hospital-onset rate is the same or almost the same in Hull as England. However, the numbers are very small with fewer than two cases per 100,000 population. This means that there is likely considerable month-to-month variability.
The rates are also given separately for hospital-onset or community-onset infections.
Compared with benchmark
| Indicator | Period | England | NHS Humber and North Yorkshire Integrated Care Board - QOQ | Humber and North Yorkshire ICB - 02Y | Humber and North Yorkshire ICB - 03F | Humber and North Yorkshire ICB - 03H | Humber and North Yorkshire ICB - 03K | Humber and North Yorkshire ICB - 03Q | Humber and North Yorkshire ICB - 42D |
|---|---|---|---|---|---|---|---|---|---|
MRSA bacteraemia 12-month rolling case counts and rates, by Sub ICB Location (SICBL) and month (Persons All ages) | Jun 2025 | 1.9 | 1.6 | 2.8 | 1.5 | 0.6 | 1.8 | 1.4 | 1.4 |
MRSA bacteraemia 12-month rolling case counts and rates of hospital-onset, by Sub ICB Location (SICBL) and month (Persons All ages) | Jun 2025 | 0.6 | 0.8 | 2.2 | 0.7 | 0.6 | 1.2 | 0.6 | 0.0 |
MRSA bacteraemia 12-month rolling case counts and rates of community-onset, by Sub ICB Location (SICBL) and month (Persons All ages) | Jun 2025 | 1.3 | 0.8 | 0.6 | 0.7 | 0.0 | 0.6 | 0.8 | 1.4 |
| Indicator | Period | England | NHS Humber and North Yorkshire Integrated Care Board - QOQ | Humber and North Yorkshire ICB - 02Y | Humber and North Yorkshire ICB - 03F | Humber and North Yorkshire ICB - 03H | Humber and North Yorkshire ICB - 03K | Humber and North Yorkshire ICB - 03Q | Humber and North Yorkshire ICB - 42D |
|---|---|---|---|---|---|---|---|---|---|
MRSA bacteraemia 12-month rolling case counts and rates, by Sub ICB Location (SICBL) and month (Persons All ages) | Jun 2025 | 1.9 | 1.6 | 2.8 | 1.5 | 0.6 | 1.8 | 1.4 | 1.4 |
MRSA bacteraemia 12-month rolling case counts and rates of hospital-onset, by Sub ICB Location (SICBL) and month (Persons All ages) | Jun 2025 | 0.6 | 0.8 | 2.2 | 0.7 | 0.6 | 1.2 | 0.6 | 0.0 |
MRSA bacteraemia 12-month rolling case counts and rates of community-onset, by Sub ICB Location (SICBL) and month (Persons All ages) | Jun 2025 | 1.3 | 0.8 | 0.6 | 0.7 | 0.0 | 0.6 | 0.8 | 1.4 |
The number of MRSA cases in Hull is very low. Examining the 12- monthly rolling figures, from 2015 to April 2024, there were between zero and six cases of of MRSA each year (as the figures are given as a 12-month rolling average). There were no cases of MRSA at all in Hull during the 16-month period July 2016 to October 2017.
With the figures quoted as 12-month rolling count and averages, it does mean that a new case will remain in the ‘count’ for a whole 12 month period. For instance, there were three cases in Hull for the year November 2017 to October 2018, and these occurred in November 2017, March 2018 and October 2018 (as the counts increased by one for each of these months). In the year prior to this covering the period, November 2016 to October 2017, there had been no cases in the previous 12 months in Hull. There were two cases in the year December 2017 to November 2018 and these occurred during November 2017 and March 2018 (the case in November 2017 was more than a year ago so dropped out of the 12-month rolling count). There was a new case in January 2019 which increased the annual count to three again.
There were no cases of hospital-onset MRSA cases between May 2016 and September 2018, with one case in October 2018 and another case in January 2019. A further case occurred in March 2020 with the next case occurring in April 2022 with a small number of new cases over the next few months so the annual count reached six for three months in 2022. The number of cases reduced to around three in the last 12 months in early 2024 with three or four cases in the last 12 months between the period September 2022 to August 2023 and the period April 2024 to March 2025, but a new case in April 2025 means that the latest 12 month rolling average number of cases is five for the year May 2024 to April 2025. Whilst it is difficult to determine if there were new cases between May 2024 and November 2024 (as there could have been a new case but a reduction with the oldest month falling out of the period), it does appear that there were no new cases. This means that the number of cases for the next period June 2024 to May 2025 is likely to reduce back to four cases again.
The number of cases are very small in Hull so there is month-on-month variability (see Small Numbers), and it is important to note with the 12 month rolling average number of cases being presented that the same case will appear in the count for 12 whole months.
Compared with benchmark
MRSA bacteraemia 12-month rolling case counts and rates, by Sub ICB Location (SICBL) and month (Persons All ages)
|
Period
|
Humber and North Yorkshire ICB - 03F |
NHS Humber and North Yorkshire Integrated Care Board - QOQ
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| Dec 2014 | • | 2 | 0.8 | - | - | 1.2 | 1.4 |
| Jan 2015 | • | 2 | 0.8 | - | - | 1.3 | 1.5 |
| Feb 2015 | • | 2 | 0.8 | - | - | 1.3 | 1.5 |
| Mar 2015 | • | 2 | 0.8 | - | - | 1.4 | 1.5 |
| Apr 2015 | • | 1 | 0.4 | - | - | 1.5 | 1.5 |
| May 2015 | • | 2 | 0.8 | - | - | 1.7 | 1.5 |
| Jun 2015 | • | 3 | 1.1 | - | - | 1.7 | 1.5 |
| Jul 2015 | • | 3 | 1.1 | - | - | 1.7 | 1.5 |
| Aug 2015 | • | 3 | 1.1 | - | - | 1.7 | 1.6 |
| Sep 2015 | • | 3 | 1.1 | - | - | 1.8 | 1.6 |
| Oct 2015 | • | 2 | 0.8 | - | - | 1.6 | 1.6 |
| Nov 2015 | • | 2 | 0.8 | - | - | 1.6 | 1.6 |
| Dec 2015 | • | 2 | 0.8 | - | - | 1.5 | 1.5 |
| Jan 2016 | • | 2 | 0.8 | - | - | 1.5 | 1.5 |
| Feb 2016 | • | 2 | 0.8 | - | - | 1.3 | 1.5 |
| Mar 2016 | • | 2 | 0.8 | - | - | 1.0 | 1.5 |
| Apr 2016 | • | 2 | 0.8 | - | - | 0.8 | 1.5 |
| May 2016 | • | 1 | 0.4 | - | - | 0.6 | 1.5 |
| Jun 2016 | • | 1 | 0.4 | - | - | 0.5 | 1.5 |
| Jul 2016 | • | 1 | 0.4 | - | - | 0.4 | 1.5 |
| Aug 2016 | • | 1 | 0.4 | - | - | 0.6 | 1.5 |
| Sep 2016 | • | 1 | 0.4 | - | - | 0.6 | 1.5 |
| Oct 2016 | • | 1 | 0.4 | - | - | 0.8 | 1.4 |
| Nov 2016 | • | 1 | 0.4 | - | - | 0.9 | 1.4 |
| Dec 2016 | • | 1 | 0.4 | - | - | 1.0 | 1.4 |
| Jan 2017 | • | 1 | 0.4 | - | - | 1.1 | 1.5 |
| Feb 2017 | • | 1 | 0.4 | - | - | 1.1 | 1.5 |
| Mar 2017 | • | 1 | 0.4 | - | - | 1.2 | 1.5 |
| Apr 2017 | • | 1 | 0.4 | - | - | 1.3 | 1.5 |
| May 2017 | • | 1 | 0.4 | - | - | 1.4 | 1.5 |
| Jun 2017 | • | - | 0.0 | - | - | 1.3 | 1.5 |
| Jul 2017 | • | - | 0.0 | - | - | 1.5 | 1.5 |
| Aug 2017 | • | - | 0.0 | - | - | 1.5 | 1.5 |
| Sep 2017 | • | - | 0.0 | - | - | 1.6 | 1.6 |
| Oct 2017 | • | - | 0.0 | - | - | 1.5 | 1.5 |
| Nov 2017 | • | 1 | 0.4 | - | - | 1.6 | 1.5 |
| Dec 2017 | • | 1 | 0.4 | - | - | 1.5 | 1.5 |
| Jan 2018 | • | 1 | 0.4 | - | - | 1.5 | 1.5 |
| Feb 2018 | • | 1 | 0.4 | - | - | 1.4 | 1.5 |
| Mar 2018 | • | 2 | 0.7 | - | - | 1.4 | 1.5 |
| Apr 2018 | • | 2 | 0.7 | - | - | 1.4 | 1.5 |
| May 2018 | • | 2 | 0.7 | - | - | 1.5 | 1.5 |
| Jun 2018 | • | 2 | 0.7 | - | - | 1.5 | 1.5 |
| Jul 2018 | • | 2 | 0.7 | - | - | 1.5 | 1.5 |
| Aug 2018 | • | 2 | 0.7 | - | - | 1.4 | 1.5 |
| Sep 2018 | • | 2 | 0.7 | - | - | 1.2 | 1.5 |
| Oct 2018 | • | 3 | 1.1 | - | - | 1.1 | 1.5 |
| Nov 2018 | • | 2 | 0.7 | - | - | 1.1 | 1.5 |
| Dec 2018 | • | 2 | 0.7 | - | - | 1.3 | 1.6 |
| Jan 2019 | • | 3 | 1.1 | - | - | 1.4 | 1.5 |
| Feb 2019 | • | 3 | 1.1 | - | - | 1.5 | 1.5 |
| Mar 2019 | • | 2 | 0.7 | - | - | 1.5 | 1.4 |
| Apr 2019 | • | 2 | 0.7 | - | - | 1.4 | 1.4 |
| May 2019 | • | 2 | 0.7 | - | - | 1.4 | 1.4 |
| Jun 2019 | • | 2 | 0.7 | - | - | 1.4 | 1.4 |
| Jul 2019 | • | 2 | 0.7 | - | - | 1.5 | 1.4 |
| Aug 2019 | • | 2 | 0.7 | - | - | 1.5 | 1.4 |
| Sep 2019 | • | 2 | 0.7 | - | - | 1.6 | 1.4 |
| Oct 2019 | • | 1 | 0.4 | - | - | 1.7 | 1.4 |
| Nov 2019 | • | 2 | 0.7 | - | - | 1.7 | 1.4 |
| Dec 2019 | • | 2 | 0.7 | - | - | 1.4 | 1.4 |
| Jan 2020 | • | 1 | 0.4 | - | - | 1.2 | 1.4 |
| Feb 2020 | • | 1 | 0.4 | - | - | 1.0 | 1.4 |
| Mar 2020 | • | 2 | 0.7 | - | - | 1.0 | 1.4 |
| Apr 2020 | • | 2 | 0.7 | - | - | 0.9 | 1.4 |
| May 2020 | • | 2 | 0.7 | - | - | 0.8 | 1.4 |
| Jun 2020 | • | 2 | 0.7 | - | - | 0.8 | 1.4 |
| Jul 2020 | • | 2 | 0.7 | - | - | 0.6 | 1.4 |
| Aug 2020 | • | 2 | 0.7 | - | - | 0.5 | 1.4 |
| Sep 2020 | • | 2 | 0.7 | - | - | 0.4 | 1.3 |
| Oct 2020 | • | 2 | 0.7 | - | - | 0.2 | 1.3 |
| Nov 2020 | • | 1 | 0.4 | - | - | 0.1 | 1.2 |
| Dec 2020 | • | 1 | 0.4 | - | - | 0.2 | 1.2 |
| Jan 2021 | • | 1 | 0.4 | - | - | 0.3 | 1.2 |
| Feb 2021 | • | 1 | 0.4 | - | - | 0.4 | 1.3 |
| Mar 2021 | • | 1 | 0.4 | - | - | 0.4 | 1.2 |
| Apr 2021 | • | 1 | 0.4 | - | - | 0.4 | 1.2 |
| May 2021 | • | 1 | 0.4 | - | - | 0.4 | 1.2 |
| Jun 2021 | • | 1 | 0.4 | - | - | 0.4 | 1.2 |
| Jul 2021 | • | 1 | 0.4 | - | - | 0.4 | 1.2 |
| Aug 2021 | • | 1 | 0.4 | - | - | 0.5 | 1.2 |
| Sep 2021 | • | 1 | 0.4 | - | - | 0.5 | 1.2 |
| Oct 2021 | • | 2 | 0.7 | - | - | 0.6 | 1.2 |
| Nov 2021 | • | 2 | 0.7 | - | - | 0.6 | 1.2 |
| Dec 2021 | • | 3 | 1.1 | - | - | 0.8 | 1.2 |
| Jan 2022 | • | 4 | 1.5 | - | - | 0.8 | 1.2 |
| Feb 2022 | • | 4 | 1.5 | - | - | 0.8 | 1.2 |
| Mar 2022 | • | 4 | 1.5 | - | - | 0.9 | 1.2 |
| Apr 2022 | • | 5 | 1.9 | - | - | 1.1 | 1.2 |
| May 2022 | • | 5 | 1.9 | - | - | 1.2 | 1.3 |
| Jun 2022 | • | 5 | 1.9 | - | - | 1.2 | 1.2 |
| Jul 2022 | • | 5 | 1.9 | - | - | 1.2 | 1.2 |
| Aug 2022 | • | 6 | 2.2 | - | - | 1.2 | 1.3 |
| Sep 2022 | • | 6 | 2.2 | - | - | 1.3 | 1.3 |
| Oct 2022 | • | 5 | 1.9 | - | - | 1.3 | 1.3 |
| Nov 2022 | • | 6 | 2.2 | - | - | 1.3 | 1.3 |
| Dec 2022 | • | 5 | 1.9 | - | - | 1.2 | 1.3 |
| Jan 2023 | • | 5 | 1.9 | - | - | 1.2 | 1.4 |
| Feb 2023 | • | 5 | 1.9 | - | - | 1.1 | 1.4 |
| Mar 2023 | • | 4 | 1.5 | - | - | 1.1 | 1.4 |
| Apr 2023 | • | 3 | 1.1 | - | - | 1.0 | 1.4 |
| May 2023 | • | 5 | 1.9 | - | - | 1.0 | 1.4 |
| Jun 2023 | • | 5 | 1.9 | - | - | 1.0 | 1.4 |
| Jul 2023 | • | 5 | 1.9 | - | - | 1.1 | 1.5 |
| Aug 2023 | • | 4 | 1.5 | - | - | 0.9 | 1.4 |
| Sep 2023 | • | 4 | 1.5 | - | - | 0.8 | 1.4 |
| Oct 2023 | • | 4 | 1.5 | - | - | 0.9 | 1.5 |
| Nov 2023 | • | 3 | 1.1 | - | - | 0.9 | 1.5 |
| Dec 2023 | • | 3 | 1.1 | - | - | 0.8 | 1.5 |
| Jan 2024 | • | 3 | 1.1 | - | - | 0.8 | 1.5 |
| Feb 2024 | • | 3 | 1.1 | - | - | 1.0 | 1.6 |
| Mar 2024 | • | 3 | 1.1 | - | - | 0.9 | 1.6 |
| Apr 2024 | • | 4 | 1.5 | - | - | 0.9 | 1.6 |
| May 2024 | • | 3 | 1.1 | - | - | 0.9 | 1.7 |
| Jun 2024 | • | 3 | 1.1 | - | - | 1.0 | 1.7 |
| Jul 2024 | • | 3 | 1.1 | - | - | 1.1 | 1.7 |
| Aug 2024 | • | 3 | 1.1 | - | - | 1.1 | 1.7 |
| Sep 2024 | • | 3 | 1.1 | - | - | 1.1 | 1.8 |
| Oct 2024 | • | 3 | 1.1 | - | - | 1.2 | 1.8 |
| Nov 2024 | • | 3 | 1.1 | - | - | 1.2 | 1.8 |
| Dec 2024 | • | 4 | 1.5 | - | - | 1.4 | 1.8 |
| Jan 2025 | • | 3 | 1.1 | - | - | 1.6 | 1.9 |
| Feb 2025 | • | 4 | 1.5 | - | - | 1.6 | 1.9 |
| Mar 2025 | • | 4 | 1.5 | - | - | 1.6 | 1.9 |
| Apr 2025 | • | 5 | 1.9 | - | - | 1.8 | 1.9 |
| May 2025 | • | 4 | 1.5 | - | - | 1.6 | 1.9 |
| Jun 2025 | • | 4 | 1.5 | - | - | 1.6 | 1.9 |
Source: UK Health Security Agency
There were only three cases of hospital-onset MRSA cases between May 2016 and March 2022. There were then new cases in April 2022, August 2022, November 2022 and January 2023 with two new cases in May 2023, then one case in January 2024, April 2024, December 2024 and April 2025. So the number of cases are very small in Hull so there is month-on-month variability (see Small Numbers). The latest rate in Hull is the same as England.
Compared with benchmark
MRSA bacteraemia 12-month rolling case counts and rates of hospital-onset, by Sub ICB Location (SICBL) and month (Persons All ages)
|
Period
|
Humber and North Yorkshire ICB - 03F |
NHS Humber and North Yorkshire Integrated Care Board - QOQ
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| Apr 2017 | • | - | 0.0 | - | - | 0.7 | 0.6 |
| May 2017 | • | - | 0.0 | - | - | 0.8 | 0.6 |
| Jun 2017 | • | - | 0.0 | - | - | 0.7 | 0.6 |
| Jul 2017 | • | - | 0.0 | - | - | 0.7 | 0.6 |
| Aug 2017 | • | - | 0.0 | - | - | 0.7 | 0.6 |
| Sep 2017 | • | - | 0.0 | - | - | 0.7 | 0.6 |
| Oct 2017 | • | - | 0.0 | - | - | 0.7 | 0.6 |
| Nov 2017 | • | - | 0.0 | - | - | 0.7 | 0.6 |
| Dec 2017 | • | - | 0.0 | - | - | 0.6 | 0.6 |
| Jan 2018 | • | - | 0.0 | - | - | 0.5 | 0.5 |
| Feb 2018 | • | - | 0.0 | - | - | 0.4 | 0.5 |
| Mar 2018 | • | - | 0.0 | - | - | 0.4 | 0.5 |
| Apr 2018 | • | - | 0.0 | - | - | 0.4 | 0.5 |
| May 2018 | • | - | 0.0 | - | - | 0.4 | 0.5 |
| Jun 2018 | • | - | 0.0 | - | - | 0.4 | 0.5 |
| Jul 2018 | • | - | 0.0 | - | - | 0.4 | 0.5 |
| Aug 2018 | • | - | 0.0 | - | - | 0.4 | 0.5 |
| Sep 2018 | • | - | 0.0 | - | - | 0.4 | 0.5 |
| Oct 2018 | • | 1 | 0.4 | - | - | 0.3 | 0.5 |
| Nov 2018 | • | 1 | 0.4 | - | - | 0.3 | 0.5 |
| Dec 2018 | • | 1 | 0.4 | - | - | 0.4 | 0.5 |
| Jan 2019 | • | 2 | 0.7 | - | - | 0.4 | 0.5 |
| Feb 2019 | • | 2 | 0.7 | - | - | 0.4 | 0.5 |
| Mar 2019 | • | 2 | 0.7 | - | - | 0.4 | 0.5 |
| Apr 2019 | • | 2 | 0.7 | - | - | 0.4 | 0.5 |
| May 2019 | • | 2 | 0.7 | - | - | 0.4 | 0.5 |
| Jun 2019 | • | 2 | 0.7 | - | - | 0.4 | 0.4 |
| Jul 2019 | • | 2 | 0.7 | - | - | 0.5 | 0.4 |
| Aug 2019 | • | 2 | 0.7 | - | - | 0.5 | 0.4 |
| Sep 2019 | • | 2 | 0.7 | - | - | 0.5 | 0.4 |
| Oct 2019 | • | 1 | 0.4 | - | - | 0.5 | 0.4 |
| Nov 2019 | • | 1 | 0.4 | - | - | 0.4 | 0.4 |
| Dec 2019 | • | 1 | 0.4 | - | - | 0.4 | 0.4 |
| Jan 2020 | • | - | 0.0 | - | - | 0.3 | 0.5 |
| Feb 2020 | • | - | 0.0 | - | - | 0.3 | 0.5 |
| Mar 2020 | • | 1 | 0.4 | - | - | 0.4 | 0.5 |
| Apr 2020 | • | 1 | 0.4 | - | - | 0.3 | 0.5 |
| May 2020 | • | 1 | 0.4 | - | - | 0.3 | 0.5 |
| Jun 2020 | • | 1 | 0.4 | - | - | 0.2 | 0.5 |
| Jul 2020 | • | 1 | 0.4 | - | - | 0.1 | 0.5 |
| Aug 2020 | • | 1 | 0.4 | - | - | 0.1 | 0.5 |
| Sep 2020 | • | 1 | 0.4 | - | - | 0.1 | 0.4 |
| Oct 2020 | • | 1 | 0.4 | - | - | 0.1 | 0.4 |
| Nov 2020 | • | 1 | 0.4 | - | - | 0.1 | 0.4 |
| Dec 2020 | • | 1 | 0.4 | - | - | 0.1 | 0.4 |
| Jan 2021 | • | 1 | 0.4 | - | - | 0.1 | 0.5 |
| Feb 2021 | • | 1 | 0.4 | - | - | 0.1 | 0.5 |
| Mar 2021 | • | - | 0.0 | - | - | 0.1 | 0.5 |
| Apr 2021 | • | - | 0.0 | - | - | 0.1 | 0.5 |
| May 2021 | • | - | 0.0 | - | - | 0.1 | 0.5 |
| Jun 2021 | • | - | 0.0 | - | - | 0.1 | 0.5 |
| Jul 2021 | • | - | 0.0 | - | - | 0.1 | 0.5 |
| Aug 2021 | • | - | 0.0 | - | - | 0.2 | 0.5 |
| Sep 2021 | • | - | 0.0 | - | - | 0.2 | 0.5 |
| Oct 2021 | • | - | 0.0 | - | - | 0.2 | 0.5 |
| Nov 2021 | • | - | 0.0 | - | - | 0.2 | 0.5 |
| Dec 2021 | • | - | 0.0 | - | - | 0.2 | 0.5 |
| Jan 2022 | • | - | 0.0 | - | - | 0.2 | 0.5 |
| Feb 2022 | • | - | 0.0 | - | - | 0.2 | 0.4 |
| Mar 2022 | • | - | 0.0 | - | - | 0.2 | 0.4 |
| Apr 2022 | • | 1 | 0.4 | - | - | 0.2 | 0.4 |
| May 2022 | • | 1 | 0.4 | - | - | 0.2 | 0.4 |
| Jun 2022 | • | 1 | 0.4 | - | - | 0.2 | 0.4 |
| Jul 2022 | • | 1 | 0.4 | - | - | 0.2 | 0.4 |
| Aug 2022 | • | 2 | 0.7 | - | - | 0.4 | 0.5 |
| Sep 2022 | • | 2 | 0.7 | - | - | 0.4 | 0.5 |
| Oct 2022 | • | 2 | 0.7 | - | - | 0.4 | 0.5 |
| Nov 2022 | • | 3 | 1.1 | - | - | 0.4 | 0.5 |
| Dec 2022 | • | 3 | 1.1 | - | - | 0.4 | 0.5 |
| Jan 2023 | • | 4 | 1.5 | - | - | 0.5 | 0.5 |
| Feb 2023 | • | 4 | 1.5 | - | - | 0.5 | 0.5 |
| Mar 2023 | • | 4 | 1.5 | - | - | 0.5 | 0.5 |
| Apr 2023 | • | 3 | 1.1 | - | - | 0.5 | 0.5 |
| May 2023 | • | 5 | 1.9 | - | - | 0.5 | 0.5 |
| Jun 2023 | • | 5 | 1.9 | - | - | 0.5 | 0.5 |
| Jul 2023 | • | 5 | 1.9 | - | - | 0.6 | 0.5 |
| Aug 2023 | • | 4 | 1.5 | - | - | 0.5 | 0.5 |
| Sep 2023 | • | 4 | 1.5 | - | - | 0.5 | 0.5 |
| Oct 2023 | • | 4 | 1.5 | - | - | 0.5 | 0.6 |
| Nov 2023 | • | 3 | 1.1 | - | - | 0.5 | 0.6 |
| Dec 2023 | • | 3 | 1.1 | - | - | 0.4 | 0.6 |
| Jan 2024 | • | 3 | 1.1 | - | - | 0.4 | 0.6 |
| Feb 2024 | • | 3 | 1.1 | - | - | 0.5 | 0.6 |
| Mar 2024 | • | 3 | 1.1 | - | - | 0.5 | 0.6 |
| Apr 2024 | • | 4 | 1.5 | - | - | 0.6 | 0.6 |
| May 2024 | • | 2 | 0.7 | - | - | 0.6 | 0.6 |
| Jun 2024 | • | 2 | 0.7 | - | - | 0.7 | 0.6 |
| Jul 2024 | • | 2 | 0.7 | - | - | 0.6 | 0.6 |
| Aug 2024 | • | 2 | 0.7 | - | - | 0.6 | 0.6 |
| Sep 2024 | • | 2 | 0.7 | - | - | 0.6 | 0.7 |
| Oct 2024 | • | 2 | 0.7 | - | - | 0.7 | 0.7 |
| Nov 2024 | • | 2 | 0.7 | - | - | 0.8 | 0.7 |
| Dec 2024 | • | 3 | 1.1 | - | - | 0.9 | 0.7 |
| Jan 2025 | • | 2 | 0.7 | - | - | 1.0 | 0.7 |
| Feb 2025 | • | 2 | 0.7 | - | - | 0.9 | 0.6 |
| Mar 2025 | • | 2 | 0.7 | - | - | 0.9 | 0.6 |
| Apr 2025 | • | 2 | 0.7 | - | - | 1.0 | 0.7 |
| May 2025 | • | 2 | 0.7 | - | - | 0.9 | 0.6 |
| Jun 2025 | • | 2 | 0.7 | - | - | 0.8 | 0.6 |
Source: UK Health Security Agency
The number of community-onset cases of MRSA is also very small. There was one new case in each of months June 2016, November 2017, March 2018, November 2019, March 2021, October 2021, December 2021, January 2022, March 2022, May 2024, February 2025 and April 2025.
Unless there is a new case in May 2025, the 12 month count will decrease back to two for the period June 2024 to May 2025.
Compared with benchmark
MRSA bacteraemia 12-month rolling case counts and rates of community-onset, by Sub ICB Location (SICBL) and month (Persons All ages)
|
Period
|
Humber and North Yorkshire ICB - 03F |
NHS Humber and North Yorkshire Integrated Care Board - QOQ
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| Apr 2017 | • | 1 | 0.4 | - | - | 0.6 | 0.9 |
| May 2017 | • | 1 | 0.4 | - | - | 0.6 | 0.9 |
| Jun 2017 | • | - | 0.0 | - | - | 0.6 | 0.9 |
| Jul 2017 | • | - | 0.0 | - | - | 0.8 | 0.9 |
| Aug 2017 | • | - | 0.0 | - | - | 0.8 | 1.0 |
| Sep 2017 | • | - | 0.0 | - | - | 0.9 | 1.0 |
| Oct 2017 | • | - | 0.0 | - | - | 0.8 | 1.0 |
| Nov 2017 | • | 1 | 0.4 | - | - | 0.9 | 1.0 |
| Dec 2017 | • | 1 | 0.4 | - | - | 0.9 | 1.0 |
| Jan 2018 | • | 1 | 0.4 | - | - | 1.0 | 1.0 |
| Feb 2018 | • | 1 | 0.4 | - | - | 1.0 | 1.0 |
| Mar 2018 | • | 2 | 0.7 | - | - | 1.0 | 1.0 |
| Apr 2018 | • | 2 | 0.7 | - | - | 1.0 | 1.0 |
| May 2018 | • | 2 | 0.7 | - | - | 1.1 | 1.1 |
| Jun 2018 | • | 2 | 0.7 | - | - | 1.1 | 1.0 |
| Jul 2018 | • | 2 | 0.7 | - | - | 1.1 | 1.0 |
| Aug 2018 | • | 2 | 0.7 | - | - | 0.9 | 1.0 |
| Sep 2018 | • | 2 | 0.7 | - | - | 0.9 | 1.0 |
| Oct 2018 | • | 2 | 0.7 | - | - | 0.8 | 1.0 |
| Nov 2018 | • | 1 | 0.4 | - | - | 0.8 | 1.0 |
| Dec 2018 | • | 1 | 0.4 | - | - | 0.9 | 1.1 |
| Jan 2019 | • | 1 | 0.4 | - | - | 1.0 | 1.0 |
| Feb 2019 | • | 1 | 0.4 | - | - | 1.1 | 1.0 |
| Mar 2019 | • | - | 0.0 | - | - | 1.1 | 1.0 |
| Apr 2019 | • | - | 0.0 | - | - | 1.0 | 0.9 |
| May 2019 | • | - | 0.0 | - | - | 1.0 | 0.9 |
| Jun 2019 | • | - | 0.0 | - | - | 1.0 | 1.0 |
| Jul 2019 | • | - | 0.0 | - | - | 0.9 | 1.0 |
| Aug 2019 | • | - | 0.0 | - | - | 0.9 | 1.0 |
| Sep 2019 | • | - | 0.0 | - | - | 1.1 | 0.9 |
| Oct 2019 | • | - | 0.0 | - | - | 1.2 | 1.0 |
| Nov 2019 | • | 1 | 0.4 | - | - | 1.2 | 1.0 |
| Dec 2019 | • | 1 | 0.4 | - | - | 1.1 | 1.0 |
| Jan 2020 | • | 1 | 0.4 | - | - | 0.9 | 1.0 |
| Feb 2020 | • | 1 | 0.4 | - | - | 0.7 | 1.0 |
| Mar 2020 | • | 1 | 0.4 | - | - | 0.6 | 1.0 |
| Apr 2020 | • | 1 | 0.4 | - | - | 0.6 | 1.0 |
| May 2020 | • | 1 | 0.4 | - | - | 0.5 | 1.0 |
| Jun 2020 | • | 1 | 0.4 | - | - | 0.5 | 1.0 |
| Jul 2020 | • | 1 | 0.4 | - | - | 0.5 | 0.9 |
| Aug 2020 | • | 1 | 0.4 | - | - | 0.5 | 0.9 |
| Sep 2020 | • | 1 | 0.4 | - | - | 0.3 | 0.9 |
| Oct 2020 | • | 1 | 0.4 | - | - | 0.2 | 0.8 |
| Nov 2020 | • | - | 0.0 | - | - | 0.1 | 0.8 |
| Dec 2020 | • | - | 0.0 | - | - | 0.1 | 0.8 |
| Jan 2021 | • | - | 0.0 | - | - | 0.2 | 0.8 |
| Feb 2021 | • | - | 0.0 | - | - | 0.2 | 0.8 |
| Mar 2021 | • | 1 | 0.4 | - | - | 0.3 | 0.7 |
| Apr 2021 | • | 1 | 0.4 | - | - | 0.3 | 0.7 |
| May 2021 | • | 1 | 0.4 | - | - | 0.3 | 0.7 |
| Jun 2021 | • | 1 | 0.4 | - | - | 0.2 | 0.7 |
| Jul 2021 | • | 1 | 0.4 | - | - | 0.3 | 0.7 |
| Aug 2021 | • | 1 | 0.4 | - | - | 0.4 | 0.7 |
| Sep 2021 | • | 1 | 0.4 | - | - | 0.4 | 0.7 |
| Oct 2021 | • | 2 | 0.7 | - | - | 0.4 | 0.7 |
| Nov 2021 | • | 2 | 0.7 | - | - | 0.5 | 0.7 |
| Dec 2021 | • | 3 | 1.1 | - | - | 0.6 | 0.7 |
| Jan 2022 | • | 4 | 1.5 | - | - | 0.6 | 0.8 |
| Feb 2022 | • | 4 | 1.5 | - | - | 0.6 | 0.8 |
| Mar 2022 | • | 4 | 1.5 | - | - | 0.7 | 0.8 |
| Apr 2022 | • | 4 | 1.5 | - | - | 0.8 | 0.8 |
| May 2022 | • | 4 | 1.5 | - | - | 0.9 | 0.8 |
| Jun 2022 | • | 4 | 1.5 | - | - | 0.9 | 0.8 |
| Jul 2022 | • | 4 | 1.5 | - | - | 0.9 | 0.8 |
| Aug 2022 | • | 4 | 1.5 | - | - | 0.9 | 0.8 |
| Sep 2022 | • | 4 | 1.5 | - | - | 1.0 | 0.8 |
| Oct 2022 | • | 3 | 1.1 | - | - | 0.9 | 0.9 |
| Nov 2022 | • | 3 | 1.1 | - | - | 0.9 | 0.9 |
| Dec 2022 | • | 2 | 0.7 | - | - | 0.8 | 0.9 |
| Jan 2023 | • | 1 | 0.4 | - | - | 0.7 | 0.9 |
| Feb 2023 | • | 1 | 0.4 | - | - | 0.6 | 0.9 |
| Mar 2023 | • | - | 0.0 | - | - | 0.6 | 0.9 |
| Apr 2023 | • | - | 0.0 | - | - | 0.5 | 0.9 |
| May 2023 | • | - | 0.0 | - | - | 0.5 | 0.9 |
| Jun 2023 | • | - | 0.0 | - | - | 0.5 | 0.9 |
| Jul 2023 | • | - | 0.0 | - | - | 0.5 | 0.9 |
| Aug 2023 | • | - | 0.0 | - | - | 0.5 | 0.9 |
| Sep 2023 | • | - | 0.0 | - | - | 0.4 | 0.9 |
| Oct 2023 | • | - | 0.0 | - | - | 0.4 | 0.9 |
| Nov 2023 | • | - | 0.0 | - | - | 0.4 | 1.0 |
| Dec 2023 | • | - | 0.0 | - | - | 0.4 | 0.9 |
| Jan 2024 | • | - | 0.0 | - | - | 0.4 | 0.9 |
| Feb 2024 | • | - | 0.0 | - | - | 0.5 | 1.0 |
| Mar 2024 | • | - | 0.0 | - | - | 0.3 | 1.0 |
| Apr 2024 | • | - | 0.0 | - | - | 0.3 | 1.0 |
| May 2024 | • | 1 | 0.4 | - | - | 0.3 | 1.0 |
| Jun 2024 | • | 1 | 0.4 | - | - | 0.3 | 1.0 |
| Jul 2024 | • | 1 | 0.4 | - | - | 0.5 | 1.1 |
| Aug 2024 | • | 1 | 0.4 | - | - | 0.5 | 1.1 |
| Sep 2024 | • | 1 | 0.4 | - | - | 0.5 | 1.1 |
| Oct 2024 | • | 1 | 0.4 | - | - | 0.5 | 1.1 |
| Nov 2024 | • | 1 | 0.4 | - | - | 0.5 | 1.1 |
| Dec 2024 | • | 1 | 0.4 | - | - | 0.5 | 1.2 |
| Jan 2025 | • | 1 | 0.4 | - | - | 0.6 | 1.2 |
| Feb 2025 | • | 2 | 0.7 | - | - | 0.7 | 1.2 |
| Mar 2025 | • | 2 | 0.7 | - | - | 0.7 | 1.2 |
| Apr 2025 | • | 3 | 1.1 | - | - | 0.8 | 1.2 |
| May 2025 | • | 2 | 0.7 | - | - | 0.7 | 1.3 |
| Jun 2025 | • | 2 | 0.7 | - | - | 0.8 | 1.3 |
Source: UK Health Security Agency
Clostridium Difficile (C. Difficile) Infection
The number of laboratory confirmed cases of C. difficile that are healthcare associated or community associated that were community-onset are small, and this impacts on trends over time and national comparisons as an increase of only one or two cases within the year can make a relatively large difference to the infection rate per 100,000 population. See Small Numbers within the Glossary for more information.
Cases by Financial Year
The infection rates for C. difficile in Hull (03F) are much lower than England for 2023/24 at 16.0 compared to 29.5 per 100,000 population (46% lower). The rates of community-onset healthcare associated C. difficile cases (48% lower) and rates of community-onset community associated C. difficile cases (68% lower) were also lower in Hull compared to England.
Compared with benchmark
| Indicator | Period | England | NHS Humber and North Yorkshire Integrated Care Board - QOQ | Humber and North Yorkshire ICB - 02Y | Humber and North Yorkshire ICB - 03F | Humber and North Yorkshire ICB - 03H | Humber and North Yorkshire ICB - 03K | Humber and North Yorkshire ICB - 03Q | Humber and North Yorkshire ICB - 42D |
|---|---|---|---|---|---|---|---|---|---|
C. difficile infection case counts and rates by Sub ICB Location (SICBL) and financial year (Persons 2+ yrs) | 2023/24 | 29.5 | 26.2 | 30.4 | 16.0 | 13.3 | 10.0 | 26.0 | 40.8 |
C. difficile infection case counts and rates of community onset-healthcare associated, by Sub ICB Location (SICBL) and financial year (Persons 2+ yrs) | 2023/24 | 5.0 | 4.9 | 6.2 | 2.6 | 3.2 | 1.8 | 5.5 | 6.7 |
C. difficile infection case counts and rates of community onset-community associated, by Sub ICB Location (SICBL) and financial year (Persons 2+ yrs) | 2023/24 | 8.2 | 5.6 | 5.6 | 2.6 | 3.2 | 1.2 | 7.4 | 8.6 |
| Indicator | Period | England | NHS Humber and North Yorkshire Integrated Care Board - QOQ | Humber and North Yorkshire ICB - 02Y | Humber and North Yorkshire ICB - 03F | Humber and North Yorkshire ICB - 03H | Humber and North Yorkshire ICB - 03K | Humber and North Yorkshire ICB - 03Q | Humber and North Yorkshire ICB - 42D |
|---|---|---|---|---|---|---|---|---|---|
C. difficile infection case counts and rates by Sub ICB Location (SICBL) and financial year (Persons 2+ yrs) | 2023/24 | 29.5 | 26.2 | 30.4 | 16.0 | 13.3 | 10.0 | 26.0 | 40.8 |
C. difficile infection case counts and rates of community onset-healthcare associated, by Sub ICB Location (SICBL) and financial year (Persons 2+ yrs) | 2023/24 | 5.0 | 4.9 | 6.2 | 2.6 | 3.2 | 1.8 | 5.5 | 6.7 |
C. difficile infection case counts and rates of community onset-community associated, by Sub ICB Location (SICBL) and financial year (Persons 2+ yrs) | 2023/24 | 8.2 | 5.6 | 5.6 | 2.6 | 3.2 | 1.2 | 7.4 | 8.6 |
In 2009/10, there were 109 cases of C. difficile in Hull, although the infection rate in Hull was lower than England. However, since then there has been a general decreasing trend in Hull albeit with some year-on-year variability. There were 43 cases of C. difficile in Hull for the latest period 2023/24.
There has also been a decrease in England over the period 2009/10 to 2022/23, but the infection rate in Hull has been even lower than England since 2016/17.
Compared with benchmark
C. difficile infection case counts and rates by Sub ICB Location (SICBL) and financial year (Persons 2+ yrs)
|
Period
|
Humber and North Yorkshire ICB - 03F |
NHS Humber and North Yorkshire Integrated Care Board - QOQ
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2007/08 | • | - | 0.0 | - | - | 0.0 | 0.0 |
| 2008/09 | • | - | 0.0 | - | - | 0.0 | 0.0 |
| 2009/10 | • | 109 | 42.6 | - | - | 39.1 | 49.0 |
| 2010/11 | • | 71 | 27.7 | - | - | 37.3 | 41.1 |
| 2011/12 | • | 117 | 45.5 | - | - | 37.1 | 33.8 |
| 2012/13 | • | 73 | 28.5 | - | - | 26.7 | 27.5 |
| 2013/14 | • | 69 | 26.8 | - | - | 27.4 | 24.8 |
| 2014/15 | • | 97 | 37.6 | - | - | 27.2 | 26.1 |
| 2015/16 | • | 72 | 27.7 | - | - | 26.4 | 25.7 |
| 2016/17 | • | 50 | 19.3 | - | - | 22.1 | 23.3 |
| 2017/18 | • | 50 | 19.2 | - | - | 21.9 | 23.9 |
| 2018/19 | • | 51 | 19.6 | - | - | 21.0 | 21.9 |
| 2019/20 | • | 50 | 19.2 | - | - | 24.5 | 23.4 |
| 2020/21 | • | 45 | 17.3 | - | - | 22.5 | 22.2 |
| 2021/22 | • | 39 | 14.6 | - | - | 26.9 | 25.2 |
| 2022/23 | • | 42 | 15.6 | - | - | 27.4 | 27.3 |
| 2023/24 | • | 43 | 16.0 | - | - | 26.2 | 29.5 |
Source: UK Health Security Agency
The number of cases of C. difficile that were healthcare associated with community-onset were small in Hull with seven cases in 2023/24.
Compared with benchmark
C. difficile infection case counts and rates of community onset-healthcare associated, by Sub ICB Location (SICBL) and financial year (Persons 2+ yrs)
|
Period
|
Humber and North Yorkshire ICB - 03F |
NHS Humber and North Yorkshire Integrated Care Board - QOQ
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2017/18 | • | 5 | 1.9 | - | - | 3.0 | 3.4 |
| 2018/19 | • | 18 | 6.9 | - | - | 4.9 | 4.1 |
| 2019/20 | • | 10 | 3.8 | - | - | 5.1 | 4.4 |
| 2020/21 | • | 11 | 4.2 | - | - | 4.2 | 3.9 |
| 2021/22 | • | 7 | 2.6 | - | - | 5.9 | 4.3 |
| 2022/23 | • | 9 | 3.3 | - | - | 6.0 | 4.4 |
| 2023/24 | • | 7 | 2.6 | - | - | 4.9 | 5.0 |
Source: UK Health Security Agency
The number of cases of C. difficile that were community associated with community-onset were small in Hull with seven cases in 2023/24. The infection rate of community-onset community associated cases has been consistently lower in Hull than England for the period 2017/18 to 2023/24.
Compared with benchmark
C. difficile infection case counts and rates of community onset-community associated, by Sub ICB Location (SICBL) and financial year (Persons 2+ yrs)
|
Period
|
Humber and North Yorkshire ICB - 03F |
NHS Humber and North Yorkshire Integrated Care Board - QOQ
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2017/18 | • | 1 | 0.4 | - | - | 3.8 | 5.1 |
| 2018/19 | • | 10 | 3.8 | - | - | 5.5 | 6.1 |
| 2019/20 | • | 12 | 4.6 | - | - | 5.2 | 6.7 |
| 2020/21 | • | 6 | 2.3 | - | - | 6.0 | 7.0 |
| 2021/22 | • | 8 | 3.0 | - | - | 6.3 | 7.4 |
| 2022/23 | • | 10 | 3.7 | - | - | 6.4 | 7.5 |
| 2023/24 | • | 7 | 2.6 | - | - | 5.6 | 8.2 |
Source: UK Health Security Agency
Cases by Month (12-Month Rolling Total)
The number of laboratory confirmed cases of C. difficile is given below for Hull (03F) compared to the other sub-ICBs within the Humber and North Yorkshire ICB.
The rates are also given separately for community-onset associated with healthcare and community-onset associated with community, so are slightly different to the infections given above which have rates separately for hospital-onset or community-onset infections.
For the year May 2024 to April 2025, the rates in Hull for community onset-healthcare associated were similar to England, but the community onset-community associated in Hull were half that of England. For all cases, the rates were also considerably lower for Hull compared to England (21.2 versus 33.0 cases per 100,000 population).
Compared with benchmark
| Indicator | Period | England | NHS Humber and North Yorkshire Integrated Care Board - QOQ | Humber and North Yorkshire ICB - 02Y | Humber and North Yorkshire ICB - 03F | Humber and North Yorkshire ICB - 03H | Humber and North Yorkshire ICB - 03K | Humber and North Yorkshire ICB - 03Q | Humber and North Yorkshire ICB - 42D |
|---|---|---|---|---|---|---|---|---|---|
C. difficile infection 12-month rolling counts and rates, by Sub ICB Location (SICBL)
and month (Persons 2+ yrs) | Jun 2025 | 32.5 | 28.4 | 28.3 | 20.1 | 14.6 | 15.9 | 36.3 | 37.0 |
C. difficile infection 12-month rolling counts and rates of community onset-healthcare associated, by Sub ICB Location (SICBL) and month (Persons 2+ yrs) | Jun 2025 | 5.7 | 5.9 | 4.4 | 4.8 | 3.2 | 2.4 | 8.3 | 8.1 |
C. difficile infection 12-month rolling counts and rates of community onset-community associated, by Sub ICB Location (SICBL) and month (Persons 2+ yrs) | Jun 2025 | 8.9 | 6.7 | 5.6 | 4.1 | 1.3 | 4.1 | 8.8 | 10.5 |
| Indicator | Period | England | NHS Humber and North Yorkshire Integrated Care Board - QOQ | Humber and North Yorkshire ICB - 02Y | Humber and North Yorkshire ICB - 03F | Humber and North Yorkshire ICB - 03H | Humber and North Yorkshire ICB - 03K | Humber and North Yorkshire ICB - 03Q | Humber and North Yorkshire ICB - 42D |
|---|---|---|---|---|---|---|---|---|---|
C. difficile infection 12-month rolling counts and rates, by Sub ICB Location (SICBL)
and month (Persons 2+ yrs) | Jun 2025 | 32.5 | 28.4 | 28.3 | 20.1 | 14.6 | 15.9 | 36.3 | 37.0 |
C. difficile infection 12-month rolling counts and rates of community onset-healthcare associated, by Sub ICB Location (SICBL) and month (Persons 2+ yrs) | Jun 2025 | 5.7 | 5.9 | 4.4 | 4.8 | 3.2 | 2.4 | 8.3 | 8.1 |
C. difficile infection 12-month rolling counts and rates of community onset-community associated, by Sub ICB Location (SICBL) and month (Persons 2+ yrs) | Jun 2025 | 8.9 | 6.7 | 5.6 | 4.1 | 1.3 | 4.1 | 8.8 | 10.5 |
Between 2015 and mid-2016, the rates of C. difficile infections was higher in Hull compared to England, but since then the rates have been consistently lower than England except for Spring and Summer of 2019 when rates were similar in Hull as England.
Over the three year period from the year May 2020 to April 2021 to the year May 2023 to April 2024, the rates in Hull have been around 14-16 cases per year per 100,000 population. In contrast, over the same period the rate in England has increased gradually from 22 to 30 cases per 100,000 population.
After April 2024, the rate in Hull started to increase from 16 to 23 cases per 100,000 population for the period November 2023 to October 2024. However, in the last seven months the rate has decreased slightly in Hull to 21 cases per 100,000 population for the latest period May 2024 to April 2025. In contrast, the rate for England increased to 33 cases per 100,000 population and has remained around 33 cases per 100,000 population for the last seven months.
In the latest period, May 2024 to April 2025, there has been 57 cases of C. difficile in Hull.
Compared with benchmark
The number of community-onset healthcare associated cases of C. difficile is relatively low in Hull (see Small Numbers within the Glossary for more information).
Except for the period September 2018 to December 2019 when rates in Hull were considerably higher and March to August 2021 where rates in Hull were marginally higher, the rates of community-onset healthcare associated cases of C. difficile has been lower in Hull compared to England, although there is some month-to-month variability in Hull.
The number of cases is very small in Hull, but has increased in the last year or so. Toward the end of 2023, in the previous 12 month period, there has been around 2.2 cases per 100,000 population (or six cases in total) over the year, but this has gradually increased in Hull with 5.6 cases per 100,000 population for the latest period May 2024 to April 2025. Despite the rate increasing in Hull in the last 18 months or so, the latest rate is marginally lower than the rate in England.
In the latest period May 2024 to April 2025, there had been 15 cases of C. difficile that were community-onset in Hull that were associated with healthcare.
Compared with benchmark
C. difficile infection 12-month rolling counts and rates of community onset-healthcare associated, by Sub ICB Location (SICBL) and month (Persons 2+ yrs)
|
Period
|
Humber and North Yorkshire ICB - 03F |
NHS Humber and North Yorkshire Integrated Care Board - QOQ
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| Apr 2017 | • | - | 0.0 | - | - | 0.4 | 0.2 |
| May 2017 | • | - | 0.0 | - | - | 0.6 | 0.4 |
| Jun 2017 | • | - | 0.0 | - | - | 0.7 | 0.6 |
| Jul 2017 | • | - | 0.0 | - | - | 0.8 | 0.8 |
| Aug 2017 | • | - | 0.0 | - | - | 0.9 | 1.2 |
| Sep 2017 | • | - | 0.0 | - | - | 1.2 | 1.5 |
| Oct 2017 | • | - | 0.0 | - | - | 1.4 | 1.8 |
| Nov 2017 | • | 1 | 0.4 | - | - | 1.8 | 2.1 |
| Dec 2017 | • | 2 | 0.7 | - | - | 2.1 | 2.4 |
| Jan 2018 | • | 4 | 1.5 | - | - | 2.4 | 2.8 |
| Feb 2018 | • | 5 | 1.9 | - | - | 2.7 | 3.1 |
| Mar 2018 | • | 5 | 1.9 | - | - | 3.0 | 3.4 |
| Apr 2018 | • | 6 | 2.2 | - | - | 3.1 | 3.6 |
| May 2018 | • | 8 | 3.0 | - | - | 3.3 | 3.8 |
| Jun 2018 | • | 9 | 3.4 | - | - | 3.5 | 3.9 |
| Jul 2018 | • | 10 | 3.7 | - | - | 3.7 | 4.1 |
| Aug 2018 | • | 11 | 4.1 | - | - | 4.0 | 4.2 |
| Sep 2018 | • | 13 | 4.9 | - | - | 4.1 | 4.3 |
| Oct 2018 | • | 16 | 6.0 | - | - | 4.5 | 4.3 |
| Nov 2018 | • | 18 | 6.7 | - | - | 4.7 | 4.3 |
| Dec 2018 | • | 18 | 6.7 | - | - | 4.8 | 4.3 |
| Jan 2019 | • | 18 | 6.7 | - | - | 4.9 | 4.2 |
| Feb 2019 | • | 17 | 6.3 | - | - | 4.8 | 4.2 |
| Mar 2019 | • | 18 | 6.7 | - | - | 4.9 | 4.1 |
| Apr 2019 | • | 19 | 7.1 | - | - | 5.2 | 4.1 |
| May 2019 | • | 19 | 7.1 | - | - | 5.6 | 4.1 |
| Jun 2019 | • | 18 | 6.7 | - | - | 5.5 | 4.1 |
| Jul 2019 | • | 19 | 7.1 | - | - | 5.8 | 4.1 |
| Aug 2019 | • | 18 | 6.7 | - | - | 5.9 | 4.2 |
| Sep 2019 | • | 17 | 6.3 | - | - | 6.0 | 4.2 |
| Oct 2019 | • | 14 | 5.2 | - | - | 5.8 | 4.3 |
| Nov 2019 | • | 13 | 4.8 | - | - | 5.6 | 4.3 |
| Dec 2019 | • | 12 | 4.5 | - | - | 5.4 | 4.3 |
| Jan 2020 | • | 10 | 3.7 | - | - | 5.4 | 4.3 |
| Feb 2020 | • | 11 | 4.1 | - | - | 5.3 | 4.4 |
| Mar 2020 | • | 10 | 3.7 | - | - | 5.1 | 4.4 |
| Apr 2020 | • | 8 | 3.0 | - | - | 4.7 | 4.3 |
| May 2020 | • | 7 | 2.6 | - | - | 4.2 | 4.2 |
| Jun 2020 | • | 7 | 2.6 | - | - | 4.1 | 4.2 |
| Jul 2020 | • | 7 | 2.6 | - | - | 4.2 | 4.2 |
| Aug 2020 | • | 7 | 2.6 | - | - | 4.1 | 4.2 |
| Sep 2020 | • | 8 | 3.0 | - | - | 4.1 | 4.1 |
| Oct 2020 | • | 9 | 3.4 | - | - | 3.9 | 4.0 |
| Nov 2020 | • | 9 | 3.4 | - | - | 4.0 | 4.0 |
| Dec 2020 | • | 10 | 3.7 | - | - | 4.2 | 4.1 |
| Jan 2021 | • | 10 | 3.7 | - | - | 4.1 | 4.0 |
| Feb 2021 | • | 10 | 3.7 | - | - | 4.0 | 3.9 |
| Mar 2021 | • | 11 | 4.1 | - | - | 4.2 | 3.9 |
| Apr 2021 | • | 11 | 4.1 | - | - | 4.1 | 4.0 |
| May 2021 | • | 11 | 4.1 | - | - | 4.5 | 4.1 |
| Jun 2021 | • | 12 | 4.5 | - | - | 4.9 | 4.2 |
| Jul 2021 | • | 11 | 4.1 | - | - | 4.9 | 4.2 |
| Aug 2021 | • | 12 | 4.5 | - | - | 5.2 | 4.2 |
| Sep 2021 | • | 11 | 4.1 | - | - | 5.2 | 4.2 |
| Oct 2021 | • | 11 | 4.1 | - | - | 5.5 | 4.3 |
| Nov 2021 | • | 9 | 3.4 | - | - | 5.3 | 4.3 |
| Dec 2021 | • | 8 | 3.0 | - | - | 5.5 | 4.3 |
| Jan 2022 | • | 8 | 3.0 | - | - | 5.7 | 4.4 |
| Feb 2022 | • | 7 | 2.6 | - | - | 5.9 | 4.4 |
| Mar 2022 | • | 7 | 2.6 | - | - | 5.9 | 4.3 |
| Apr 2022 | • | 7 | 2.6 | - | - | 6.0 | 4.3 |
| May 2022 | • | 6 | 2.2 | - | - | 5.7 | 4.3 |
| Jun 2022 | • | 5 | 1.9 | - | - | 5.7 | 4.3 |
| Jul 2022 | • | 6 | 2.2 | - | - | 5.7 | 4.3 |
| Aug 2022 | • | 5 | 1.9 | - | - | 5.6 | 4.3 |
| Sep 2022 | • | 6 | 2.2 | - | - | 5.3 | 4.3 |
| Oct 2022 | • | 6 | 2.2 | - | - | 5.4 | 4.3 |
| Nov 2022 | • | 7 | 2.6 | - | - | 5.9 | 4.3 |
| Dec 2022 | • | 8 | 3.0 | - | - | 5.9 | 4.3 |
| Jan 2023 | • | 8 | 3.0 | - | - | 5.8 | 4.3 |
| Feb 2023 | • | 10 | 3.7 | - | - | 5.6 | 4.3 |
| Mar 2023 | • | 9 | 3.3 | - | - | 6.0 | 4.4 |
| Apr 2023 | • | 9 | 3.3 | - | - | 5.9 | 4.5 |
| May 2023 | • | 9 | 3.4 | - | - | 5.7 | 4.6 |
| Jun 2023 | • | 9 | 3.4 | - | - | 5.6 | 4.6 |
| Jul 2023 | • | 9 | 3.4 | - | - | 5.5 | 4.6 |
| Aug 2023 | • | 9 | 3.4 | - | - | 5.1 | 4.5 |
| Sep 2023 | • | 7 | 2.6 | - | - | 5.3 | 4.6 |
| Oct 2023 | • | 6 | 2.2 | - | - | 5.0 | 4.6 |
| Nov 2023 | • | 6 | 2.2 | - | - | 4.7 | 4.6 |
| Dec 2023 | • | 6 | 2.2 | - | - | 4.4 | 4.7 |
| Jan 2024 | • | 8 | 3.0 | - | - | 4.8 | 4.8 |
| Feb 2024 | • | 6 | 2.2 | - | - | 5.1 | 4.9 |
| Mar 2024 | • | 7 | 2.6 | - | - | 4.9 | 4.9 |
| Apr 2024 | • | 8 | 3.0 | - | - | 5.4 | 5.1 |
| May 2024 | • | 10 | 3.7 | - | - | 5.5 | 5.1 |
| Jun 2024 | • | 11 | 4.1 | - | - | 5.9 | 5.1 |
| Jul 2024 | • | 10 | 3.7 | - | - | 6.0 | 5.3 |
| Aug 2024 | • | 11 | 4.1 | - | - | 6.2 | 5.4 |
| Sep 2024 | • | 12 | 4.5 | - | - | 6.1 | 5.6 |
| Oct 2024 | • | 13 | 4.8 | - | - | 6.6 | 5.7 |
| Nov 2024 | • | 13 | 4.8 | - | - | 6.7 | 5.8 |
| Dec 2024 | • | 12 | 4.5 | - | - | 6.8 | 5.8 |
| Jan 2025 | • | 11 | 4.1 | - | - | 6.4 | 5.9 |
| Feb 2025 | • | 15 | 5.6 | - | - | 6.6 | 5.8 |
| Mar 2025 | • | 15 | 5.6 | - | - | 6.6 | 5.8 |
| Apr 2025 | • | 15 | 5.6 | - | - | 6.0 | 5.7 |
| May 2025 | • | 13 | 4.8 | - | - | 6.1 | 5.7 |
| Jun 2025 | • | 13 | 4.8 | - | - | 5.9 | 5.7 |
Source: UK Health Security Agency
The rate of community onset-community associated infections of C. difficile has increased over time in Hull between the beginning of 2017 and the beginning of 2019, but then remained relatively consistent with 3-4 cases over the year per 100,000 population. The numbers dropped at the start of the COVID-19 pandemic from a high of 4.6 cases per year per 100,000 population in March 2020 to a low of 1.5 cases per year per 100,000 population for the year to July 2021. The numbers increased since then back to around 3-4 cases per year per 100,000 population in 2022, falling to just over two cases per year per 100,000 population towards the end of 2023. Since then though, the rate has increased to almost six cases per 100,000 population for the period January 2024 to December 2024, although has fallen to 4.1 cases per 100,000 population for the latest period May 2024 to April 2025.
The absolute number of cases in the year are still relatively low at 11 infections of C. difficile in the community that were community-onset for the latest period May 2024 to April 2025.
Despite the recent in increase in Hull over the last year or so, the infection rate in Hull has been consistently lower than England.
Compared with benchmark
C. difficile infection 12-month rolling counts and rates of community onset-community associated, by Sub ICB Location (SICBL) and month (Persons 2+ yrs)
|
Period
|
Humber and North Yorkshire ICB - 03F |
NHS Humber and North Yorkshire Integrated Care Board - QOQ
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| Apr 2017 | • | - | 0.0 | - | - | 0.2 | 0.3 |
| May 2017 | • | - | 0.0 | - | - | 0.6 | 0.6 |
| Jun 2017 | • | - | 0.0 | - | - | 0.8 | 0.9 |
| Jul 2017 | • | - | 0.0 | - | - | 1.1 | 1.3 |
| Aug 2017 | • | - | 0.0 | - | - | 1.4 | 1.8 |
| Sep 2017 | • | - | 0.0 | - | - | 1.8 | 2.2 |
| Oct 2017 | • | - | 0.0 | - | - | 2.3 | 2.8 |
| Nov 2017 | • | 1 | 0.4 | - | - | 2.4 | 3.3 |
| Dec 2017 | • | 1 | 0.4 | - | - | 2.8 | 3.7 |
| Jan 2018 | • | 1 | 0.4 | - | - | 3.4 | 4.2 |
| Feb 2018 | • | 1 | 0.4 | - | - | 3.9 | 4.7 |
| Mar 2018 | • | 1 | 0.4 | - | - | 3.8 | 5.1 |
| Apr 2018 | • | 3 | 1.1 | - | - | 4.3 | 5.4 |
| May 2018 | • | 5 | 1.9 | - | - | 4.5 | 5.7 |
| Jun 2018 | • | 6 | 2.2 | - | - | 4.9 | 6.0 |
| Jul 2018 | • | 7 | 2.6 | - | - | 5.0 | 6.2 |
| Aug 2018 | • | 7 | 2.6 | - | - | 5.1 | 6.4 |
| Sep 2018 | • | 9 | 3.4 | - | - | 5.0 | 6.5 |
| Oct 2018 | • | 9 | 3.4 | - | - | 5.1 | 6.5 |
| Nov 2018 | • | 9 | 3.4 | - | - | 5.4 | 6.4 |
| Dec 2018 | • | 9 | 3.4 | - | - | 5.4 | 6.4 |
| Jan 2019 | • | 10 | 3.7 | - | - | 5.1 | 6.3 |
| Feb 2019 | • | 10 | 3.7 | - | - | 5.0 | 6.2 |
| Mar 2019 | • | 10 | 3.7 | - | - | 5.5 | 6.1 |
| Apr 2019 | • | 11 | 4.1 | - | - | 5.6 | 6.2 |
| May 2019 | • | 10 | 3.7 | - | - | 5.3 | 6.1 |
| Jun 2019 | • | 11 | 4.1 | - | - | 5.1 | 6.1 |
| Jul 2019 | • | 11 | 4.1 | - | - | 5.1 | 6.1 |
| Aug 2019 | • | 11 | 4.1 | - | - | 5.3 | 6.1 |
| Sep 2019 | • | 10 | 3.7 | - | - | 5.4 | 6.2 |
| Oct 2019 | • | 10 | 3.7 | - | - | 5.2 | 6.3 |
| Nov 2019 | • | 9 | 3.4 | - | - | 5.1 | 6.4 |
| Dec 2019 | • | 9 | 3.4 | - | - | 5.1 | 6.5 |
| Jan 2020 | • | 10 | 3.7 | - | - | 5.3 | 6.6 |
| Feb 2020 | • | 11 | 4.1 | - | - | 5.4 | 6.7 |
| Mar 2020 | • | 12 | 4.5 | - | - | 5.2 | 6.7 |
| Apr 2020 | • | 9 | 3.3 | - | - | 4.8 | 6.6 |
| May 2020 | • | 9 | 3.3 | - | - | 5.0 | 6.7 |
| Jun 2020 | • | 8 | 3.0 | - | - | 5.1 | 6.8 |
| Jul 2020 | • | 8 | 3.0 | - | - | 5.3 | 6.8 |
| Aug 2020 | • | 8 | 3.0 | - | - | 5.3 | 6.9 |
| Sep 2020 | • | 8 | 3.0 | - | - | 5.2 | 6.8 |
| Oct 2020 | • | 9 | 3.4 | - | - | 5.4 | 6.8 |
| Nov 2020 | • | 10 | 3.7 | - | - | 5.5 | 6.8 |
| Dec 2020 | • | 10 | 3.7 | - | - | 5.5 | 6.9 |
| Jan 2021 | • | 8 | 3.0 | - | - | 5.7 | 6.8 |
| Feb 2021 | • | 7 | 2.6 | - | - | 5.7 | 6.9 |
| Mar 2021 | • | 6 | 2.2 | - | - | 6.1 | 7.0 |
| Apr 2021 | • | 6 | 2.2 | - | - | 6.1 | 7.1 |
| May 2021 | • | 5 | 1.9 | - | - | 6.0 | 7.1 |
| Jun 2021 | • | 5 | 1.9 | - | - | 5.8 | 7.2 |
| Jul 2021 | • | 4 | 1.5 | - | - | 5.7 | 7.2 |
| Aug 2021 | • | 7 | 2.6 | - | - | 5.8 | 7.2 |
| Sep 2021 | • | 6 | 2.2 | - | - | 6.1 | 7.3 |
| Oct 2021 | • | 5 | 1.9 | - | - | 6.1 | 7.3 |
| Nov 2021 | • | 5 | 1.9 | - | - | 6.4 | 7.4 |
| Dec 2021 | • | 5 | 1.9 | - | - | 6.5 | 7.4 |
| Jan 2022 | • | 7 | 2.6 | - | - | 6.6 | 7.4 |
| Feb 2022 | • | 8 | 3.0 | - | - | 6.5 | 7.3 |
| Mar 2022 | • | 8 | 3.0 | - | - | 6.3 | 7.4 |
| Apr 2022 | • | 8 | 3.0 | - | - | 6.4 | 7.4 |
| May 2022 | • | 9 | 3.4 | - | - | 6.7 | 7.4 |
| Jun 2022 | • | 9 | 3.4 | - | - | 6.9 | 7.4 |
| Jul 2022 | • | 10 | 3.7 | - | - | 6.9 | 7.3 |
| Aug 2022 | • | 7 | 2.6 | - | - | 6.8 | 7.5 |
| Sep 2022 | • | 8 | 3.0 | - | - | 6.5 | 7.5 |
| Oct 2022 | • | 9 | 3.4 | - | - | 6.6 | 7.5 |
| Nov 2022 | • | 9 | 3.4 | - | - | 6.3 | 7.5 |
| Dec 2022 | • | 9 | 3.4 | - | - | 6.2 | 7.5 |
| Jan 2023 | • | 9 | 3.4 | - | - | 6.1 | 7.5 |
| Feb 2023 | • | 8 | 3.0 | - | - | 6.2 | 7.5 |
| Mar 2023 | • | 10 | 3.7 | - | - | 6.4 | 7.5 |
| Apr 2023 | • | 10 | 3.7 | - | - | 6.1 | 7.5 |
| May 2023 | • | 9 | 3.4 | - | - | 5.9 | 7.5 |
| Jun 2023 | • | 8 | 3.0 | - | - | 5.9 | 7.6 |
| Jul 2023 | • | 7 | 2.6 | - | - | 5.8 | 7.6 |
| Aug 2023 | • | 7 | 2.6 | - | - | 5.8 | 7.5 |
| Sep 2023 | • | 6 | 2.2 | - | - | 5.5 | 7.5 |
| Oct 2023 | • | 7 | 2.6 | - | - | 5.7 | 7.6 |
| Nov 2023 | • | 6 | 2.2 | - | - | 5.8 | 7.7 |
| Dec 2023 | • | 6 | 2.2 | - | - | 5.7 | 7.8 |
| Jan 2024 | • | 6 | 2.2 | - | - | 6.0 | 7.9 |
| Feb 2024 | • | 7 | 2.6 | - | - | 5.9 | 8.1 |
| Mar 2024 | • | 7 | 2.6 | - | - | 5.6 | 8.2 |
| Apr 2024 | • | 7 | 2.6 | - | - | 5.9 | 8.4 |
| May 2024 | • | 9 | 3.3 | - | - | 6.4 | 8.7 |
| Jun 2024 | • | 11 | 4.1 | - | - | 6.2 | 8.7 |
| Jul 2024 | • | 11 | 4.1 | - | - | 6.6 | 9.0 |
| Aug 2024 | • | 12 | 4.5 | - | - | 6.5 | 9.2 |
| Sep 2024 | • | 14 | 5.2 | - | - | 7.0 | 9.3 |
| Oct 2024 | • | 12 | 4.5 | - | - | 6.8 | 9.4 |
| Nov 2024 | • | 13 | 4.8 | - | - | 6.8 | 9.4 |
| Dec 2024 | • | 15 | 5.6 | - | - | 6.9 | 9.4 |
| Jan 2025 | • | 13 | 4.8 | - | - | 6.5 | 9.4 |
| Feb 2025 | • | 12 | 4.5 | - | - | 6.6 | 9.4 |
| Mar 2025 | • | 10 | 3.7 | - | - | 6.6 | 9.3 |
| Apr 2025 | • | 11 | 4.1 | - | - | 6.8 | 9.3 |
| May 2025 | • | 12 | 4.5 | - | - | 6.7 | 9.1 |
| Jun 2025 | • | 11 | 4.1 | - | - | 6.7 | 8.9 |
Source: UK Health Security Agency
Klebsiella Spp. Bacteraemia
Cases by Financial Year
For 2023/24, the rate of cases of klebsiella spp. bacteraemia infection cases per 100,000 population was higher in Hull (03F) compared to England both overall and for community-onset cases.
Compared with benchmark
| Indicator | Period | England | NHS Humber and North Yorkshire Integrated Care Board - QOQ | Humber and North Yorkshire ICB - 02Y | Humber and North Yorkshire ICB - 03F | Humber and North Yorkshire ICB - 03H | Humber and North Yorkshire ICB - 03K | Humber and North Yorkshire ICB - 03Q | Humber and North Yorkshire ICB - 42D |
|---|---|---|---|---|---|---|---|---|---|
Klebsiella spp. bacteraemia case counts and rates, by sub ICB location (SICBL) and financial year (Persons All ages) | 2023/24 | 22.9 | 26.9 | 30.1 | 29.3 | 25.3 | 22.3 | 20.0 | 31.1 |
Klebsiella spp. bacteraemia case counts and rates of community-onset, by sub ICB location (SICBL) and financial year (Persons All ages) | 2023/24 | 15.9 | 18.8 | 20.8 | 19.3 | 21.5 | 12.3 | 12.6 | 23.9 |
| Indicator | Period | England | NHS Humber and North Yorkshire Integrated Care Board - QOQ | Humber and North Yorkshire ICB - 02Y | Humber and North Yorkshire ICB - 03F | Humber and North Yorkshire ICB - 03H | Humber and North Yorkshire ICB - 03K | Humber and North Yorkshire ICB - 03Q | Humber and North Yorkshire ICB - 42D |
|---|---|---|---|---|---|---|---|---|---|
Klebsiella spp. bacteraemia case counts and rates, by sub ICB location (SICBL) and financial year (Persons All ages) | 2023/24 | 22.9 | 26.9 | 30.1 | 29.3 | 25.3 | 22.3 | 20.0 | 31.1 |
Klebsiella spp. bacteraemia case counts and rates of community-onset, by sub ICB location (SICBL) and financial year (Persons All ages) | 2023/24 | 15.9 | 18.8 | 20.8 | 19.3 | 21.5 | 12.3 | 12.6 | 23.9 |
There is year-on-year variability in the number of cases of klebsiella spp. infections in Hull, but the pattern of change between 2017/18 and 2022/23 in Hull is similar to that of England. However, in the last year there has been a much larger increase in the number of infections in Hull.
During the year 2023/24, there were 79 cases of klebsiella spp. infections in Hull.
Compared with benchmark
Klebsiella spp. bacteraemia case counts and rates, by sub ICB location (SICBL) and financial year (Persons All ages)
|
Period
|
Humber and North Yorkshire ICB - 03F |
NHS Humber and North Yorkshire Integrated Care Board - QOQ
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2017/18 | • | 42 | 16.1 | - | - | 20.6 | 17.6 |
| 2018/19 | • | 54 | 20.7 | - | - | 20.8 | 19.1 |
| 2019/20 | • | 52 | 20.0 | - | - | 22.1 | 19.6 |
| 2020/21 | • | 45 | 17.3 | - | - | 20.3 | 19.8 |
| 2021/22 | • | 63 | 23.6 | - | - | 22.4 | 20.2 |
| 2022/23 | • | 48 | 17.9 | - | - | 22.4 | 20.7 |
| 2023/24 | • | 79 | 29.3 | - | - | 26.9 | 22.9 |
Source: UK Health Security Agency
There is year-on-year variability in the number of cases of klebsiella spp. infections taht are community-onset in Hull, but the pattern of change between 2017/18 and 2022/23 in Hull is similar to that of England with a very marginal increase over the period of time. However, again over the last year, the increase in Hull is greater.
The rate in Hull has generally been lower than England with the exception of 2021/22 and the latest year 2023/24.
During the year 2023/24, there were 52 cases of klebsiella spp. infections that were community-onset in Hull so almost two-thirds of cases of klebiella spp. infections in Hull are community-onset.
Compared with benchmark
Klebsiella spp. bacteraemia case counts and rates of community-onset, by sub ICB location (SICBL) and financial year (Persons All ages)
|
Period
|
Humber and North Yorkshire ICB - 03F |
NHS Humber and North Yorkshire Integrated Care Board - QOQ
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2017/18 | • | 26 | 10.0 | - | - | 15.1 | 12.3 |
| 2018/19 | • | 34 | 13.1 | - | - | 15.1 | 13.4 |
| 2019/20 | • | 30 | 11.5 | - | - | 16.3 | 13.9 |
| 2020/21 | • | 29 | 11.1 | - | - | 15.1 | 13.1 |
| 2021/22 | • | 43 | 16.1 | - | - | 16.0 | 13.6 |
| 2022/23 | • | 31 | 11.5 | - | - | 15.1 | 13.8 |
| 2023/24 | • | 52 | 19.3 | - | - | 18.8 | 15.9 |
Source: UK Health Security Agency
Cases by Month (12-Month Rolling Total)
For the year to April 2025, the rate of klebsiella spp. infections is the same in Hull (03F) as England being slightly lower for hospital-onset cases and slightly higher for community-onset cases.
Compared with benchmark
| Indicator | Period | England | NHS Humber and North Yorkshire Integrated Care Board - QOQ | Humber and North Yorkshire ICB - 02Y | Humber and North Yorkshire ICB - 03F | Humber and North Yorkshire ICB - 03H | Humber and North Yorkshire ICB - 03K | Humber and North Yorkshire ICB - 03Q | Humber and North Yorkshire ICB - 42D |
|---|---|---|---|---|---|---|---|---|---|
Klebsiella spp. bacteraemia 12-month rolling case counts and rates, by Sub ICB Location (SICBL) and month (Persons All ages) | Jun 2025 | 23.7 | 25.7 | 25.5 | 23.1 | 29.2 | 27.7 | 23.7 | 27.0 |
Klebsiella spp. bacteraemia 12-month rolling case counts and rates of hospital-onset, by Sub ICB Location (SICBL) and month (Persons All ages) | Jun 2025 | 7.3 | 6.7 | 7.8 | 6.3 | 9.5 | 6.5 | 6.1 | 5.6 |
Klebsiella spp. bacteraemia 12-month rolling case counts and rates of community-onset, by Sub ICB Location (SICBL) and month (Persons All ages) | Jun 2025 | 16.4 | 19.0 | 17.8 | 16.8 | 19.7 | 21.2 | 17.6 | 21.4 |
| Indicator | Period | England | NHS Humber and North Yorkshire Integrated Care Board - QOQ | Humber and North Yorkshire ICB - 02Y | Humber and North Yorkshire ICB - 03F | Humber and North Yorkshire ICB - 03H | Humber and North Yorkshire ICB - 03K | Humber and North Yorkshire ICB - 03Q | Humber and North Yorkshire ICB - 42D |
|---|---|---|---|---|---|---|---|---|---|
Klebsiella spp. bacteraemia 12-month rolling case counts and rates, by Sub ICB Location (SICBL) and month (Persons All ages) | Jun 2025 | 23.7 | 25.7 | 25.5 | 23.1 | 29.2 | 27.7 | 23.7 | 27.0 |
Klebsiella spp. bacteraemia 12-month rolling case counts and rates of hospital-onset, by Sub ICB Location (SICBL) and month (Persons All ages) | Jun 2025 | 7.3 | 6.7 | 7.8 | 6.3 | 9.5 | 6.5 | 6.1 | 5.6 |
Klebsiella spp. bacteraemia 12-month rolling case counts and rates of community-onset, by Sub ICB Location (SICBL) and month (Persons All ages) | Jun 2025 | 16.4 | 19.0 | 17.8 | 16.8 | 19.7 | 21.2 | 17.6 | 21.4 |
There were four cases of klebsiella spp. infection in Hull for the year May 2016 to April 2017 giving a rate of 1.5 cases per 100,000 population, but this steadily increased to around 40 cases by February 2018 (for the year March 2017 to February 2018) giving a rate of around 15 cases per 100,000 population. The rate gradually increased over quite a long period of time between 20018 and mid-2023 to around 20 cases per 100,000 population although there was a slight decrease in 2020 and early 2021 due to the COVID-19 pandemic. Since mid-2023, the rate has increased in Hull to a high of 30 cases per 100,000 population for March 2024 (for the year April 2023 to March 2024) although there has been reduction to 21 per 100,000 population for April 2025 (for the year May 2024 to April 2025).
Over the period April 2017 to Autumn 2023, the infection rate in Hull has been reasonably similar to England, although since late 2023, the rate in Hull has increased at a faster rate than the increase for England so that the rate in Hull was 30% higher than England for the year April 2023 to March 2024. With the recent decrease in the infection rate in Hull combined with no real change in England, the rate in Hull is lower than England for the latest period May 2024 to April 2025.
The increased rate could be due to increased testing, detection and/or recording of klebsiella spp. infections over time.
Over the period May 2024 to April 2025, there were 56 cases of klebsiella spp. infection in Hull.
Compared with benchmark
Klebsiella spp. bacteraemia 12-month rolling case counts and rates, by Sub ICB Location (SICBL) and month (Persons All ages)
|
Period
|
Humber and North Yorkshire ICB - 03F |
NHS Humber and North Yorkshire Integrated Care Board - QOQ
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| Apr 2017 | • | 4 | 1.5 | - | - | 2.0 | 1.4 |
| May 2017 | • | 7 | 2.6 | - | - | 4.0 | 2.8 |
| Jun 2017 | • | 10 | 3.8 | - | - | 5.3 | 4.2 |
| Jul 2017 | • | 16 | 6.0 | - | - | 7.7 | 6.0 |
| Aug 2017 | • | 21 | 7.9 | - | - | 9.5 | 7.5 |
| Sep 2017 | • | 23 | 8.6 | - | - | 11.2 | 9.1 |
| Oct 2017 | • | 28 | 10.5 | - | - | 13.1 | 10.7 |
| Nov 2017 | • | 32 | 12.0 | - | - | 15.0 | 12.2 |
| Dec 2017 | • | 36 | 13.5 | - | - | 16.4 | 13.6 |
| Jan 2018 | • | 38 | 14.2 | - | - | 17.8 | 15.0 |
| Feb 2018 | • | 40 | 15.0 | - | - | 19.1 | 16.2 |
| Mar 2018 | • | 42 | 15.7 | - | - | 20.7 | 17.6 |
| Apr 2018 | • | 44 | 16.4 | - | - | 20.8 | 17.7 |
| May 2018 | • | 45 | 16.8 | - | - | 20.7 | 17.8 |
| Jun 2018 | • | 48 | 17.9 | - | - | 21.1 | 17.9 |
| Jul 2018 | • | 46 | 17.2 | - | - | 20.3 | 18.0 |
| Aug 2018 | • | 44 | 16.4 | - | - | 20.2 | 18.1 |
| Sep 2018 | • | 48 | 17.9 | - | - | 20.5 | 18.3 |
| Oct 2018 | • | 48 | 17.9 | - | - | 20.5 | 18.3 |
| Nov 2018 | • | 50 | 18.6 | - | - | 20.3 | 18.4 |
| Dec 2018 | • | 50 | 18.6 | - | - | 20.3 | 18.6 |
| Jan 2019 | • | 52 | 19.4 | - | - | 21.0 | 18.8 |
| Feb 2019 | • | 52 | 19.4 | - | - | 20.8 | 19.0 |
| Mar 2019 | • | 54 | 20.1 | - | - | 20.9 | 19.2 |
| Apr 2019 | • | 52 | 19.4 | - | - | 20.9 | 19.3 |
| May 2019 | • | 52 | 19.4 | - | - | 21.2 | 19.2 |
| Jun 2019 | • | 50 | 18.6 | - | - | 21.6 | 19.1 |
| Jul 2019 | • | 49 | 18.3 | - | - | 22.0 | 19.2 |
| Aug 2019 | • | 53 | 19.8 | - | - | 22.5 | 19.3 |
| Sep 2019 | • | 51 | 19.0 | - | - | 22.6 | 19.3 |
| Oct 2019 | • | 49 | 18.3 | - | - | 22.4 | 19.5 |
| Nov 2019 | • | 49 | 18.3 | - | - | 22.6 | 19.7 |
| Dec 2019 | • | 50 | 18.6 | - | - | 22.9 | 19.7 |
| Jan 2020 | • | 49 | 18.3 | - | - | 22.4 | 19.7 |
| Feb 2020 | • | 50 | 18.6 | - | - | 22.6 | 19.7 |
| Mar 2020 | • | 52 | 19.3 | - | - | 22.3 | 19.6 |
| Apr 2020 | • | 49 | 18.2 | - | - | 21.2 | 19.5 |
| May 2020 | • | 50 | 18.6 | - | - | 20.6 | 19.4 |
| Jun 2020 | • | 46 | 17.1 | - | - | 19.9 | 19.4 |
| Jul 2020 | • | 45 | 16.8 | - | - | 19.7 | 19.3 |
| Aug 2020 | • | 44 | 16.4 | - | - | 19.7 | 19.2 |
| Sep 2020 | • | 46 | 17.1 | - | - | 19.3 | 19.3 |
| Oct 2020 | • | 47 | 17.5 | - | - | 19.9 | 19.2 |
| Nov 2020 | • | 45 | 16.8 | - | - | 19.9 | 19.1 |
| Dec 2020 | • | 45 | 16.8 | - | - | 19.8 | 19.2 |
| Jan 2021 | • | 48 | 17.9 | - | - | 20.4 | 19.5 |
| Feb 2021 | • | 48 | 18.0 | - | - | 20.2 | 19.7 |
| Mar 2021 | • | 45 | 16.9 | - | - | 20.4 | 19.9 |
| Apr 2021 | • | 50 | 18.7 | - | - | 21.5 | 19.9 |
| May 2021 | • | 53 | 19.9 | - | - | 21.7 | 20.0 |
| Jun 2021 | • | 55 | 20.6 | - | - | 21.9 | 20.1 |
| Jul 2021 | • | 57 | 21.4 | - | - | 21.9 | 20.3 |
| Aug 2021 | • | 55 | 20.6 | - | - | 21.6 | 20.3 |
| Sep 2021 | • | 54 | 20.2 | - | - | 22.3 | 20.3 |
| Oct 2021 | • | 54 | 20.2 | - | - | 21.6 | 20.5 |
| Nov 2021 | • | 59 | 22.1 | - | - | 22.3 | 20.7 |
| Dec 2021 | • | 58 | 21.7 | - | - | 22.2 | 20.7 |
| Jan 2022 | • | 55 | 20.6 | - | - | 21.3 | 20.3 |
| Feb 2022 | • | 58 | 21.7 | - | - | 21.7 | 20.1 |
| Mar 2022 | • | 63 | 23.6 | - | - | 22.4 | 20.2 |
| Apr 2022 | • | 60 | 22.5 | - | - | 21.9 | 20.3 |
| May 2022 | • | 57 | 21.3 | - | - | 21.6 | 20.3 |
| Jun 2022 | • | 57 | 21.3 | - | - | 21.6 | 20.3 |
| Jul 2022 | • | 55 | 20.6 | - | - | 21.6 | 20.3 |
| Aug 2022 | • | 61 | 22.8 | - | - | 22.9 | 20.4 |
| Sep 2022 | • | 58 | 21.7 | - | - | 22.4 | 20.5 |
| Oct 2022 | • | 58 | 21.6 | - | - | 22.4 | 20.5 |
| Nov 2022 | • | 51 | 19.0 | - | - | 21.9 | 20.4 |
| Dec 2022 | • | 54 | 20.1 | - | - | 22.2 | 20.4 |
| Jan 2023 | • | 57 | 21.2 | - | - | 22.7 | 20.6 |
| Feb 2023 | • | 55 | 20.5 | - | - | 23.0 | 20.7 |
| Mar 2023 | • | 48 | 17.9 | - | - | 22.4 | 20.7 |
| Apr 2023 | • | 52 | 19.4 | - | - | 23.1 | 20.8 |
| May 2023 | • | 51 | 19.0 | - | - | 23.3 | 21.0 |
| Jun 2023 | • | 54 | 20.1 | - | - | 23.9 | 21.3 |
| Jul 2023 | • | 60 | 22.3 | - | - | 24.1 | 21.5 |
| Aug 2023 | • | 57 | 21.2 | - | - | 23.8 | 21.6 |
| Sep 2023 | • | 61 | 22.7 | - | - | 24.4 | 21.8 |
| Oct 2023 | • | 68 | 25.3 | - | - | 25.2 | 22.0 |
| Nov 2023 | • | 70 | 26.1 | - | - | 25.0 | 22.1 |
| Dec 2023 | • | 72 | 26.8 | - | - | 25.5 | 22.3 |
| Jan 2024 | • | 71 | 26.4 | - | - | 25.8 | 22.4 |
| Feb 2024 | • | 72 | 26.7 | - | - | 25.7 | 22.6 |
| Mar 2024 | • | 80 | 29.7 | - | - | 26.9 | 22.9 |
| Apr 2024 | • | 77 | 28.6 | - | - | 26.2 | 23.1 |
| May 2024 | • | 74 | 27.5 | - | - | 26.4 | 23.2 |
| Jun 2024 | • | 71 | 26.4 | - | - | 26.8 | 23.2 |
| Jul 2024 | • | 66 | 24.5 | - | - | 27.0 | 23.3 |
| Aug 2024 | • | 66 | 24.5 | - | - | 25.9 | 23.4 |
| Sep 2024 | • | 63 | 23.4 | - | - | 26.0 | 23.5 |
| Oct 2024 | • | 62 | 23.0 | - | - | 25.7 | 23.5 |
| Nov 2024 | • | 67 | 24.9 | - | - | 25.8 | 23.5 |
| Dec 2024 | • | 62 | 23.1 | - | - | 26.1 | 23.5 |
| Jan 2025 | • | 63 | 23.4 | - | - | 26.1 | 23.6 |
| Feb 2025 | • | 62 | 23.1 | - | - | 26.6 | 23.7 |
| Mar 2025 | • | 55 | 20.5 | - | - | 25.3 | 23.6 |
| Apr 2025 | • | 56 | 20.9 | - | - | 25.9 | 23.5 |
| May 2025 | • | 57 | 21.3 | - | - | 26.0 | 23.7 |
| Jun 2025 | • | 62 | 23.1 | - | - | 25.7 | 23.7 |
Source: UK Health Security Agency
The number of hospital-onset cases of klebsiella spp. infections has generally been higher in Hull compared to England when examining the 12-month rolling total number of infections.
In the year May 2016 to April 2017, there had been no hospital-onset klebsiella spp. infections in Hull but this has gradually increased in Hull. An increase has also been observed for England and the region, and it is possible that the increase is associated with better testing, detection and/or recording of klebsiella spp. infections over time.
The infection rate has shown considerably month-to-month variability over time, but since the end of 2017, the hospital-onset infection rate in Hull has generally been higher than England except for mid-2023 and the most recent few months.
The rate in Hull reached a peak of 10 cases per 100,000 population for the year April 2023 to March 2024 with a total of 27 cases, but the rate has decreased since then to 6.3 cases per 100,000 population for the latest period May 2024 to April 2025.
In the last 10 months, the infection rate in Hull has been lower than in England.
There have bee 17 hospital-onset cases of klebsiella spp. infections in Hull over the year May 2024 to April 2025.
Compared with benchmark
Klebsiella spp. bacteraemia 12-month rolling case counts and rates of hospital-onset, by Sub ICB Location (SICBL) and month (Persons All ages)
|
Period
|
Humber and North Yorkshire ICB - 03F |
NHS Humber and North Yorkshire Integrated Care Board - QOQ
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| Apr 2017 | • | - | 0.0 | - | - | 0.5 | 0.4 |
| May 2017 | • | - | 0.0 | - | - | 1.0 | 0.8 |
| Jun 2017 | • | 2 | 0.8 | - | - | 1.4 | 1.2 |
| Jul 2017 | • | 2 | 0.8 | - | - | 2.0 | 1.7 |
| Aug 2017 | • | 4 | 1.5 | - | - | 2.3 | 2.2 |
| Sep 2017 | • | 5 | 1.9 | - | - | 2.7 | 2.6 |
| Oct 2017 | • | 8 | 3.0 | - | - | 3.4 | 3.1 |
| Nov 2017 | • | 12 | 4.5 | - | - | 4.0 | 3.6 |
| Dec 2017 | • | 14 | 5.2 | - | - | 4.3 | 4.0 |
| Jan 2018 | • | 15 | 5.6 | - | - | 4.8 | 4.5 |
| Feb 2018 | • | 16 | 6.0 | - | - | 5.0 | 4.8 |
| Mar 2018 | • | 16 | 6.0 | - | - | 5.5 | 5.3 |
| Apr 2018 | • | 17 | 6.3 | - | - | 5.7 | 5.3 |
| May 2018 | • | 18 | 6.7 | - | - | 5.9 | 5.3 |
| Jun 2018 | • | 18 | 6.7 | - | - | 5.9 | 5.4 |
| Jul 2018 | • | 20 | 7.5 | - | - | 5.7 | 5.4 |
| Aug 2018 | • | 18 | 6.7 | - | - | 5.9 | 5.4 |
| Sep 2018 | • | 20 | 7.5 | - | - | 6.0 | 5.6 |
| Oct 2018 | • | 17 | 6.3 | - | - | 5.7 | 5.6 |
| Nov 2018 | • | 16 | 6.0 | - | - | 5.5 | 5.6 |
| Dec 2018 | • | 18 | 6.7 | - | - | 5.8 | 5.7 |
| Jan 2019 | • | 19 | 7.1 | - | - | 5.9 | 5.6 |
| Feb 2019 | • | 19 | 7.1 | - | - | 5.8 | 5.7 |
| Mar 2019 | • | 20 | 7.5 | - | - | 5.7 | 5.7 |
| Apr 2019 | • | 21 | 7.8 | - | - | 5.7 | 5.8 |
| May 2019 | • | 21 | 7.8 | - | - | 5.4 | 5.8 |
| Jun 2019 | • | 21 | 7.8 | - | - | 5.4 | 5.8 |
| Jul 2019 | • | 20 | 7.5 | - | - | 5.4 | 5.7 |
| Aug 2019 | • | 23 | 8.6 | - | - | 5.6 | 5.8 |
| Sep 2019 | • | 22 | 8.2 | - | - | 5.8 | 5.7 |
| Oct 2019 | • | 23 | 8.6 | - | - | 5.7 | 5.7 |
| Nov 2019 | • | 23 | 8.6 | - | - | 5.8 | 5.8 |
| Dec 2019 | • | 22 | 8.2 | - | - | 5.7 | 5.8 |
| Jan 2020 | • | 20 | 7.5 | - | - | 5.4 | 5.8 |
| Feb 2020 | • | 21 | 7.8 | - | - | 5.8 | 5.8 |
| Mar 2020 | • | 22 | 8.2 | - | - | 5.8 | 5.7 |
| Apr 2020 | • | 20 | 7.4 | - | - | 5.4 | 5.8 |
| May 2020 | • | 19 | 7.1 | - | - | 5.2 | 5.8 |
| Jun 2020 | • | 17 | 6.3 | - | - | 5.1 | 5.8 |
| Jul 2020 | • | 16 | 6.0 | - | - | 5.2 | 5.7 |
| Aug 2020 | • | 14 | 5.2 | - | - | 5.2 | 5.6 |
| Sep 2020 | • | 13 | 4.8 | - | - | 4.9 | 5.6 |
| Oct 2020 | • | 14 | 5.2 | - | - | 5.1 | 5.7 |
| Nov 2020 | • | 13 | 4.9 | - | - | 5.3 | 5.8 |
| Dec 2020 | • | 14 | 5.2 | - | - | 5.2 | 5.9 |
| Jan 2021 | • | 18 | 6.7 | - | - | 5.3 | 6.4 |
| Feb 2021 | • | 18 | 6.7 | - | - | 5.4 | 6.6 |
| Mar 2021 | • | 16 | 6.0 | - | - | 5.1 | 6.7 |
| Apr 2021 | • | 16 | 6.0 | - | - | 5.5 | 6.6 |
| May 2021 | • | 17 | 6.4 | - | - | 5.7 | 6.7 |
| Jun 2021 | • | 17 | 6.4 | - | - | 5.7 | 6.7 |
| Jul 2021 | • | 19 | 7.1 | - | - | 5.8 | 6.9 |
| Aug 2021 | • | 20 | 7.5 | - | - | 6.0 | 7.0 |
| Sep 2021 | • | 21 | 7.9 | - | - | 6.1 | 7.1 |
| Oct 2021 | • | 19 | 7.1 | - | - | 6.2 | 7.2 |
| Nov 2021 | • | 21 | 7.9 | - | - | 6.4 | 7.2 |
| Dec 2021 | • | 19 | 7.1 | - | - | 6.5 | 7.2 |
| Jan 2022 | • | 17 | 6.4 | - | - | 6.5 | 6.8 |
| Feb 2022 | • | 16 | 6.0 | - | - | 6.3 | 6.6 |
| Mar 2022 | • | 20 | 7.5 | - | - | 6.5 | 6.5 |
| Apr 2022 | • | 22 | 8.2 | - | - | 6.5 | 6.6 |
| May 2022 | • | 25 | 9.4 | - | - | 6.9 | 6.6 |
| Jun 2022 | • | 25 | 9.3 | - | - | 7.0 | 6.7 |
| Jul 2022 | • | 24 | 9.0 | - | - | 7.1 | 6.6 |
| Aug 2022 | • | 26 | 9.7 | - | - | 7.5 | 6.7 |
| Sep 2022 | • | 24 | 9.0 | - | - | 7.6 | 6.7 |
| Oct 2022 | • | 25 | 9.3 | - | - | 7.5 | 6.7 |
| Nov 2022 | • | 21 | 7.8 | - | - | 7.2 | 6.7 |
| Dec 2022 | • | 21 | 7.8 | - | - | 7.4 | 6.7 |
| Jan 2023 | • | 21 | 7.8 | - | - | 7.2 | 6.8 |
| Feb 2023 | • | 21 | 7.8 | - | - | 7.3 | 6.8 |
| Mar 2023 | • | 17 | 6.3 | - | - | 7.3 | 6.9 |
| Apr 2023 | • | 17 | 6.3 | - | - | 7.5 | 6.9 |
| May 2023 | • | 14 | 5.2 | - | - | 7.2 | 6.8 |
| Jun 2023 | • | 18 | 6.7 | - | - | 7.5 | 6.9 |
| Jul 2023 | • | 19 | 7.1 | - | - | 7.2 | 6.9 |
| Aug 2023 | • | 17 | 6.3 | - | - | 6.9 | 6.9 |
| Sep 2023 | • | 21 | 7.8 | - | - | 7.0 | 6.9 |
| Oct 2023 | • | 21 | 7.8 | - | - | 7.3 | 6.9 |
| Nov 2023 | • | 23 | 8.6 | - | - | 7.3 | 6.9 |
| Dec 2023 | • | 22 | 8.2 | - | - | 7.2 | 6.9 |
| Jan 2024 | • | 20 | 7.4 | - | - | 7.2 | 6.8 |
| Feb 2024 | • | 23 | 8.5 | - | - | 7.5 | 6.9 |
| Mar 2024 | • | 27 | 10.0 | - | - | 8.0 | 7.0 |
| Apr 2024 | • | 25 | 9.3 | - | - | 7.4 | 7.0 |
| May 2024 | • | 24 | 8.9 | - | - | 7.5 | 7.1 |
| Jun 2024 | • | 21 | 7.8 | - | - | 7.3 | 7.2 |
| Jul 2024 | • | 19 | 7.1 | - | - | 7.5 | 7.2 |
| Aug 2024 | • | 18 | 6.7 | - | - | 6.9 | 7.2 |
| Sep 2024 | • | 14 | 5.2 | - | - | 6.8 | 7.3 |
| Oct 2024 | • | 15 | 5.6 | - | - | 6.5 | 7.3 |
| Nov 2024 | • | 15 | 5.6 | - | - | 6.3 | 7.2 |
| Dec 2024 | • | 15 | 5.6 | - | - | 6.4 | 7.2 |
| Jan 2025 | • | 18 | 6.7 | - | - | 6.8 | 7.3 |
| Feb 2025 | • | 16 | 6.0 | - | - | 6.6 | 7.3 |
| Mar 2025 | • | 14 | 5.2 | - | - | 6.2 | 7.3 |
| Apr 2025 | • | 17 | 6.3 | - | - | 6.8 | 7.3 |
| May 2025 | • | 18 | 6.7 | - | - | 6.7 | 7.4 |
| Jun 2025 | • | 17 | 6.3 | - | - | 6.7 | 7.3 |
Source: UK Health Security Agency
The number of community-onset cases of klebsiella spp. infections as shown a similar pattern to that for hospital-onset cases, and it is again possible that the increase is due to better testing, detection and/or recording over time.
The community-onset klebsiella spp. infection rate was generally been lower in Hull compared to England until mid-2023.
Since then, the rate in Hull has increased quite sharply compared to only a small increase for England and the rate has been higher than England between July 2023 (year August 2022 to July 2023) and February 2025 (year March 2024 to February 2025). In the last two months, the 12 month rolling average number of cases in Hull has decreased and is slightly lower than England for the latest period May 2024 to April 2025.
Over the year May 2024 to April 2025, there were 39 klebsiella spp. infections in Hull that were community-onset.
Compared with benchmark
Klebsiella spp. bacteraemia 12-month rolling case counts and rates of community-onset, by Sub ICB Location (SICBL) and month (Persons All ages)
|
Period
|
Humber and North Yorkshire ICB - 03F |
NHS Humber and North Yorkshire Integrated Care Board - QOQ
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| Apr 2017 | • | 4 | 1.5 | - | - | 1.5 | 1.0 |
| May 2017 | • | 7 | 2.6 | - | - | 3.0 | 2.0 |
| Jun 2017 | • | 8 | 3.0 | - | - | 3.9 | 3.0 |
| Jul 2017 | • | 14 | 5.3 | - | - | 5.6 | 4.2 |
| Aug 2017 | • | 17 | 6.4 | - | - | 7.2 | 5.3 |
| Sep 2017 | • | 18 | 6.8 | - | - | 8.5 | 6.4 |
| Oct 2017 | • | 20 | 7.5 | - | - | 9.7 | 7.6 |
| Nov 2017 | • | 20 | 7.5 | - | - | 11.0 | 8.6 |
| Dec 2017 | • | 22 | 8.2 | - | - | 12.2 | 9.6 |
| Jan 2018 | • | 23 | 8.6 | - | - | 13.0 | 10.5 |
| Feb 2018 | • | 24 | 9.0 | - | - | 14.1 | 11.4 |
| Mar 2018 | • | 26 | 9.7 | - | - | 15.2 | 12.3 |
| Apr 2018 | • | 27 | 10.1 | - | - | 15.2 | 12.4 |
| May 2018 | • | 27 | 10.1 | - | - | 14.8 | 12.5 |
| Jun 2018 | • | 30 | 11.2 | - | - | 15.2 | 12.6 |
| Jul 2018 | • | 26 | 9.7 | - | - | 14.6 | 12.6 |
| Aug 2018 | • | 26 | 9.7 | - | - | 14.3 | 12.7 |
| Sep 2018 | • | 28 | 10.4 | - | - | 14.4 | 12.7 |
| Oct 2018 | • | 31 | 11.6 | - | - | 14.8 | 12.6 |
| Nov 2018 | • | 34 | 12.7 | - | - | 14.8 | 12.8 |
| Dec 2018 | • | 32 | 11.9 | - | - | 14.5 | 12.9 |
| Jan 2019 | • | 33 | 12.3 | - | - | 15.1 | 13.2 |
| Feb 2019 | • | 33 | 12.3 | - | - | 15.0 | 13.3 |
| Mar 2019 | • | 34 | 12.7 | - | - | 15.2 | 13.4 |
| Apr 2019 | • | 31 | 11.6 | - | - | 15.1 | 13.5 |
| May 2019 | • | 31 | 11.6 | - | - | 15.8 | 13.5 |
| Jun 2019 | • | 29 | 10.8 | - | - | 16.1 | 13.4 |
| Jul 2019 | • | 29 | 10.8 | - | - | 16.6 | 13.4 |
| Aug 2019 | • | 30 | 11.2 | - | - | 16.9 | 13.5 |
| Sep 2019 | • | 29 | 10.8 | - | - | 16.8 | 13.6 |
| Oct 2019 | • | 26 | 9.7 | - | - | 16.7 | 13.8 |
| Nov 2019 | • | 26 | 9.7 | - | - | 16.8 | 13.9 |
| Dec 2019 | • | 28 | 10.4 | - | - | 17.3 | 13.9 |
| Jan 2020 | • | 29 | 10.8 | - | - | 17.0 | 13.9 |
| Feb 2020 | • | 29 | 10.8 | - | - | 16.8 | 13.9 |
| Mar 2020 | • | 30 | 11.2 | - | - | 16.4 | 13.9 |
| Apr 2020 | • | 29 | 10.8 | - | - | 15.8 | 13.7 |
| May 2020 | • | 31 | 11.5 | - | - | 15.4 | 13.6 |
| Jun 2020 | • | 29 | 10.8 | - | - | 14.8 | 13.7 |
| Jul 2020 | • | 29 | 10.8 | - | - | 14.5 | 13.6 |
| Aug 2020 | • | 30 | 11.2 | - | - | 14.6 | 13.6 |
| Sep 2020 | • | 33 | 12.3 | - | - | 14.4 | 13.6 |
| Oct 2020 | • | 33 | 12.3 | - | - | 14.9 | 13.5 |
| Nov 2020 | • | 32 | 11.9 | - | - | 14.6 | 13.3 |
| Dec 2020 | • | 31 | 11.6 | - | - | 14.5 | 13.3 |
| Jan 2021 | • | 30 | 11.2 | - | - | 15.1 | 13.1 |
| Feb 2021 | • | 30 | 11.2 | - | - | 14.8 | 13.1 |
| Mar 2021 | • | 29 | 10.9 | - | - | 15.3 | 13.1 |
| Apr 2021 | • | 34 | 12.7 | - | - | 16.0 | 13.3 |
| May 2021 | • | 36 | 13.5 | - | - | 16.1 | 13.4 |
| Jun 2021 | • | 38 | 14.2 | - | - | 16.2 | 13.4 |
| Jul 2021 | • | 38 | 14.2 | - | - | 16.1 | 13.4 |
| Aug 2021 | • | 35 | 13.1 | - | - | 15.6 | 13.3 |
| Sep 2021 | • | 33 | 12.4 | - | - | 16.2 | 13.2 |
| Oct 2021 | • | 35 | 13.1 | - | - | 15.4 | 13.3 |
| Nov 2021 | • | 38 | 14.2 | - | - | 15.9 | 13.5 |
| Dec 2021 | • | 39 | 14.6 | - | - | 15.7 | 13.5 |
| Jan 2022 | • | 38 | 14.2 | - | - | 14.8 | 13.5 |
| Feb 2022 | • | 42 | 15.7 | - | - | 15.4 | 13.6 |
| Mar 2022 | • | 43 | 16.1 | - | - | 16.0 | 13.6 |
| Apr 2022 | • | 38 | 14.2 | - | - | 15.4 | 13.6 |
| May 2022 | • | 32 | 12.0 | - | - | 14.8 | 13.7 |
| Jun 2022 | • | 32 | 12.0 | - | - | 14.6 | 13.7 |
| Jul 2022 | • | 31 | 11.6 | - | - | 14.5 | 13.7 |
| Aug 2022 | • | 35 | 13.1 | - | - | 15.4 | 13.8 |
| Sep 2022 | • | 34 | 12.7 | - | - | 14.9 | 13.8 |
| Oct 2022 | • | 33 | 12.3 | - | - | 14.9 | 13.8 |
| Nov 2022 | • | 30 | 11.2 | - | - | 14.7 | 13.8 |
| Dec 2022 | • | 33 | 12.3 | - | - | 14.8 | 13.7 |
| Jan 2023 | • | 36 | 13.4 | - | - | 15.5 | 13.8 |
| Feb 2023 | • | 34 | 12.7 | - | - | 15.7 | 13.9 |
| Mar 2023 | • | 31 | 11.5 | - | - | 15.1 | 13.8 |
| Apr 2023 | • | 35 | 13.0 | - | - | 15.6 | 14.0 |
| May 2023 | • | 37 | 13.8 | - | - | 16.1 | 14.1 |
| Jun 2023 | • | 36 | 13.4 | - | - | 16.4 | 14.4 |
| Jul 2023 | • | 41 | 15.3 | - | - | 16.9 | 14.6 |
| Aug 2023 | • | 40 | 14.9 | - | - | 16.8 | 14.7 |
| Sep 2023 | • | 40 | 14.9 | - | - | 17.3 | 14.9 |
| Oct 2023 | • | 47 | 17.5 | - | - | 17.9 | 15.1 |
| Nov 2023 | • | 47 | 17.5 | - | - | 17.7 | 15.2 |
| Dec 2023 | • | 50 | 18.6 | - | - | 18.3 | 15.4 |
| Jan 2024 | • | 51 | 19.0 | - | - | 18.6 | 15.6 |
| Feb 2024 | • | 49 | 18.2 | - | - | 18.2 | 15.6 |
| Mar 2024 | • | 53 | 19.7 | - | - | 18.8 | 15.9 |
| Apr 2024 | • | 52 | 19.3 | - | - | 18.8 | 16.0 |
| May 2024 | • | 50 | 18.6 | - | - | 18.9 | 16.0 |
| Jun 2024 | • | 50 | 18.6 | - | - | 19.5 | 16.0 |
| Jul 2024 | • | 47 | 17.5 | - | - | 19.6 | 16.1 |
| Aug 2024 | • | 48 | 17.8 | - | - | 19.1 | 16.1 |
| Sep 2024 | • | 49 | 18.2 | - | - | 19.2 | 16.2 |
| Oct 2024 | • | 47 | 17.5 | - | - | 19.2 | 16.2 |
| Nov 2024 | • | 52 | 19.3 | - | - | 19.5 | 16.3 |
| Dec 2024 | • | 47 | 17.5 | - | - | 19.7 | 16.3 |
| Jan 2025 | • | 45 | 16.7 | - | - | 19.4 | 16.3 |
| Feb 2025 | • | 46 | 17.2 | - | - | 20.0 | 16.4 |
| Mar 2025 | • | 41 | 15.3 | - | - | 19.1 | 16.2 |
| Apr 2025 | • | 39 | 14.5 | - | - | 19.1 | 16.2 |
| May 2025 | • | 39 | 14.5 | - | - | 19.2 | 16.3 |
| Jun 2025 | • | 45 | 16.8 | - | - | 19.0 | 16.4 |
Source: UK Health Security Agency
Pseudomonas Aeruginosa (P. Aeruginosa) Bacteraemia
Cases by Financial Year
The rate of P. aeruginosa bacteraemia infections in Hull (03F) was higher than England for 2023/24 both overall and for community-onset cases. The number of cases of infection are relatively small.
Compared with benchmark
| Indicator | Period | England | NHS Humber and North Yorkshire Integrated Care Board - QOQ | Humber and North Yorkshire ICB - 02Y | Humber and North Yorkshire ICB - 03F | Humber and North Yorkshire ICB - 03H | Humber and North Yorkshire ICB - 03K | Humber and North Yorkshire ICB - 03Q | Humber and North Yorkshire ICB - 42D |
|---|---|---|---|---|---|---|---|---|---|
P. aeruginosa bacteraemia case counts and rates, by sub ICB location (SICBL) and financial year (Persons All ages) | 2023/24 | 7.8 | 8.4 | 10.9 | 10.0 | 8.2 | 7.6 | 5.7 | 8.4 |
P. aeruginosa bacteraemia case counts and rates of community-onset, by sub ICB location (SICBL) and financial year (Persons All ages) | 2023/24 | 4.8 | 5.4 | 5.6 | 5.6 | 5.7 | 5.9 | 4.4 | 5.6 |
| Indicator | Period | England | NHS Humber and North Yorkshire Integrated Care Board - QOQ | Humber and North Yorkshire ICB - 02Y | Humber and North Yorkshire ICB - 03F | Humber and North Yorkshire ICB - 03H | Humber and North Yorkshire ICB - 03K | Humber and North Yorkshire ICB - 03Q | Humber and North Yorkshire ICB - 42D |
|---|---|---|---|---|---|---|---|---|---|
P. aeruginosa bacteraemia case counts and rates, by sub ICB location (SICBL) and financial year (Persons All ages) | 2023/24 | 7.8 | 8.4 | 10.9 | 10.0 | 8.2 | 7.6 | 5.7 | 8.4 |
P. aeruginosa bacteraemia case counts and rates of community-onset, by sub ICB location (SICBL) and financial year (Persons All ages) | 2023/24 | 4.8 | 5.4 | 5.6 | 5.6 | 5.7 | 5.9 | 4.4 | 5.6 |
There has been year-on-year variability in the P. aeruginosa infection rate in Hull, but in general the rate has been higher in Hull than England.
During 2023/24, there were relatively few cases of P. aeruginosa in Hull with 27 in total over the year.
Compared with benchmark
P. aeruginosa bacteraemia case counts and rates, by sub ICB location (SICBL) and financial year (Persons All ages)
|
Period
|
Humber and North Yorkshire ICB - 03F |
NHS Humber and North Yorkshire Integrated Care Board - QOQ
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2017/18 | • | 23 | 8.8 | - | - | 8.6 | 7.7 |
| 2018/19 | • | 22 | 8.4 | - | - | 8.4 | 7.5 |
| 2019/20 | • | 26 | 10.0 | - | - | 9.7 | 7.7 |
| 2020/21 | • | 20 | 7.7 | - | - | 7.3 | 7.6 |
| 2021/22 | • | 18 | 6.7 | - | - | 9.3 | 7.7 |
| 2022/23 | • | 25 | 9.3 | - | - | 8.6 | 7.7 |
| 2023/24 | • | 27 | 10.0 | - | - | 8.4 | 7.8 |
Source: UK Health Security Agency
There has been year-on-year variability in the community-onset P. aeruginosa infection rate in Hull, but in general the rate has been higher in Hull than England.
During 2023/24, there were only 15 cases of P. aeruginosa in Hull that were community-onset so the number of cases is relatively small.
Compared with benchmark
P. aeruginosa bacteraemia case counts and rates of community-onset, by sub ICB location (SICBL) and financial year (Persons All ages)
|
Period
|
Humber and North Yorkshire ICB - 03F |
NHS Humber and North Yorkshire Integrated Care Board - QOQ
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2017/18 | • | 14 | 5.4 | - | - | 5.1 | 4.8 |
| 2018/19 | • | 16 | 6.1 | - | - | 5.2 | 4.8 |
| 2019/20 | • | 16 | 6.2 | - | - | 6.3 | 4.9 |
| 2020/21 | • | 10 | 3.8 | - | - | 4.8 | 4.6 |
| 2021/22 | • | 11 | 4.1 | - | - | 6.0 | 4.8 |
| 2022/23 | • | 17 | 6.3 | - | - | 5.6 | 4.7 |
| 2023/24 | • | 15 | 5.6 | - | - | 5.4 | 4.8 |
Source: UK Health Security Agency
Cases by Month (12-Month Rolling Total)
For the year to April 2025, the number of hospital-onset cases of P. aeruginosa has been higher in Hull compared to England, but the number of community-onset cases has been lower. The number of cases overall at 7.8 cases per 100,000 population for May 2024 to April 2025 is the same for Hull as it is for England.
Compared with benchmark
| Indicator | Period | England | NHS Humber and North Yorkshire Integrated Care Board - QOQ | Humber and North Yorkshire ICB - 02Y | Humber and North Yorkshire ICB - 03F | Humber and North Yorkshire ICB - 03H | Humber and North Yorkshire ICB - 03K | Humber and North Yorkshire ICB - 03Q | Humber and North Yorkshire ICB - 42D |
|---|---|---|---|---|---|---|---|---|---|
P. aeruginosa bacteraemia 12-month rolling case counts and rates, by Sub ICB Location (SICBL) and month (Persons All ages) | Jun 2025 | 7.8 | 8.3 | 7.8 | 7.8 | 8.9 | 7.1 | 9.1 | 8.6 |
P. aeruginosa bacteraemia 12-month rolling case counts and rates of hospital-onset, by Sub ICB Location (SICBL) and month (Persons All ages) | Jun 2025 | 2.9 | 2.6 | 2.8 | 4.1 | 2.5 | 2.9 | 1.4 | 2.3 |
P. aeruginosa bacteraemia 12-month rolling case counts and rates of community-onset, by Sub ICB Location (SICBL) and month (Persons All ages) | Jun 2025 | 4.9 | 5.7 | 5.0 | 3.7 | 6.4 | 4.1 | 7.7 | 6.3 |
| Indicator | Period | England | NHS Humber and North Yorkshire Integrated Care Board - QOQ | Humber and North Yorkshire ICB - 02Y | Humber and North Yorkshire ICB - 03F | Humber and North Yorkshire ICB - 03H | Humber and North Yorkshire ICB - 03K | Humber and North Yorkshire ICB - 03Q | Humber and North Yorkshire ICB - 42D |
|---|---|---|---|---|---|---|---|---|---|
P. aeruginosa bacteraemia 12-month rolling case counts and rates, by Sub ICB Location (SICBL) and month (Persons All ages) | Jun 2025 | 7.8 | 8.3 | 7.8 | 7.8 | 8.9 | 7.1 | 9.1 | 8.6 |
P. aeruginosa bacteraemia 12-month rolling case counts and rates of hospital-onset, by Sub ICB Location (SICBL) and month (Persons All ages) | Jun 2025 | 2.9 | 2.6 | 2.8 | 4.1 | 2.5 | 2.9 | 1.4 | 2.3 |
P. aeruginosa bacteraemia 12-month rolling case counts and rates of community-onset, by Sub ICB Location (SICBL) and month (Persons All ages) | Jun 2025 | 4.9 | 5.7 | 5.0 | 3.7 | 6.4 | 4.1 | 7.7 | 6.3 |
The number of cases of P. aeruginosa showed a steady increase from the year May 2016 to April 2017 to the year April 2018 to March 2019 for both Hull and England with the rate in Hull increasing from 0.8 to 8.8 per 100,000 population. The increased rate could be due to increased testing, detection and/or recording of P. aeruginosa infections over time.
The rate remained relatively constant for England at just under eight cases per 100,000 population, but for Hull the infection rate has been more variable ranging from 6.5 to 11.9 cases per 100,000 population. The rate in Hull has generally been higher than England with the exception of 2022 where the rate in Hull was lower. Since a low of 5.6 cases per 100,o00 population for the year November 2021 to October 2022 in Hull, the rate in Hull increased sharply to 11.9 cases per 100,000 population for the year October 2022 to September 2023. Since then the rate has varied from around 9 to 11 cases per 100,000 population but has been slightly lower the last two months with 7.8 cases in the latest period May 2024 to April 2025.
For the latest period May 2024 to April 2025, there were only 21 cases of P. aeruginosa in Hull so the number of cases is relatively small.
Compared with benchmark
P. aeruginosa bacteraemia 12-month rolling case counts and rates, by Sub ICB Location (SICBL) and month (Persons All ages)
|
Period
|
Humber and North Yorkshire ICB - 03F |
NHS Humber and North Yorkshire Integrated Care Board - QOQ
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| Apr 2017 | • | 2 | 0.8 | - | - | 0.7 | 0.5 |
| May 2017 | • | 4 | 1.5 | - | - | 1.5 | 1.2 |
| Jun 2017 | • | 7 | 2.6 | - | - | 2.0 | 1.8 |
| Jul 2017 | • | 9 | 3.4 | - | - | 2.9 | 2.5 |
| Aug 2017 | • | 11 | 4.1 | - | - | 3.2 | 3.3 |
| Sep 2017 | • | 15 | 5.6 | - | - | 4.5 | 4.0 |
| Oct 2017 | • | 18 | 6.7 | - | - | 5.6 | 4.7 |
| Nov 2017 | • | 19 | 7.1 | - | - | 6.3 | 5.4 |
| Dec 2017 | • | 20 | 7.5 | - | - | 6.8 | 6.0 |
| Jan 2018 | • | 20 | 7.5 | - | - | 7.5 | 6.7 |
| Feb 2018 | • | 22 | 8.2 | - | - | 8.2 | 7.2 |
| Mar 2018 | • | 23 | 8.6 | - | - | 8.6 | 7.7 |
| Apr 2018 | • | 22 | 8.2 | - | - | 8.5 | 7.8 |
| May 2018 | • | 21 | 7.8 | - | - | 8.3 | 7.7 |
| Jun 2018 | • | 19 | 7.1 | - | - | 8.3 | 7.6 |
| Jul 2018 | • | 18 | 6.7 | - | - | 8.0 | 7.6 |
| Aug 2018 | • | 20 | 7.5 | - | - | 8.3 | 7.6 |
| Sep 2018 | • | 18 | 6.7 | - | - | 8.2 | 7.6 |
| Oct 2018 | • | 17 | 6.3 | - | - | 8.0 | 7.6 |
| Nov 2018 | • | 18 | 6.7 | - | - | 8.0 | 7.5 |
| Dec 2018 | • | 21 | 7.8 | - | - | 8.5 | 7.5 |
| Jan 2019 | • | 24 | 8.9 | - | - | 8.7 | 7.5 |
| Feb 2019 | • | 22 | 8.2 | - | - | 8.4 | 7.5 |
| Mar 2019 | • | 22 | 8.2 | - | - | 8.5 | 7.5 |
| Apr 2019 | • | 23 | 8.6 | - | - | 8.3 | 7.5 |
| May 2019 | • | 24 | 8.9 | - | - | 8.6 | 7.6 |
| Jun 2019 | • | 25 | 9.3 | - | - | 9.5 | 7.6 |
| Jul 2019 | • | 27 | 10.1 | - | - | 10.5 | 7.7 |
| Aug 2019 | • | 24 | 8.9 | - | - | 10.6 | 7.7 |
| Sep 2019 | • | 26 | 9.7 | - | - | 10.2 | 7.7 |
| Oct 2019 | • | 28 | 10.4 | - | - | 10.2 | 7.6 |
| Nov 2019 | • | 28 | 10.4 | - | - | 10.2 | 7.7 |
| Dec 2019 | • | 26 | 9.7 | - | - | 10.0 | 7.7 |
| Jan 2020 | • | 25 | 9.3 | - | - | 9.8 | 7.7 |
| Feb 2020 | • | 26 | 9.7 | - | - | 9.7 | 7.8 |
| Mar 2020 | • | 26 | 9.7 | - | - | 9.7 | 7.7 |
| Apr 2020 | • | 24 | 8.9 | - | - | 9.7 | 7.7 |
| May 2020 | • | 24 | 8.9 | - | - | 9.3 | 7.5 |
| Jun 2020 | • | 24 | 8.9 | - | - | 8.4 | 7.4 |
| Jul 2020 | • | 22 | 8.2 | - | - | 7.8 | 7.4 |
| Aug 2020 | • | 25 | 9.3 | - | - | 7.5 | 7.3 |
| Sep 2020 | • | 24 | 8.9 | - | - | 7.8 | 7.4 |
| Oct 2020 | • | 21 | 7.8 | - | - | 7.2 | 7.4 |
| Nov 2020 | • | 20 | 7.5 | - | - | 7.3 | 7.4 |
| Dec 2020 | • | 20 | 7.5 | - | - | 7.1 | 7.4 |
| Jan 2021 | • | 19 | 7.1 | - | - | 7.0 | 7.5 |
| Feb 2021 | • | 20 | 7.5 | - | - | 7.2 | 7.5 |
| Mar 2021 | • | 20 | 7.5 | - | - | 7.3 | 7.6 |
| Apr 2021 | • | 22 | 8.2 | - | - | 7.6 | 7.7 |
| May 2021 | • | 22 | 8.2 | - | - | 8.0 | 7.7 |
| Jun 2021 | • | 22 | 8.2 | - | - | 8.0 | 7.8 |
| Jul 2021 | • | 22 | 8.2 | - | - | 8.0 | 7.8 |
| Aug 2021 | • | 20 | 7.5 | - | - | 8.3 | 7.9 |
| Sep 2021 | • | 18 | 6.7 | - | - | 8.0 | 7.9 |
| Oct 2021 | • | 22 | 8.2 | - | - | 9.1 | 8.0 |
| Nov 2021 | • | 21 | 7.9 | - | - | 8.9 | 7.9 |
| Dec 2021 | • | 21 | 7.9 | - | - | 9.0 | 7.9 |
| Jan 2022 | • | 20 | 7.5 | - | - | 9.1 | 7.8 |
| Feb 2022 | • | 19 | 7.1 | - | - | 9.2 | 7.7 |
| Mar 2022 | • | 18 | 6.7 | - | - | 9.3 | 7.7 |
| Apr 2022 | • | 16 | 6.0 | - | - | 9.2 | 7.6 |
| May 2022 | • | 18 | 6.7 | - | - | 9.4 | 7.7 |
| Jun 2022 | • | 17 | 6.4 | - | - | 9.4 | 7.7 |
| Jul 2022 | • | 17 | 6.4 | - | - | 9.1 | 7.6 |
| Aug 2022 | • | 17 | 6.3 | - | - | 9.0 | 7.5 |
| Sep 2022 | • | 16 | 6.0 | - | - | 8.7 | 7.5 |
| Oct 2022 | • | 15 | 5.6 | - | - | 8.2 | 7.6 |
| Nov 2022 | • | 18 | 6.7 | - | - | 8.4 | 7.6 |
| Dec 2022 | • | 22 | 8.2 | - | - | 9.1 | 7.6 |
| Jan 2023 | • | 24 | 8.9 | - | - | 9.2 | 7.6 |
| Feb 2023 | • | 25 | 9.3 | - | - | 9.1 | 7.7 |
| Mar 2023 | • | 25 | 9.3 | - | - | 8.6 | 7.7 |
| Apr 2023 | • | 27 | 10.0 | - | - | 8.6 | 7.8 |
| May 2023 | • | 26 | 9.7 | - | - | 8.5 | 7.8 |
| Jun 2023 | • | 28 | 10.4 | - | - | 8.6 | 7.8 |
| Jul 2023 | • | 31 | 11.5 | - | - | 8.8 | 7.9 |
| Aug 2023 | • | 30 | 11.2 | - | - | 8.8 | 7.8 |
| Sep 2023 | • | 32 | 11.9 | - | - | 8.9 | 7.8 |
| Oct 2023 | • | 29 | 10.8 | - | - | 8.9 | 7.8 |
| Nov 2023 | • | 27 | 10.1 | - | - | 8.5 | 7.8 |
| Dec 2023 | • | 23 | 8.6 | - | - | 7.8 | 7.8 |
| Jan 2024 | • | 24 | 8.9 | - | - | 7.9 | 7.8 |
| Feb 2024 | • | 23 | 8.5 | - | - | 8.0 | 7.8 |
| Mar 2024 | • | 27 | 10.0 | - | - | 8.4 | 7.8 |
| Apr 2024 | • | 28 | 10.4 | - | - | 8.7 | 7.8 |
| May 2024 | • | 26 | 9.7 | - | - | 8.4 | 7.8 |
| Jun 2024 | • | 25 | 9.3 | - | - | 8.6 | 7.8 |
| Jul 2024 | • | 24 | 8.9 | - | - | 8.9 | 7.8 |
| Aug 2024 | • | 24 | 8.9 | - | - | 9.2 | 7.8 |
| Sep 2024 | • | 24 | 8.9 | - | - | 9.5 | 7.9 |
| Oct 2024 | • | 25 | 9.3 | - | - | 9.6 | 8.0 |
| Nov 2024 | • | 25 | 9.3 | - | - | 9.5 | 7.9 |
| Dec 2024 | • | 29 | 10.8 | - | - | 9.9 | 8.0 |
| Jan 2025 | • | 28 | 10.4 | - | - | 9.4 | 8.0 |
| Feb 2025 | • | 27 | 10.1 | - | - | 9.2 | 7.8 |
| Mar 2025 | • | 23 | 8.6 | - | - | 9.2 | 7.8 |
| Apr 2025 | • | 21 | 7.8 | - | - | 9.0 | 7.9 |
| May 2025 | • | 20 | 7.5 | - | - | 8.5 | 7.8 |
| Jun 2025 | • | 21 | 7.8 | - | - | 8.3 | 7.8 |
Source: UK Health Security Agency
There were no cases of hospital-onset P. aeruginosa infections in Hull recorded until early 2014 to mid-2017 and then remaining relatively constant since then at around 2-4 cases per 100,000 population. Again, it is possible that this increase is due to better testing, detection and/or recording of P. aeruginosa infections over time.
The rate in Hull has been much more variable compared to England but the infection rate has been slightly higher in Hull for more months than it has been lower.
The highest number of cases recorded in Hull has been 5.2 cases per 100,000 population (or 14 cases in total) which was relatively recently for the period January 2024 to December 2024. The rate in Hull is 4.1 per 100,000 population for the most recent period May 2024 to April 2025.
In the latest year period from May 2024 to April 2025, there has been 11 cases of hospital-onset P. aeruginosa. So the numbers are relatively small.
Compared with benchmark
P. aeruginosa bacteraemia 12-month rolling case counts and rates of hospital-onset, by Sub ICB Location (SICBL) and month (Persons All ages)
|
Period
|
Humber and North Yorkshire ICB - 03F |
NHS Humber and North Yorkshire Integrated Care Board - QOQ
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| Dec 2014 | • | - | 0.0 | - | - | 0.0 | 0.0 |
| Jan 2015 | • | - | 0.0 | - | - | 0.0 | 0.0 |
| Feb 2015 | • | - | 0.0 | - | - | 0.0 | 0.0 |
| Mar 2015 | • | - | 0.0 | - | - | 0.0 | 0.0 |
| Apr 2015 | • | - | 0.0 | - | - | 0.0 | 0.0 |
| May 2015 | • | - | 0.0 | - | - | 0.0 | 0.0 |
| Jun 2015 | • | - | 0.0 | - | - | 0.0 | 0.0 |
| Jul 2015 | • | - | 0.0 | - | - | 0.0 | 0.0 |
| Aug 2015 | • | - | 0.0 | - | - | 0.0 | 0.0 |
| Sep 2015 | • | - | 0.0 | - | - | 0.0 | 0.0 |
| Oct 2015 | • | - | 0.0 | - | - | 0.0 | 0.0 |
| Nov 2015 | • | - | 0.0 | - | - | 0.0 | 0.0 |
| Dec 2015 | • | - | 0.0 | - | - | 0.0 | 0.0 |
| Jan 2016 | • | - | 0.0 | - | - | 0.0 | 0.0 |
| Feb 2016 | • | - | 0.0 | - | - | 0.0 | 0.0 |
| Mar 2016 | • | - | 0.0 | - | - | 0.0 | 0.0 |
| Apr 2016 | • | - | 0.0 | - | - | 0.0 | 0.0 |
| May 2016 | • | - | 0.0 | - | - | 0.0 | 0.0 |
| Jun 2016 | • | - | 0.0 | - | - | 0.0 | 0.0 |
| Jul 2016 | • | - | 0.0 | - | - | 0.0 | 0.0 |
| Aug 2016 | • | - | 0.0 | - | - | 0.0 | 0.0 |
| Sep 2016 | • | - | 0.0 | - | - | 0.0 | 0.0 |
| Oct 2016 | • | - | 0.0 | - | - | 0.0 | 0.0 |
| Nov 2016 | • | - | 0.0 | - | - | 0.0 | 0.0 |
| Dec 2016 | • | - | 0.0 | - | - | 0.0 | 0.0 |
| Jan 2017 | • | - | 0.0 | - | - | 0.0 | 0.0 |
| Feb 2017 | • | - | 0.0 | - | - | 0.0 | 0.0 |
| Mar 2017 | • | - | 0.0 | - | - | 0.0 | 0.0 |
| Apr 2017 | • | - | 0.0 | - | - | 0.1 | 0.2 |
| May 2017 | • | 1 | 0.4 | - | - | 0.6 | 0.4 |
| Jun 2017 | • | 3 | 1.1 | - | - | 1.0 | 0.7 |
| Jul 2017 | • | 4 | 1.5 | - | - | 1.4 | 0.9 |
| Aug 2017 | • | 5 | 1.9 | - | - | 1.5 | 1.2 |
| Sep 2017 | • | 8 | 3.0 | - | - | 2.0 | 1.4 |
| Oct 2017 | • | 8 | 3.0 | - | - | 2.3 | 1.7 |
| Nov 2017 | • | 8 | 3.0 | - | - | 2.6 | 2.0 |
| Dec 2017 | • | 8 | 3.0 | - | - | 2.7 | 2.2 |
| Jan 2018 | • | 8 | 3.0 | - | - | 3.1 | 2.5 |
| Feb 2018 | • | 9 | 3.4 | - | - | 3.4 | 2.7 |
| Mar 2018 | • | 9 | 3.4 | - | - | 3.6 | 2.9 |
| Apr 2018 | • | 9 | 3.4 | - | - | 3.7 | 3.0 |
| May 2018 | • | 9 | 3.4 | - | - | 3.4 | 2.9 |
| Jun 2018 | • | 8 | 3.0 | - | - | 3.1 | 2.9 |
| Jul 2018 | • | 7 | 2.6 | - | - | 2.9 | 2.9 |
| Aug 2018 | • | 7 | 2.6 | - | - | 3.0 | 2.8 |
| Sep 2018 | • | 5 | 1.9 | - | - | 3.2 | 2.9 |
| Oct 2018 | • | 5 | 1.9 | - | - | 3.3 | 2.9 |
| Nov 2018 | • | 5 | 1.9 | - | - | 3.1 | 2.8 |
| Dec 2018 | • | 7 | 2.6 | - | - | 3.3 | 2.8 |
| Jan 2019 | • | 7 | 2.6 | - | - | 3.1 | 2.8 |
| Feb 2019 | • | 6 | 2.2 | - | - | 3.1 | 2.7 |
| Mar 2019 | • | 6 | 2.2 | - | - | 3.2 | 2.7 |
| Apr 2019 | • | 7 | 2.6 | - | - | 3.1 | 2.7 |
| May 2019 | • | 7 | 2.6 | - | - | 3.4 | 2.8 |
| Jun 2019 | • | 6 | 2.2 | - | - | 3.6 | 2.8 |
| Jul 2019 | • | 8 | 3.0 | - | - | 3.7 | 2.8 |
| Aug 2019 | • | 7 | 2.6 | - | - | 3.6 | 2.8 |
| Sep 2019 | • | 8 | 3.0 | - | - | 3.3 | 2.8 |
| Oct 2019 | • | 10 | 3.7 | - | - | 3.4 | 2.7 |
| Nov 2019 | • | 12 | 4.5 | - | - | 3.5 | 2.8 |
| Dec 2019 | • | 10 | 3.7 | - | - | 3.6 | 2.8 |
| Jan 2020 | • | 10 | 3.7 | - | - | 3.7 | 2.8 |
| Feb 2020 | • | 10 | 3.7 | - | - | 3.5 | 2.8 |
| Mar 2020 | • | 10 | 3.7 | - | - | 3.4 | 2.8 |
| Apr 2020 | • | 9 | 3.3 | - | - | 3.2 | 2.8 |
| May 2020 | • | 8 | 3.0 | - | - | 2.9 | 2.7 |
| Jun 2020 | • | 10 | 3.7 | - | - | 2.7 | 2.6 |
| Jul 2020 | • | 9 | 3.4 | - | - | 2.8 | 2.6 |
| Aug 2020 | • | 11 | 4.1 | - | - | 2.8 | 2.6 |
| Sep 2020 | • | 10 | 3.7 | - | - | 3.0 | 2.6 |
| Oct 2020 | • | 8 | 3.0 | - | - | 2.7 | 2.6 |
| Nov 2020 | • | 7 | 2.6 | - | - | 2.7 | 2.7 |
| Dec 2020 | • | 9 | 3.4 | - | - | 2.4 | 2.7 |
| Jan 2021 | • | 10 | 3.7 | - | - | 2.4 | 2.8 |
| Feb 2021 | • | 10 | 3.7 | - | - | 2.4 | 2.9 |
| Mar 2021 | • | 10 | 3.7 | - | - | 2.5 | 3.0 |
| Apr 2021 | • | 11 | 4.1 | - | - | 2.6 | 3.0 |
| May 2021 | • | 12 | 4.5 | - | - | 2.8 | 3.0 |
| Jun 2021 | • | 11 | 4.1 | - | - | 2.8 | 3.0 |
| Jul 2021 | • | 10 | 3.7 | - | - | 2.7 | 3.1 |
| Aug 2021 | • | 9 | 3.4 | - | - | 2.8 | 3.1 |
| Sep 2021 | • | 8 | 3.0 | - | - | 2.7 | 3.2 |
| Oct 2021 | • | 11 | 4.1 | - | - | 3.0 | 3.2 |
| Nov 2021 | • | 10 | 3.7 | - | - | 3.1 | 3.2 |
| Dec 2021 | • | 8 | 3.0 | - | - | 3.1 | 3.2 |
| Jan 2022 | • | 7 | 2.6 | - | - | 3.1 | 3.0 |
| Feb 2022 | • | 7 | 2.6 | - | - | 3.1 | 2.9 |
| Mar 2022 | • | 7 | 2.6 | - | - | 3.3 | 2.9 |
| Apr 2022 | • | 6 | 2.2 | - | - | 3.4 | 2.9 |
| May 2022 | • | 8 | 3.0 | - | - | 3.6 | 3.0 |
| Jun 2022 | • | 7 | 2.6 | - | - | 3.6 | 3.0 |
| Jul 2022 | • | 7 | 2.6 | - | - | 3.6 | 2.9 |
| Aug 2022 | • | 7 | 2.6 | - | - | 3.4 | 2.9 |
| Sep 2022 | • | 7 | 2.6 | - | - | 3.3 | 2.9 |
| Oct 2022 | • | 5 | 1.9 | - | - | 3.1 | 2.9 |
| Nov 2022 | • | 6 | 2.2 | - | - | 3.2 | 2.9 |
| Dec 2022 | • | 7 | 2.6 | - | - | 3.4 | 2.9 |
| Jan 2023 | • | 7 | 2.6 | - | - | 3.3 | 2.9 |
| Feb 2023 | • | 8 | 3.0 | - | - | 3.3 | 3.0 |
| Mar 2023 | • | 8 | 3.0 | - | - | 3.0 | 3.0 |
| Apr 2023 | • | 9 | 3.3 | - | - | 3.0 | 3.0 |
| May 2023 | • | 6 | 2.2 | - | - | 2.6 | 3.0 |
| Jun 2023 | • | 7 | 2.6 | - | - | 2.7 | 3.0 |
| Jul 2023 | • | 10 | 3.7 | - | - | 2.9 | 3.1 |
| Aug 2023 | • | 9 | 3.4 | - | - | 3.0 | 3.1 |
| Sep 2023 | • | 11 | 4.1 | - | - | 3.2 | 3.0 |
| Oct 2023 | • | 10 | 3.7 | - | - | 3.1 | 3.0 |
| Nov 2023 | • | 9 | 3.4 | - | - | 2.7 | 3.0 |
| Dec 2023 | • | 9 | 3.4 | - | - | 2.7 | 3.0 |
| Jan 2024 | • | 11 | 4.1 | - | - | 2.9 | 3.0 |
| Feb 2024 | • | 11 | 4.1 | - | - | 2.9 | 3.0 |
| Mar 2024 | • | 12 | 4.5 | - | - | 3.1 | 3.0 |
| Apr 2024 | • | 11 | 4.1 | - | - | 3.0 | 3.0 |
| May 2024 | • | 11 | 4.1 | - | - | 3.0 | 3.0 |
| Jun 2024 | • | 10 | 3.7 | - | - | 3.0 | 3.1 |
| Jul 2024 | • | 8 | 3.0 | - | - | 3.0 | 3.0 |
| Aug 2024 | • | 9 | 3.3 | - | - | 3.1 | 3.0 |
| Sep 2024 | • | 8 | 3.0 | - | - | 2.9 | 3.0 |
| Oct 2024 | • | 9 | 3.3 | - | - | 3.1 | 3.1 |
| Nov 2024 | • | 9 | 3.3 | - | - | 3.0 | 3.0 |
| Dec 2024 | • | 14 | 5.2 | - | - | 3.3 | 3.1 |
| Jan 2025 | • | 13 | 4.8 | - | - | 3.0 | 3.1 |
| Feb 2025 | • | 12 | 4.5 | - | - | 2.9 | 3.0 |
| Mar 2025 | • | 11 | 4.1 | - | - | 3.0 | 3.0 |
| Apr 2025 | • | 11 | 4.1 | - | - | 2.9 | 3.0 |
| May 2025 | • | 11 | 4.1 | - | - | 2.8 | 3.0 |
| Jun 2025 | • | 11 | 4.1 | - | - | 2.6 | 2.9 |
Source: UK Health Security Agency
The community-onset cases of P. aeruginosa also increased substantially from April 2017 to February 2018 possibly due to better testing, detection and/or recording of P. aeruginosa infections over time. Since February 2018, the rate in England has remained relatively constant at just under five cases per 100,000 population, whereas there has been much greater variability in the number of cases in Hull.
The highest number of cases recorded in Hull as 21 giving a rate of 7.8 cases per 100,000 population for the year July 2022 to June 2023 (next four months has the same number and rate of infections recorded).
For the latest period May 2024 to April 2025, there have been 3.7 cases per 100,000 population which is the lowest it has been in Hull since the end of 2023.
Over the year May 2024 to April 2025, there were 10 cases of P. aeruginosa in Hull that were community-onset cases. So the numbers are relatively small.
Compared with benchmark
P. aeruginosa bacteraemia 12-month rolling case counts and rates of community-onset, by Sub ICB Location (SICBL) and month (Persons All ages)
|
Period
|
Humber and North Yorkshire ICB - 03F |
NHS Humber and North Yorkshire Integrated Care Board - QOQ
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| Apr 2017 | • | 2 | 0.8 | - | - | 0.6 | 0.4 |
| May 2017 | • | 3 | 1.1 | - | - | 0.9 | 0.7 |
| Jun 2017 | • | 4 | 1.5 | - | - | 1.0 | 1.2 |
| Jul 2017 | • | 5 | 1.9 | - | - | 1.4 | 1.6 |
| Aug 2017 | • | 6 | 2.3 | - | - | 1.7 | 2.1 |
| Sep 2017 | • | 7 | 2.6 | - | - | 2.5 | 2.5 |
| Oct 2017 | • | 10 | 3.7 | - | - | 3.4 | 3.0 |
| Nov 2017 | • | 11 | 4.1 | - | - | 3.8 | 3.4 |
| Dec 2017 | • | 12 | 4.5 | - | - | 4.0 | 3.8 |
| Jan 2018 | • | 12 | 4.5 | - | - | 4.3 | 4.2 |
| Feb 2018 | • | 13 | 4.9 | - | - | 4.8 | 4.5 |
| Mar 2018 | • | 14 | 5.2 | - | - | 5.1 | 4.8 |
| Apr 2018 | • | 13 | 4.9 | - | - | 4.9 | 4.8 |
| May 2018 | • | 12 | 4.5 | - | - | 4.9 | 4.8 |
| Jun 2018 | • | 11 | 4.1 | - | - | 5.2 | 4.8 |
| Jul 2018 | • | 11 | 4.1 | - | - | 5.1 | 4.8 |
| Aug 2018 | • | 13 | 4.9 | - | - | 5.3 | 4.7 |
| Sep 2018 | • | 13 | 4.9 | - | - | 5.0 | 4.8 |
| Oct 2018 | • | 12 | 4.5 | - | - | 4.7 | 4.7 |
| Nov 2018 | • | 13 | 4.8 | - | - | 4.9 | 4.7 |
| Dec 2018 | • | 14 | 5.2 | - | - | 5.1 | 4.7 |
| Jan 2019 | • | 17 | 6.3 | - | - | 5.6 | 4.7 |
| Feb 2019 | • | 16 | 6.0 | - | - | 5.3 | 4.7 |
| Mar 2019 | • | 16 | 6.0 | - | - | 5.3 | 4.8 |
| Apr 2019 | • | 16 | 6.0 | - | - | 5.2 | 4.8 |
| May 2019 | • | 17 | 6.3 | - | - | 5.3 | 4.8 |
| Jun 2019 | • | 19 | 7.1 | - | - | 5.9 | 4.9 |
| Jul 2019 | • | 19 | 7.1 | - | - | 6.7 | 4.9 |
| Aug 2019 | • | 17 | 6.3 | - | - | 7.0 | 4.9 |
| Sep 2019 | • | 18 | 6.7 | - | - | 6.9 | 4.9 |
| Oct 2019 | • | 18 | 6.7 | - | - | 6.8 | 4.9 |
| Nov 2019 | • | 16 | 6.0 | - | - | 6.6 | 4.9 |
| Dec 2019 | • | 16 | 6.0 | - | - | 6.4 | 4.9 |
| Jan 2020 | • | 15 | 5.6 | - | - | 6.1 | 4.9 |
| Feb 2020 | • | 16 | 5.9 | - | - | 6.2 | 5.0 |
| Mar 2020 | • | 16 | 5.9 | - | - | 6.4 | 4.9 |
| Apr 2020 | • | 15 | 5.6 | - | - | 6.4 | 4.9 |
| May 2020 | • | 16 | 6.0 | - | - | 6.4 | 4.8 |
| Jun 2020 | • | 14 | 5.2 | - | - | 5.7 | 4.8 |
| Jul 2020 | • | 13 | 4.8 | - | - | 5.1 | 4.8 |
| Aug 2020 | • | 14 | 5.2 | - | - | 4.7 | 4.7 |
| Sep 2020 | • | 14 | 5.2 | - | - | 4.8 | 4.8 |
| Oct 2020 | • | 13 | 4.8 | - | - | 4.5 | 4.8 |
| Nov 2020 | • | 13 | 4.9 | - | - | 4.7 | 4.8 |
| Dec 2020 | • | 11 | 4.1 | - | - | 4.7 | 4.7 |
| Jan 2021 | • | 9 | 3.4 | - | - | 4.6 | 4.7 |
| Feb 2021 | • | 10 | 3.7 | - | - | 4.8 | 4.6 |
| Mar 2021 | • | 10 | 3.7 | - | - | 4.8 | 4.7 |
| Apr 2021 | • | 11 | 4.1 | - | - | 5.0 | 4.7 |
| May 2021 | • | 10 | 3.7 | - | - | 5.1 | 4.7 |
| Jun 2021 | • | 11 | 4.1 | - | - | 5.2 | 4.8 |
| Jul 2021 | • | 12 | 4.5 | - | - | 5.3 | 4.8 |
| Aug 2021 | • | 11 | 4.1 | - | - | 5.4 | 4.8 |
| Sep 2021 | • | 10 | 3.7 | - | - | 5.3 | 4.7 |
| Oct 2021 | • | 11 | 4.1 | - | - | 6.1 | 4.8 |
| Nov 2021 | • | 11 | 4.1 | - | - | 5.8 | 4.8 |
| Dec 2021 | • | 13 | 4.9 | - | - | 5.9 | 4.7 |
| Jan 2022 | • | 13 | 4.9 | - | - | 6.1 | 4.8 |
| Feb 2022 | • | 12 | 4.5 | - | - | 6.2 | 4.8 |
| Mar 2022 | • | 11 | 4.1 | - | - | 6.0 | 4.8 |
| Apr 2022 | • | 10 | 3.7 | - | - | 5.8 | 4.7 |
| May 2022 | • | 10 | 3.7 | - | - | 5.7 | 4.7 |
| Jun 2022 | • | 10 | 3.7 | - | - | 5.7 | 4.7 |
| Jul 2022 | • | 10 | 3.7 | - | - | 5.6 | 4.7 |
| Aug 2022 | • | 10 | 3.7 | - | - | 5.6 | 4.7 |
| Sep 2022 | • | 9 | 3.4 | - | - | 5.4 | 4.6 |
| Oct 2022 | • | 10 | 3.7 | - | - | 5.1 | 4.6 |
| Nov 2022 | • | 12 | 4.5 | - | - | 5.2 | 4.7 |
| Dec 2022 | • | 15 | 5.6 | - | - | 5.7 | 4.7 |
| Jan 2023 | • | 17 | 6.3 | - | - | 5.9 | 4.7 |
| Feb 2023 | • | 17 | 6.3 | - | - | 5.7 | 4.7 |
| Mar 2023 | • | 17 | 6.3 | - | - | 5.6 | 4.7 |
| Apr 2023 | • | 18 | 6.7 | - | - | 5.6 | 4.8 |
| May 2023 | • | 20 | 7.4 | - | - | 5.9 | 4.8 |
| Jun 2023 | • | 21 | 7.8 | - | - | 5.9 | 4.8 |
| Jul 2023 | • | 21 | 7.8 | - | - | 5.8 | 4.8 |
| Aug 2023 | • | 21 | 7.8 | - | - | 5.7 | 4.7 |
| Sep 2023 | • | 21 | 7.8 | - | - | 5.7 | 4.8 |
| Oct 2023 | • | 19 | 7.1 | - | - | 5.8 | 4.8 |
| Nov 2023 | • | 18 | 6.7 | - | - | 5.8 | 4.8 |
| Dec 2023 | • | 14 | 5.2 | - | - | 5.1 | 4.7 |
| Jan 2024 | • | 13 | 4.8 | - | - | 5.0 | 4.8 |
| Feb 2024 | • | 12 | 4.5 | - | - | 5.1 | 4.8 |
| Mar 2024 | • | 15 | 5.6 | - | - | 5.4 | 4.8 |
| Apr 2024 | • | 17 | 6.3 | - | - | 5.7 | 4.8 |
| May 2024 | • | 15 | 5.6 | - | - | 5.4 | 4.8 |
| Jun 2024 | • | 15 | 5.6 | - | - | 5.6 | 4.8 |
| Jul 2024 | • | 16 | 5.9 | - | - | 5.9 | 4.8 |
| Aug 2024 | • | 15 | 5.6 | - | - | 6.1 | 4.8 |
| Sep 2024 | • | 16 | 5.9 | - | - | 6.6 | 4.9 |
| Oct 2024 | • | 16 | 5.9 | - | - | 6.4 | 4.9 |
| Nov 2024 | • | 16 | 5.9 | - | - | 6.5 | 4.9 |
| Dec 2024 | • | 15 | 5.6 | - | - | 6.6 | 4.9 |
| Jan 2025 | • | 15 | 5.6 | - | - | 6.4 | 4.9 |
| Feb 2025 | • | 15 | 5.6 | - | - | 6.3 | 4.8 |
| Mar 2025 | • | 12 | 4.5 | - | - | 6.2 | 4.8 |
| Apr 2025 | • | 10 | 3.7 | - | - | 6.1 | 4.9 |
| May 2025 | • | 9 | 3.4 | - | - | 5.7 | 4.8 |
| Jun 2025 | • | 10 | 3.7 | - | - | 5.7 | 4.9 |
Source: UK Health Security Agency
Tuberculosis (TB)
The incidence (new cases) of tuberculosis (TB) for the three years 2021-23 is lower in Hull compared to England (6.4 versus 8.0 new cases per 100,000 population).
Compared with benchmark
| Indicator | Period | England | Yorkshire and the Humber region (statistical) | Kingston upon Hull | East Riding of Yorkshire | North East Lincolnshire | North Lincolnshire | York | Barnsley | Doncaster | Rotherham | Sheffield | Bradford | Calderdale | Kirklees | Leeds | Wakefield | North Yorkshire Cty |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
TB incidence (three year average) (Persons All ages) | 2021 - 23 | 8.0 | 6.0 | 6.4 | 2.2 | - | 4.3 | 2.5 | 3.5 | 6.2 | 4.5 | 6.5 | 14.0 | 5.1 | 8.5 | 8.1 | 3.2 | - |
| Indicator | Period | England | Yorkshire and the Humber region (statistical) | Kingston upon Hull | East Riding of Yorkshire | North East Lincolnshire | North Lincolnshire | York | Barnsley | Doncaster | Rotherham | Sheffield | Bradford | Calderdale | Kirklees | Leeds | Wakefield | North Yorkshire Cty |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
TB incidence (three year average) (Persons All ages) | 2021 - 23 | 8.0 | 6.0 | 6.4 | 2.2 | - | 4.3 | 2.5 | 3.5 | 6.2 | 4.5 | 6.5 | 14.0 | 5.1 | 8.5 | 8.1 | 3.2 | - |
The number of new cases of TB in Hull was around five per 100,000 population for the three year period 2001-03, but gradually increased to a high of 8.8 new cases per 100,000 population for 2010-12. The rate subsequently decreased to 5.9 new cases per 100,000 population for 2015-17, but increased to 7.5 new cases per 100,000 population for 2019-21. There has been a reduction to 6.4 new cases per 100,000 population for the three year period 2021-23.
The incidence rate had been statistically significantly lower in Hull compared to England prior to 2018-20, but for the last five years 2017-19 to 2021-22, the incidence rate had been comparable to England (no statistically significant difference).
Compared with benchmark
TB incidence (three year average) (Persons All ages)
|
Period
|
Kingston upon Hull |
Yorkshire and the Humber region (statistical)
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2001 - 03 | • | 38 | 5.1 | 3.6 | 6.9 | 10.7 | 13.1 |
| 2002 - 04 | • | 43 | 5.7 | 4.2 | 7.6 | 10.5 | 13.5 |
| 2003 - 05 | • | 36 | 4.7 | 3.4 | 6.5 | 10.8 | 14.1 |
| 2004 - 06 | • | 38 | 5.0 | 3.6 | 6.8 | 11.5 | 14.8 |
| 2005 - 07 | • | 40 | 5.2 | 3.8 | 7.0 | 12.0 | 15.1 |
| 2006 - 08 | • | 45 | 5.9 | 4.3 | 7.8 | 12.4 | 15.0 |
| 2007 - 09 | • | 37 | 4.8 | 3.4 | 6.6 | 12.5 | 15.1 |
| 2008 - 10 | • | 40 | 5.2 | 3.8 | 7.0 | 12.5 | 15.1 |
| 2009 - 11 | • | 52 | 6.8 | 5.1 | 8.8 | 12.6 | 15.2 |
| 2010 - 12 | • | 68 | 8.8 | 6.9 | 11.1 | 11.9 | 15.1 |
| 2011 - 13 | • | 65 | 8.4 | 6.5 | 10.6 | 11.6 | 14.7 |
| 2012 - 14 | • | 59 | 7.6 | 5.8 | 9.7 | 10.6 | 13.5 |
| 2013 - 15 | • | 51 | 6.5 | 4.9 | 8.5 | 9.6 | 11.9 |
| 2014 - 16 | • | 48 | 6.1 | 4.5 | 8.0 | 8.5 | 10.8 |
| 2015 - 17 | • | 47 | 5.9 | 4.4 | 7.8 | 7.4 | 9.9 |
| 2016 - 18 | • | 49 | 6.1 | 4.6 | 8.0 | 6.9 | 9.2 |
| 2017 - 19 | • | 54 | 6.7 | 5.1 | 8.7 | 6.4 | 8.6 |
| 2018 - 20 | • | 59 | 7.3 | 5.6 | 9.4 | 6.1 | 8.0 |
| 2019 - 21 | • | 60 | 7.5 | 5.8 | 9.6 | 5.9 | 7.8 |
| 2020 - 22 | • | 56 | 7.0 | 5.3 | 9.0 | 5.6 | 7.6 |
| 2021 - 23 | • | 52 | 6.4 | 4.9 | 8.4 | 6.0 | 8.0 |
Source: UK Health Security Agency and Office for National Statistics
Seven in ten of drug sensitive TB notification cases had the full treatment course in 2022 in Hull compared to 83% for England. The rate in Hull was the lowest across the region, although data was not available for all local authorities.
The numbers of drug sensitive TB notifications are small which means that there is considerable year-on-year variability (see Small Numbers in the Glossary for more information.).
Compared with benchmark
| Indicator | Period | England | Yorkshire and the Humber region (statistical) | Kingston upon Hull | East Riding of Yorkshire | North East Lincolnshire | North Lincolnshire | York | Barnsley | Doncaster | Rotherham | Sheffield | Bradford | Calderdale | Kirklees | Leeds | Wakefield | North Yorkshire Cty |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Proportion of drug sensitive TB notifications who had completed a full course of treatment by 12 months (Persons All ages) | 2022 | 82.8 | 83.2 | 69.2 | - | - | - | - | 88.9 | 75.0 | 83.3 | 78.6 | 85.5 | 90.0 | 90.0 | 82.7 | 100 | - |
| Indicator | Period | England | Yorkshire and the Humber region (statistical) | Kingston upon Hull | East Riding of Yorkshire | North East Lincolnshire | North Lincolnshire | York | Barnsley | Doncaster | Rotherham | Sheffield | Bradford | Calderdale | Kirklees | Leeds | Wakefield | North Yorkshire Cty |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Proportion of drug sensitive TB notifications who had completed a full course of treatment by 12 months (Persons All ages) | 2022 | 82.8 | 83.2 | 69.2 | - | - | - | - | 88.9 | 75.0 | 83.3 | 78.6 | 85.5 | 90.0 | 90.0 | 82.7 | 100 | - |
During 2021, six of the 17 people with drug sensitive TB had completed their full treatment within 12 months in Hull. However, with the relatively small number of drug sensitive TB notifications, there is considerable variability in the percentages completing full treatment. In general, the treatment completion rates have been comparable to England with no statistically significant differences, but there have been four years in the last 21 years where the percentages have been statistically significantly lower in Hull compared to England including the last two years of 2020 and 2021.
The percentage of people with drug sensitive TB had completed their full treatment within 12 months has ranged from 35% to 100% in Hull over the 22 year period. Across England, the percentage gradually increased from 65% in 2001 to 87% for 2013, before decreasing to 83% for 2022.
In the last ten years or so, the rate in Hull was comparable or slightly higher than England with the exception of 2015 when the rate was much lower in Hull (54% versus 85%) and the most recent 2-3 years. The numbers are very small in Hull though. In the last three years, the percentage in Hull has been statistically significantly lower than England for two of those three years despite the small numbers. In 2020, 11 out of 19 complete their full course of treatment and this was 6 out of 17 for 2021 and 9 out of 13 for 2022 equating to a total of 23 out of 49 (47%) who did not complete the full course of treatment.
Compared with benchmark
Proportion of drug sensitive TB notifications who had completed a full course of treatment by 12 months (Persons All ages)
|
Period
|
Kingston upon Hull |
Yorkshire and the Humber region (statistical)
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2001 | • | 5 | 71.4% | 30.3% | 94.9% | 78.6% | 64.9% |
| 2002 | • | 10 | 71.4% | 42.0% | 90.4% | 78.5% | 69.5% |
| 2003 | • | 12 | 80.0% | 51.4% | 94.7% | 80.9% | 72.4% |
| 2004 | • | 10 | 76.9% | 46.0% | 93.8% | 65.0% | 73.6% |
| 2006 | • | 11 | 73.3% | 44.8% | 91.1% | 77.4% | 79.7% |
| 2007 | • | 10 | 71.4% | 42.0% | 90.4% | 76.5% | 82.6% |
| 2008 | • | 9 | 75.0% | 42.8% | 93.3% | 80.2% | 84.7% |
| 2009 | • | 4 | 57.1% | 20.2% | 88.2% | 81.2% | 85.7% |
| 2010 | • | 11 | 64.7% | 38.6% | 84.7% | 81.5% | 86.6% |
| 2011 | • | 17 | 73.9% | 51.3% | 88.9% | 78.0% | 86.6% |
| 2012 | • | 22 | 100% | 81.5% | 100% | 87.4% | 87.8% |
| 2013 | • | 13 | 100% | 71.7% | 100% | 88.9% | 87.1% |
| 2014 | • | 14 | 87.5% | 60.4% | 97.8% | 89.2% | 86.4% |
| 2015 | • | 7 | 53.8% | 26.1% | 79.6% | 85.9% | 84.7% |
| 2016 | • | 10 | 76.9% | 46.0% | 93.8% | 88.5% | 85.5% |
| 2017 | • | 12 | 85.7% | 56.2% | 97.5% | 91.8% | 85.8% |
| 2018 | • | 17 | 89.5% | 65.5% | 98.2% | 90.1% | 85.2% |
| 2019 | • | 14 | 82.4% | 55.8% | 95.3% | 86.8% | 85.3% |
| 2020 | • | 11 | 57.9% | 34.0% | 78.9% | 80.3% | 85.0% |
| 2021 | • | 6 | 35.3% | 15.3% | 61.4% | 81.0% | 85.1% |
| 2022 | • | 9 | 69.2% | 38.9% | 89.6% | 83.2% | 82.8% |
Source: UK Health Security Agency
Childhood Diseases
There is relatively limited information on the incidence of childhood diseases such as measles, mumps, rubella, etc, although some information relating to vaccinations of some conditions can be found within Vaccinations under Prevention for Adults, and within Screening and Vaccinations under Health Factors for Children and Young People.
COVID-19
Further information on Coronavirus (COVID-19) can be found under Health Factors within Adults.
Influenza
Further information on some other influenza can be found within Respiratory Diseases under Health Factors within Adults. Information relating to flu vaccinations can be found within Vaccinations under Prevention for Adults, and within Screening and Vaccinations under Health Factors for Children and Young People.
Sexually Transmitted Infections
Further information on Sexually Transmitted Infectious can be found under Health Factors within Adults.
Mortality from Communicable Diseases
For deaths registered during 2021-23, the direct standardised mortality rates for communicable diseases was slightly higher in Hull at 14.2 deaths per 100,000 population compared to 13.0 deaths per 100,000 population for England.
The measure includes deaths from certain infectious and parasitic diseases based on the International Classification of Diseases version 10 codes A00 to B99 as well as influenza (ICD10 codes J09-J11).
Compared with benchmark
| Indicator | Period | England | Yorkshire and the Humber region (statistical) | Kingston upon Hull | East Riding of Yorkshire | North East Lincolnshire | North Lincolnshire | York | North Yorkshire UA | Barnsley | Doncaster | Rotherham | Sheffield | Bradford | Calderdale | Kirklees | Leeds | Wakefield |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Mortality rate from a range of specified communicable diseases, including influenza (Persons All ages) | 2021 - 23 | 13.0 | 13.4 | 14.2 | 10.7 | 7.4 | 13.0 | 11.2 | 10.9 | 17.2 | 11.5 | 14.2 | 14.9 | 11.8 | 14.5 | 14.3 | 16.1 | 17.6 |
| Indicator | Period | England | Yorkshire and the Humber region (statistical) | Kingston upon Hull | East Riding of Yorkshire | North East Lincolnshire | North Lincolnshire | York | North Yorkshire UA | Barnsley | Doncaster | Rotherham | Sheffield | Bradford | Calderdale | Kirklees | Leeds | Wakefield |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Mortality rate from a range of specified communicable diseases, including influenza (Persons All ages) | 2021 - 23 | 13.0 | 13.4 | 14.2 | 10.7 | 7.4 | 13.0 | 11.2 | 10.9 | 17.2 | 11.5 | 14.2 | 14.9 | 11.8 | 14.5 | 14.3 | 16.1 | 17.6 |
There were 92 deaths to Hull residents from communicable diseases that were registered within the three-year period 2021 to 2023. Between 2012-14 and 2020-22, there have been around 10-11 deaths per 100,000 population (slightly lower during the pandemic), so that latest rate represents an increase on trends observed over the last decade or so.
Compared with benchmark
Mortality rate from a range of specified communicable diseases, including influenza (Persons All ages)
|
Period
|
Kingston upon Hull |
Yorkshire and the Humber region (statistical)
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2001 - 03 | • | 70 | 12.4 | 9.7 | 15.7 | 8.5 | 9.2 |
| 2002 - 04 | • | 71 | 13.1 | 10.2 | 16.5 | 8.8 | 9.6 |
| 2003 - 05 | • | 86 | 16.0 | 12.8 | 19.8 | 9.5 | 10.9 |
| 2004 - 06 | • | 90 | 16.5 | 13.3 | 20.4 | 10.0 | 12.9 |
| 2005 - 07 | • | 106 | 18.5 | 15.1 | 22.4 | 11.2 | 14.9 |
| 2006 - 08 | • | 93 | 16.1 | 12.9 | 19.8 | 12.1 | 14.9 |
| 2007 - 09 | • | 76 | 12.9 | 10.1 | 16.1 | 11.9 | 13.3 |
| 2008 - 10 | • | 55 | 9.2 | 6.9 | 12.0 | 10.3 | 10.9 |
| 2009 - 11 | • | 82 | 13.7 | 10.9 | 17.1 | 9.5 | 9.9 |
| 2010 - 12 | • | 89 | 14.8 | 11.8 | 18.2 | 9.2 | 9.1 |
| 2011 - 13 | • | 91 | 15.0 | 12.0 | 18.5 | 9.2 | 8.9 |
| 2012 - 14 | • | 65 | 10.7 | 8.2 | 13.7 | 8.2 | 8.5 |
| 2013 - 15 | • | 63 | 10.7 | 8.2 | 13.7 | 8.3 | 8.8 |
| 2014 - 16 | • | 67 | 11.5 | 8.9 | 14.6 | 8.5 | 9.0 |
| 2015 - 17 | • | 63 | 11.0 | 8.5 | 14.2 | 8.9 | 9.1 |
| 2016 - 18 | • | 66 | 11.0 | 8.5 | 14.0 | 9.5 | 9.6 |
| 2017 - 19 | • | 61 | 10.0 | 7.6 | 12.9 | 9.6 | 9.5 |
| 2018 - 20 | • | 59 | 9.3 | 7.0 | 12.0 | 9.4 | 9.4 |
| 2019 - 21 | • | 62 | 9.9 | 7.5 | 12.7 | 8.9 | 9.0 |
| 2020 - 22 | • | 73 | 11.5 | 9.0 | 14.4 | 10.4 | 10.3 |
| 2021 - 23 | • | 92 | 14.2 | 11.4 | 17.5 | 13.4 | 13.0 |
Source: Office for Health Improvement and Disparities
From local data, the deaths from communicable diseases were mainly from bacteria diseases including those which resulted in sepsis with 38 deaths in total. Additionally, there were 14 deaths from intestinal infectious diseases, seven deaths from flu, and five deaths from viral hepatitis. The remaining nine deaths were from tuberculosis, viral infections, HIV, mycoses, sequelae (or consequence) of infectious and parasitic diseases, and other infectious diseases. There were a similar number of deaths for men (35) and women (38). Almost seven in ten of the deaths were among those aged 70+ years with 7, 10, 14 and 19 deaths among those aged 70-74, 75-79, 80-84 and 85+ years respectively. There were nine deaths among people aged 40-49 years, four deaths among those aged 50-59 years and six deaths among those aged 60-69 years.
There were 92 deaths from communicable diseases which were registered during the period 2021-23, with a similar number of deaths from the different causes mentioned above except a higher number from bacteria diseases including those which resulted in sepsis (50) and from flu (15). There was also a similar number of deaths for males (47) and females (45), and just over two-thirds were among people aged 70+ years with 13, 12, 15 and 22 deaths among those aged 70-74, 75-79, 80-84 and 85+ years respectively. There were seven deaths among people aged 40-49 years, six deaths among those aged 50-59 years and 13 deaths among those aged 60-69 years.
The number of deaths registered each year from communicable disease has generally been around 22-27, but has been particularly high for some years such as 2007 when there was 45, 2011 when there was 57 and 2016 when there was 32. The higher numbers are generally due to a higher number of deaths from sepsis. There was only 16 deaths from communicable disease that were registered during 2020 which is associated with the COVID-19 pandemic as there was lower rates of social mixing, people wearing face masks and likely more people employing better hand hygiene habits. However, the number of deaths from communicable disease registered during 2022 and 2023 are relatively high with 33 and 35 deaths respectively.
There have been relatively few deaths from influenza with five registered during 2018, six during 2019 and very few registered during 2020 and 2021 due to the pandemic. The numbers increased to five and 10 for 2022 and 2023 respectively with seven already registered in 2024 (which includes most deaths which have been registered up to the end of July 2024).
Antibiotic Prescribing in Primary Care
Reductions in antibiotic consumption is a well-recognised target in antimicrobial resistance (AMR) policies both nationally and internationally. Fingertips includes information on adjusted antibiotic prescribing in primary are by the NHS. The rates of antibiotic prescribing are adjusted to take into account the demographics of the population as this influences the levels of prescribing. The annual total number of prescribing antibiotic items per STAR PU (Specific Therapeutic group Age sex weightings Related Prescribing Units) are given. The information is presented as indirectly standardised ratios (see Indirectly Standardised Ratios within the Glossary for more information although for the case of antibiotic prescribing the comparison groups is not England as the ratio is not one for England but the ‘standard’ is related to the population in terms of the STAR PU).
For 2023, after adjusting for the population, there is a marginally higher rate of antibiotic prescribing in Hull compared to England (0.90 versus 0.88 annual total items per STAR PU).
Compared with benchmark
| Indicator | Period | England | Yorkshire and the Humber region (statistical) | Kingston upon Hull | East Riding of Yorkshire | North East Lincolnshire | North Lincolnshire | York | Barnsley | Doncaster | Rotherham | Sheffield | Bradford | Calderdale | Kirklees | Leeds | Wakefield | North Yorkshire Cty |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Adjusted antibiotic prescribing in primary care by the NHS (Persons All ages) | 2023 | 0.88 | 0.94 | 0.90 | 0.92 | 1.01 | 0.94 | 0.78 | 0.98 | 0.95 | 1.00 | 0.83 | 0.98 | 0.99 | 1.05 | 0.88 | 1.05 | - |
| Indicator | Period | England | Yorkshire and the Humber region (statistical) | Kingston upon Hull | East Riding of Yorkshire | North East Lincolnshire | North Lincolnshire | York | Barnsley | Doncaster | Rotherham | Sheffield | Bradford | Calderdale | Kirklees | Leeds | Wakefield | North Yorkshire Cty |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Adjusted antibiotic prescribing in primary care by the NHS (Persons All ages) | 2023 | 0.88 | 0.94 | 0.90 | 0.92 | 1.01 | 0.94 | 0.78 | 0.98 | 0.95 | 1.00 | 0.83 | 0.98 | 0.99 | 1.05 | 0.88 | 1.05 | - |
The annual total number of antibiotic items prescribed in primary care by the NHS has reduced in Hull from 1.22 to 0.93 units per STAR PU between 2015 and 2022. A reasonably similar rate of change has occurred for England. There was a decrease in 2020 and 2021, likely associated with the COVID-19 pandemic, but rates have increased in 2022, although are at a lower level than the rates observed prior to the pandemic.
In 2015, the rate of antibiotic prescribing in primary are by the NHS after taking into account Hull’s population was 11% higher than England (1.22 versus 1.10 annual total items per STAR PU). This has reduced over time to 2% higher in Hull compared to England for 2023 (0.90 versus 0.88 annual total items per STAR PU).
Compared with benchmark
Adjusted antibiotic prescribing in primary care by the NHS (Persons All ages)
|
Period
|
Kingston upon Hull |
Yorkshire and the Humber region (statistical)
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2015 | • | 193737 | 1.22 | 1.21 | 1.23 | 1.15 | 1.10 |
| 2016 | • | 188910 | 1.18 | 1.17 | 1.18 | 1.12 | 1.08 |
| 2017 | • | 187134 | 1.16 | 1.16 | 1.17 | 1.09 | 1.04 |
| 2018 | • | 176767 | 1.09 | 1.08 | 1.09 | 1.03 | 0.99 |
| 2019 | • | 169722 | 1.04 | 1.03 | 1.04 | 1.00 | 0.95 |
| 2020 | • | 135982 | 0.83 | 0.82 | 0.83 | 0.81 | 0.75 |
| 2021 | • | 137250 | 0.83 | 0.83 | 0.84 | 0.81 | 0.74 |
| 2022 | • | 155162 | 0.93 | 0.93 | 0.94 | 0.93 | 0.87 |
| 2023 | • | 152411 | 0.90 | 0.90 | 0.91 | 0.94 | 0.88 |
Source: NHS England
Vaccinations For Infectious Diseases
Information relating to vaccinations of some infectious conditions can be found within Vaccinations under Prevention for Adults, and within Screening and Vaccinations under Health Factors for Children and Young People.
Strategic Need and Service Provision
Whilst effects from some infectious diseases can be relatively mild, some infectious diseases can cause high levels of mortality and disability. Therefore, it is important to prevent the spread of infectious diseases as much as possible, particularly those infections that have a higher likelihood of causing death and disability.
From the UK Health Security Agency, the general advice for managing outbreaks of infectious diseases in a particular setting or establishment is to encourage people who are unwell to not attend or remain separate from others, ensuring all eligible groups are enabled and supported to take up the offer of vaccinations, ensuring occupied spaces are well ventilated, reinforcing good hygiene practice, and requesting that infectious diseases are reported to the setting or establishment. There are recommendations on how long people should remain away from a setting such as work, school or nursery for specific diseases, and certain infections need to be reported to the Health Protection Teams. The UK Health Security Agency also has advice for Managing Specific Infectious Diseases.
Resources
Very Well Health. https://www.verywellhealth.com/the-difference-between-communicable-and-infectious-diseases-4151985
World Health Organisation. Infectious Diseases. https://www.emro.who.int/health-topics/infectious-diseases/index.html
UK Health Security Agency. Guidance: Managing outbreak and incidents. https://www.gov.uk/government/publications/health-protection-in-schools-and-other-childcare-facilities/managing-outbreaks-and-incidents
UK Government. Escherichia coli (E. coli): guidance, data and analysis. https://www.gov.uk/government/collections/escherichia-coli-e-coli-guidance-data-and-analysis
UK Government. Staphylococcus aureus (MRSA): guidance, data and analysis. https://www.gov.uk/government/collections/staphylococcus-aureus-guidance-data-and-analysis
UK Government. Clostridioides difficile (C. difficile): guidance, data and analysis. https://www.gov.uk/government/collections/clostridium-difficile-guidance-data-and-analysis
UK Government. Klebsiella species: guidance, data and analysis. https://www.gov.uk/government/collections/klebsiella-species-guidance-data-and-analysis
UK Government. Pseudomonas aeruginosa (P. aeruginosa): guidance, data and analysis. https://www.gov.uk/government/collections/pseudomonas-aeruginosa-guidance-data-and-analysis
World Health Organisation. Tuberculosis. https://www.who.int/health-topics/tuberculosis
NHS. Tuberculosis (TB). https://www.nhs.uk/conditions/tuberculosis-tb/
The Office for Health Improvement & Disparities’ Fingertips: https://fingertips.phe.org.uk/
Updates
This page was last updated / checked on 3 July 2025.
This page is due to be updated / checked in January 2026.
Migrants
This topic area covers statistics and information relating to migrants in Hull and the Yorkshire and Humber region including refugees and asylum seekers. Further information relating to Race and Ethnicity is given under Population.
Headlines
- There is no single definition of migrants and often different information is recorded which makes it difficult to quantify the number of migrants and examine their health needs.
- The dictionary definition of a migrant is a person who moves from one place to another, especially in order to find work or better living conditions, and a refugee is a person who has been forced to leave their country in order to escape war, persecution, or national disaster. An asylum-seeker is someone who is seeking international protection who has left their home country as a political refugee and is seeking asylum in another country. Only asylum-seekers who are granted refugee status are allowed to work in the country.
- In terms of defining migrants within health and other datasets, migrants are often defined as foreign-born, by foreign nationality or duration of stay, but none of these truly fulfil the definition a ‘migrant’, but are simply a consequence of the information captured within specific datasets.
- At the time of the 2021 Census, 34,963 of Hull’s residents were foreign-born representing 13.1% of all Hull residents mainly born in Ireland or Europe (8.5%) with smaller percentages from the Middle East and Asia (2.8%) and Africa (1.5%). However, there were large differences by age with 3.4% of Hull residents aged 65+ years being foreign-born compared to 23.0% among those aged 35-49 years.
- Over four in ten (43%) of Hull residents who had not been born in the UK, had moved to the UK prior to 2011 (15,058 residents in total). The remaining 19,906 residents had moved to the UK in the last decade between 2011 and 2021.
- Of Hull residents who were foreign-born, 44% had been in the UK for more than 10 years, 25% for five years or more but less than ten years, 17% for two years or more but less than five years, and 14% had been in the UK for less than two years. Half of people who were aged 0-15 years when they first arrived in the UK had been in the UK for 10 or more years, but the percentage was lower with older age groups decreasing to 21% among those who had first arrived in the UK when they were 65+ years. Overall, among
- Almost nine in ten of Hull’s residents has been at the same address one year prior to the Census (88.5%), 0.7% had been at a student term-time address one year ago, 8.9% had been at a different UK address one year ago, and 0.7% had been at a non-UK address one year ago. Perhaps not surprisingly, the oldest (50+ years) and youngest (<15 years) residents were the most likely to be living at the same address as they were one year ago, whereas those aged 16-24 years were the least likely to be living at the same address as one year ago. Hull residents who were born outside the UK were less likely to have been at the same address one year prior to the Census, although for three-quarters this was because they were at a different address in the UK a year ago rather than being at an address outside the UK a year ago.
- Migrants populations are extremely diverse, and their health needs differ greatly. On average, foreign-born residents of the UK have better health compared to UK-born residents even accounting for age. However, this masks considerable differences among migrants. People who migrate solely for social and economic reasons have much better health than people who are forced to flee from poverty, adverse events, persecution, oppression and violence. Refugees and asylum seekers have much worse health. Migrants face an increased likelihood of adverse health outcomes resulting from previous conflict and trauma as well as other adverse events from their countries and their journey. Furthermore, they face additional exclusions and barriers to essential services such as housing, employment, education, social services and healthcare in their destination country due to exclusionary migration policies, and language and cultural barriers as well as racism and discrimination.
The Population Affected – Why Is It Important?
In the BioMed Central article on migration and health research, they state that human migration is essential to growing economies and represent a critical part of social and cultural fabric of our societies. They point out that global migration continues to rise at unprecedented rates, fuelled by ‘push’ factors such as extreme weather events caused by climate change, conflict and violence, political instability, and poverty, as well as ‘pull’ factors including kinship networks and a desire for social and economic mobility.
Definitions
The dictionary definition of a migrant is a person who moves from one place to another, especially in order to find work or better living conditions, and a refugee is a person who has been forced to leave their country in order to escape war, persecution, or national disaster. An asylum-seeker is someone who is seeking international protection who has left their home country as a political refugee and is seeking asylum in another country. Only asylum-seekers who are granted refugee status are allowed to work in the country. The term ‘illegal immigrant’ or ‘irregular migration’ is often used and this often refers to someone who is living and/or working in the UK without the legal right to do so (and as a result are generally not permitted to work or access benefits, social housing or free hospital care).
As stated by the Migration Observatory, there are different definitions of migrants. Migrants might be defined as foreign-born, by foreign citizenship, or by their movement into a new country to stay temporarily or settle for the long-term. Dictionary definitions sometimes distinguish immigrants – people who are, or intend to be, settled in their new country – from migrants who temporarily residents. However, in practice, phrases are used interchangeably, and there are no definitions in law, although from a legal perspective, there is a key distinction between people who are ‘subject to immigration control’, who need permission to enter or remain in the UK, and those who do not. While the UK was part of the European Union, European Union nationals were not subject to immigration control, although they were often described as migrants. Different datasets define migrants based on country of birth, nationality and/or length of stay depending on what data is collected. The Office of National Statistics use the United Nations definition of ‘long-term international migrant’ as “a person who moves to a country other than that of his or her usual residence for a period of at least one year so that the country of destination effectively becomes his or her new country of usual residence”. This represents a challenge for newly arrived migrants as it is often not known how long they will stay. To complicate the situation further, different definitions are not interchangeable. For example, people who are foreign-born are not all foreign nationals, some foreign nationals may have lived in the UK for decades whereas others have only been in the UK for a year. Not all foreign-born UK residents are subject to immigration control as there will be some children born abroad of UK national parents (e.g. service personnel) and others are long-term British residents who have acquired citizenship. In addition, the term ‘migrant’ is sometimes distinguished from, and sometimes includes, foreign nationals who are seeking asylum in the UK. These represents a small proportion of the overall entrants into the UK, although attract a great deal of public and policy attention.
Migrant status can also be relatively fluid depending on the ‘length of time in country’ used to define migrants. Whilst one year in the country is generally used to define migrants, there will be people who living in the UK for shorter periods of time, or return periodically. Some people who are foreign-born can come to the UK to study, and some people born in the UK can move abroad to study. Some of these will be temporary moves which might last the duration of the educational course, but others may settle in the country due to the relationships formed, preference, or for work prospects. This of course is true of people who come into the UK or move out of the UK for work or other purposes, they could return to their country of birth in the future, or return to their country of birth for a period of time and then return to the UK again. The people who migrate may have a plan or idea of how long they will remain in their new country when they migrate, but the time actually spent in the country ultimately may be different to that originally anticipated, and additionally will likely depend on permissions to enter or remain in the UK. People who are aged 18-39 years are probably more likely to migrate for study or work reasons.
As stated by the Migration Observatory, the definition of ‘migrant’ is not simply a technical problem but has an important effect on migration data and the analyses generated from the data. This, in turn, has an impact on public understanding and on policy debates. The confusion in public debate over the definition of ‘migrant’ poses challenges for government policy. Not all those who are considered ‘migrants’ in public debate and datasets are subject to immigration controls and policies. The definition of ‘migrant’ used by most official sources includes many British citizens and others whose rights to work and access to services in the UK are not determined by immigration controls alone.
Regardless of migration status, all refugees and migrants have the right to health and countries should provide refugee and migrant-sensitive health care services.
Why is Refugee and Migrant Health Important?
From the World Health Organisation, global migration is a long-standing phenomenon. It may increase because of conflict, persecution, environmental degradation and climate change, and a profound lack of human security and opportunity. Many people move in the hope of improved employment and life opportunities.
The correlation between health and migration is dynamic by nature and complex. Health is strongly related to the social determinants of health, including employment, income, education and housing. When not properly supported by appropriate intersectoral policies, migration can expose the most vulnerable socioeconomic groups to significant risks.
Addressing the needs of these populations with well-functioning public health and health services responds to the human right to health, protects the health of both migrants and host communities, and contributes to integration and social and economic development. This is because refugees and migrants contribute to the society in which they live, especially when in good health. Access to information, prevention and appropriate care, including diagnostics, treatment and vaccines, is essential for these groups to fulfil their health needs. Furthermore, it ensures security for global public health.
Health Among Refugees and Migrants
Migrant populations are very diverse. People who choose to migrate for social or economic reasons can be very different compared to people who are forced to migrate. From the Migration Observatory, on average, foreign-born residents are healthier than UK-born residents. In part, this is because people who are not born in the UK tend to be younger than people born in the UK. However, even within the same age groups, people who are foreign-born have better health than people who were born in the UK. This is because the people who tend to migrate for social or economic reasons tend to be younger and healthier than those who stay behind and do not migrate, and at the same time, the Migration Observatory state that the healthiest migrants are more likely to stay in their new destination rather than return to their origin countries.
However, whilst this is the case on average, this masks considerable inequalities within the migrant population. People who are forced to flee from adverse events – persecution, oppression and violence – are by their very nature include a higher percentage of vulnerable populations. Refugees and asylum seekers have much worse health than other migrants.
Barriers to Health
From the World Health Organisation, refugees and migrants often experience barriers in accessing essential services including health because legislation or regulations restrict access according to nationality or migration status; fear of immigration authorities and detection, detention and deportation; financial barriers; language and cultural differences; social stigma; administrative hurdles; and the inability to join local health financing schemes (particularly social insurance schemes).
A significant challenge is the national acceptance in legal and policy terms of the human right to health of refugees and migrants. This acceptance requires political commitment to tackle xenophobia, discrimination, exclusion and misinformation about these populations and their health needs.
Reduction or removal of communication and language barriers is key to improving access to services by refugees and migrants. However, while a common language is crucial, culturally competent services should offer more than just minimal communication. Refugee-friendly and migrant-friendly services should be able to explain the host country’s system of health care, and use telephone interpreting, face-to-face interpreting, intercultural mediation, and supportive written information to improve health communication for both providers and patients.
Migrant Health Guide
The UK government has a Migrant Health Guide which provides advice and guidance on the health needs of migrant patients for healthcare professionals. It covers access to healthcare, assessing and treating patients, vulnerable migrant groups, communicable diseases, outbreak management, non-communicable diseases and nutrition.
The Hull Picture
Estimated Number of Migrants in Hull
The information presented below is based on information from the 2021 Census and as a result is based on the Hull residents at the time of the Census. The Census collected information on country of birth, time living in UK, age of first arrival in UK and whether the person’s address one year ago was the same as their (current) address at the time of the Census. The information from the Census can be used to give an estimate of the number of ‘migrants’ living in Hull, but due to there being no standard definition, the numbers will differ and conflict depending on what measure is used, and may not reflect the number of people in Hull who are living in Hull based on permission to enter or stay in the UK (subject to immigration control). Many people living in Hull who are foreign-born have lived in the UK a long time.
As the UK Census clearly does not include non-UK residents at the time of the Census, it cannot provide information on the number of UK-born or foreign-born people who lived in Hull one year prior to the Census but had moved outside the UK and were living abroad at the time of the Census. However, there are other national sources and estimates in relation to the numbers entering and leaving Hull available from the Office of National Statistics provided as part of their resident population estimates.
Estimates Based on the 2021 Census
From the 2021 Census, based on the foreign-born, there were 34,963 residents of Hull who were not born in the UK representing 13.1% of all Hull’s residents. However, the percentages were not evenly distributed by age with a far higher percentage of residents not born in the UK among those aged 25-34 years (20.2%) and 35-49 years (23.0%) compared to those aged under 15 years (7.2%), 50-64 years (9.4%) or 65+ years (3.4%). Overall, 65% of residents who were not born in the UK were born in European countries although this also varied by age from 54% among those aged 65+ years to 70% among those aged under 15 years.
| Country of birth | <15 | 16-24 | 25-34 | 35-49 | 50-64 | 65+ | Total |
| Total (N) | 53,139 | 31,806 | 41,038 | 50,812 | 49,396 | 40,824 | 267,015 |
| UK (N) | 49,324 | 26,662 | 32,765 | 39,105 | 44,776 | 39,420 | 232,052 |
| Foreign-born (N) | 3,815 | 5,144 | 8,273 | 11,707 | 4,620 | 1,404 | 34,963 |
| UK (%) | 92.8 | 83.8 | 79.8 | 77.0 | 90.6 | 96.6 | 86.9 |
| Foreign-born (%) | 7.2 | 16.2 | 20.2 | 23.0 | 9.4 | 3.4 | 13.1 |
| Ireland & other Europe (%) | 5.0 | 10.4 | 13.8 | 14.6 | 5.7 | 1.9 | 8.5 |
| Africa (%) | 0.7 | 2.1 | 1.9 | 2.6 | 1.2 | 0.4 | 1.5 |
| Middle East & Asia (%) | 1.3 | 3.3 | 4.0 | 5.3 | 2.1 | 0.9 | 2.8 |
| Americans & Caribbean (%) | 0.1 | 0.4 | 0.3 | 0.4 | 0.3 | 0.2 | 0.3 |
| Antarctica & Oceania including Australasia (%) | 0.0 | 0.1 | 0.1 | 0.2 | 0.1 | 0.0 | 0.1 |
From the 2021 Census, based on the year of arrival in the UK, 232,051 Hull residents were born in the UK representing 86.9% of the population. Over four in ten (43%) of Hull residents who had not been born in the UK, had moved to the UK prior to 2011 (15,058 residents in total). The remaining 19,906 residents had moved to the UK in the last decade between 2011 and 2021.
| Year of arrival in UK | Number | Percentage |
| Born in UK | 232,051 | 86.9 |
| Before 1951 | 103 | 0.0 |
| 1951 to 1960 | 235 | 0.1 |
| 1961 to 1970 | 490 | 0.2 |
| 1971 to 1980 | 679 | 0.3 |
| 1981 to 1990 | 735 | 0.3 |
| 1991 to 2000 | 1,582 | 0.6 |
| 2000 to 2010 | 11,234 | 4.2 |
| 2011 to 2013 | 4,380 | 1.6 |
| 2014 to 2016 | 6,164 | 2.3 |
| 2017 to 2019 | 6,469 | 2.4 |
| 2020 to 2021 | 2,893 | 1.1 |
| Total | 267,015 | 100 |
From the 2021 Census, examining age of arrival in the UK and length of time in UK, there were 232,051 residents who were born in the UK, around 9,000-9,600 foreign-born residents of Hull arrived in the UK for each of the three age groups: 0-15, 16-24 and 25-34 years, with fewer people aged 35+ years when they first arrived in the UK. The number of foreign-born residents of Hull who first arrived in the UK when they were aged 65+ years was low – being only 188 residents. It is possible that the majority of these people are relatives of people who are already living in the UK.
Under 2% of Hull residents had been in the UK for less than two years. The majority of Hull’s residents who had not been born in the UK had been in the UK for five or more years.
| Age of arrival in UK (N) | Born in UK | In UK 10+ years | In UK 5-<10 years | In UK 2-<5 years | In UK <2 years | Total |
| Born in UK | 232,051 | 232,051 | ||||
| Aged 0-15 | 4,725 | 2,221 | 1,453 | 903 | 9,302 | |
| Aged 16-24 | 4,413 | 2,288 | 1,550 | 1,342 | 9,593 | |
| Aged 25-34 | 3,938 | 2,286 | 1,535 | 1,291 | 9,050 | |
| Aged 35-49 | 1,881 | 1,632 | 1,094 | 907 | 5,514 | |
| Aged 50-64 | 342 | 350 | 364 | 264 | 1,320 | |
| Aged 65+ | 39 | 41 | 49 | 59 | 188 | |
| Total | 232,051 | 15,338 | 8,818 | 6,045 | 4,766 | 267,018 |
More than four in ten of those not born in the UK had arrived in the UK 10 years or more ago (43.9%), one-quarter (25.2%) five years or more but less than ten years ago, 17.3% two years or more but less than five years ago, and 13.6% had arrived in the UK within the last two years.
Eight in ten of foreign-born residents of Hull had first arrived in the UK prior to the age of 35 years with an additional 15.8% arriving when they were aged 35-49 years.
| Age of arrival in UK (%) | In UK 10+ years | In UK 5-<10 years | In UK 2-<5 years | In UK <2 years | Total |
| Aged 0-15 | 13.5 | 6.4 | 4.2 | 2.6 | 26.4 |
| Aged 16-24 | 12.6 | 6.5 | 4.4 | 3.8 | 27.4 |
| Aged 25-34 | 11.3 | 6.5 | 4.4 | 3.7 | 25.9 |
| Aged 35-49 | 5.4 | 4.7 | 3.1 | 2.6 | 15.8 |
| Aged 50-64 | 1.0 | 1.0 | 1.0 | 0.8 | 3.8 |
| Aged 65+ | 0.1 | 0.1 | 0.1 | 0.2 | 0.5 |
| Total | 43.9 | 25.2 | 17.3 | 13.6 | 100 |
Half of children and young people who had first arrived in the UK aged 0-15 years had lived in the UK for ten or more years with almost a further quarter lived in the UK five or more years but fewer than ten years.
As age of arrival in the UK increased, people were more less likely to have been in the UK for ten or more years.
The lowest percentage of people who had lived in the UK for ten or more years was among those people who had first arrived in the UK when they were aged 65+ years where just over one in five (21%) had lived in the UK for ten or more years, although as noted above there were only 188 residents of Hull who were foreign-born who had first moved to the UK when they were aged 65+ years so relatively small numbers.
The time in the UK and the age of arrival in the UK reflects the increased migration in the last decade combined with the usual age of migrants when they first arrive in a new country.
| Age of arrival in UK (%) | In UK 10+ years | In UK 5-<10 years | In UK 2-<5 years | In UK <2 years | Total |
| Aged 0-15 | 50.8 | 23.9 | 15.6 | 9.7 | 100 |
| Aged 16-24 | 46.0 | 23.9 | 16.2 | 14.0 | 100 |
| Aged 25-34 | 43.5 | 25.3 | 17.0 | 14.3 | 100 |
| Aged 35-49 | 34.1 | 29.6 | 19.8 | 16.4 | 100 |
| Aged 50-64 | 25.9 | 26.5 | 27.6 | 20.0 | 100 |
| Aged 65+ | 20.7 | 21.8 | 26.1 | 31.4 | 100 |
| Total | 43.9 | 25.2 | 17.3 | 13.6 | 100 |
Of those who had been in the UK ten or more years, 31% had been 0-15 years when they first arrived in the UK, 29% had been aged 16-24 years and 26% had been aged 25-34 years. Of those who had been in the UK for five or more years but fewer than ten years, and for two or more years but fewer than five years, one-quarter had first arrived for each of the age groups 0-15, 16-24 and 25-34 years. The age distribution of first arrival in the UK was slightly different among those who had first arrived in the UK in the last two years with 19% aged 0-15 years when they first arrived, 28% aged 16-24, 27% aged 35-49 and 19% aged 35-49 years when they first arrived in the UK.
| Age of arrival in UK (%) | In UK 10+ years | In UK 5-<10 years | In UK 2-<5 years | In UK <2 years | Total |
| Aged 0-15 | 30.8 | 25.2 | 24.0 | 18.9 | 26.6 |
| Aged 16-24 | 28.8 | 25.9 | 25.6 | 28.2 | 27.4 |
| Aged 25-34 | 25.7 | 25.9 | 25.4 | 27.1 | 25.9 |
| Aged 35-49 | 12.3 | 18.5 | 18.1 | 19.0 | 15.8 |
| Aged 50-64 | 2.2 | 4.0 | 6.0 | 5.5 | 3.8 |
| Aged 65+ | 0.3 | 0.5 | 0.8 | 1.2 | 0.5 |
| Total | 100 | 100 | 100 | 100 | 100 |
The highest number of foreign-born Hull residents by current age (at the time of the Census) and age of arrival in the UK were people aged 35-49 years who first arrived in the UK when they were aged 25-34 years (5,400), people who are aged 25-34 years who first arrived in the UK when they were aged 16-24 years (4,311), children and young people aged under 16 years (3,816) and people aged 35-49 years who first arrived in the UK when they were aged 35-49 years (3,042).
| Age of arrival in UK | Aged 0-15 now | Aged 16-24 now | Aged 25-34 now | Aged 35-49 now | Aged 50-64 now | Aged 65+ now | Total |
| Born in UK | 49,322 | 26,662 | 32,765 | 39,106 | 44,776 | 39,420 | 232,051 |
| Aged 0-15 | 3,816 | 2,917 | 1,020 | 682 | 607 | 256 | 9,298 |
| Aged 16-24 | 2,227 | 4,311 | 2,583 | 233 | 239 | 9,593 | |
| Aged 25-34 | 2,941 | 5,400 | 545 | 165 | 9,051 | ||
| Aged 35-49 | 3,042 | 2,310 | 160 | 5,512 | |||
| Aged 50-64 | 925 | 395 | 1,320 | ||||
| Aged 65+ | 188 | 188 | |||||
| Total | 53,138 | 31,806 | 41,037 | 50,813 | 49,396 | 40,823 | 267,013 |
The majority of Hull residents who were not born in the UK and were aged 0-15 years when they first arrived in the UK were aged under 25 years (at the time of the Census) with 41% aged 0-15 years and 31% aged 16-24 years.
Almost 45% of Hull residents who first arrived in the UK when they were aged 16-24 years were aged 25-49 years at the time of the Census with the remaining split between 16-24 and 35-49 years (with very few currently aged 50+ years).
Six in ten of foreign-born Hull residents who first arrived in the UK when they were aged 25-34 years were aged 35-49 at the time of the Census with almost a third currently aged 25-34 years.
Over half of Hull residents not born in the UK who first arrived in the UK when they were aged 35-49 years were still in the same age band at the time of the Census with an additional 42% aged 50-64 years at the time of the Census (although the age band is slightly wider than the younger age bands so it might be expected that more are within the same age band at the time of the Census compared to their age when they first arrived in the UK).
| Age of arrival in UK | Aged 0-15 now | Aged 16-24 now | Aged 25-34 now | Aged 35-49 now | Aged 50-64 now | Aged 65+ now | Total |
| Aged 0-15 | 41.0 | 31.4 | 11.0 | 7.3 | 6.5 | 2.8 | 100 |
| Aged 16-24 | 23.2 | 44.9 | 26.9 | 2.4 | 2.5 | 100 | |
| Aged 25-34 | 32.5 | 59.7 | 6.0 | 1.8 | 100 | ||
| Aged 35-49 | 55.2 | 41.9 | 2.9 | 100 | |||
| Aged 50-64 | 70.1 | 29.9 | 100 | ||||
| Aged 65+ | 100 | 100 | |||||
| Total | 10.9 | 14.7 | 23.7 | 33.5 | 13.2 | 4.0 | 100 |
Among Hull residents aged 0-15 years (at the time of the 2021 Census), 92.8% were born in the UK. Over nine in ten residents of Hull who were aged 50-64 years at the time of the Census were also born in the UK, and the percentage was even higher among Hull residents aged 65+ years at 97%.
The percentages born in the UK were lower among those aged 16-49 years.
Among all Hull residents aged 16-24 years, 9.2% were foreign-born and had first arrived in the UK when they were aged 0-15 years and 7.0% were foreign-born and had first arrived in the UK when they were aged 16-24 years.
Among all Hull residents aged 25-34 years, 20.2% were foreign-born which included 10.5% who were aged 16-24 years and 7.2% who were aged 25-34 years when they first arriving in the UK.
Among all Hull residents aged 35-49 years, 23.0% were foreign-born which included 10.6% who were aged 25-3 years, 6.0% who were aged 35-49 years and 5.1% who were aged 16-24 years when they first arriving in the UK.
| Age of arrival in UK | Aged 0-15 now | Aged 16-24 now | Aged 25-34 now | Aged 35-49 now | Aged 50-64 now | Aged 65+ now | Total |
| Born in UK | 92.8 | 83.8 | 79.8 | 77.0 | 90.6 | 96.6 | 86.9 |
| Aged 0-15 | 7.2 | 9.2 | 2.5 | 1.3 | 1.2 | 0.6 | 3.5 |
| Aged 16-24 | 7.0 | 10.5 | 5.1 | 0.5 | 0.6 | 3.6 | |
| Aged 25-34 | 7.2 | 10.6 | 1.1 | 0.4 | 3.4 | ||
| Aged 35-49 | 6.0 | 4.7 | 0.4 | 2.1 | |||
| Aged 50-64 | 1.9 | 1.0 | 0.5 | ||||
| Aged 65+ | 0.5 | 0.1 | |||||
| Total | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
Of Hull residents who were foreign-born, from their current age (at the time of the Census) and the age when they first arrived in the UK, for all current age groups aged 16+ years, the majority were within a younger age band when they first arrived in the UK compared to their current age.
| Age of arrival in UK | Aged 0-15 now | Aged 16-24 now | Aged 25-34 now | Aged 35-49 now | Aged 50-64 now | Aged 65+ now | Total |
| Aged 0-15 | 100 | 56.7 | 12.3 | 5.8 | 13.1 | 18.2 | 26.6 |
| Aged 16-24 | 43.3 | 52.1 | 22.1 | 5.0 | 17.0 | 27.4 | |
| Aged 25-34 | 35.6 | 46.1 | 11.8 | 11.8 | 25.9 | ||
| Aged 35-49 | 26.0 | 50.0 | 11.4 | 15.8 | |||
| Aged 50-64 | 20.0 | 28.2 | 3.8 | ||||
| Aged 65+ | 13.4 | 0.5 | |||||
| Total | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
There is a ‘migrant status’ variable recorded in the Census which is defined on the basis of the address one year earlier, and is categorised as migration within the UK as well as migration into the UK within the last year.
Among the 267,022 residents of Hull, 234,762 (87.9%) were living at the same address at the time of the 2021 Census as they were one year ago. A further 2,015 (0.8%) Hull residents had been living at a different address one year ago which was a student term-time or boarding school address in the UK. The remaining 27,017 (10.1%) Hull residents were living at a different address one year ago with that address in the UK for 25,002 (9.4%) of Hull residents and outside the UK for 2,015 (0.8%) of Hull residents. For 3,090 Hull residents, their prior address was not applicable as they were infants aged under one year.
Overall, there were 2,015 Hull residents who had been living at an address outside the UK one year prior to the Census, 262 of these had been born in the UK and 1,753 were foreign-born.
As mentioned earlier, as the Census is a count of residents at the time of the Census, it will not capture previous residents of Hull who were living in Hull one year prior to the Census who have moved out of Hull to other parts of the UK or abroad. So this table reflects migration in one direction only whether that is people moving into Hull from abroad, moving into Hull other parts of the UK, or moving home within Hull. It is likely that a sizeable percentage of people who are recorded as living at a different address in the UK one year prior to the Census were living in Hull (or perhaps surrounding areas such as East Riding of Yorkshire) one year prior to the Census and their address change was within the local area. This will be particularly the case among older ages. Young people who are transitioning between school and further education or work will be more likely to have moved address in the last year perhaps from further afield. Families with school-aged children are also perhaps more likely to move as are people of working-age for work purposes.
| Born in UK or not | Address one year before Census | <15 | 16-24 | 25-34 | 35-49 | 50-64 | 65+ | Total |
| Born in UK | Infant | 3,073 | 3,073 | |||||
| Same | 42,346 | 19,221 | 27,564 | 36,353 | 43,082 | 38,482 | 207,048 | |
| Student | 2 | 1,722 | 91 | 3 | 1 | 0 | 1,819 | |
| Different in UK | 3,878 | 5,665 | 5,033 | 2,717 | 1,644 | 917 | 19,854 | |
| Non-UK | 25 | 56 | 78 | 33 | 49 | 21 | 262 | |
| Total | 49,324 | 26,664 | 32,766 | 39,106 | 44,776 | 39,420 | 232,056 | |
| Not born in UK | Infant | 17 | ||||||
| Same | 3,000 | 3,271 | 5,978 | 10,068 | 4,086 | 1,311 | 27,714 | |
| Student | 0 | 275 | 48 | 8 | 3 | 0 | 334 | |
| Different in UK | 527 | 1,153 | 1,735 | 1,249 | 422 | 62 | 5,148 | |
| Non-UK | 271 | 445 | 512 | 384 | 110 | 31 | 1,753 | |
| Total | 3,815 | 5,144 | 8,273 | 11,709 | 4,621 | 1,404 | 34,966 | |
| All | Infant | 3,090 | ||||||
| Same | 45,346 | 22,492 | 33,542 | 46,421 | 47,168 | 39,793 | 234,762 | |
| Student | 2 | 1,997 | 139 | 11 | 4 | 0 | 2,153 | |
| Different in UK | 4,405 | 6,818 | 6,768 | 3,966 | 2,066 | 979 | 25,002 | |
| Non-UK | 296 | 501 | 590 | 417 | 159 | 52 | 2,015 | |
| Total | 53,139 | 31,808 | 41,039 | 50,815 | 49,397 | 40,824 | 267,022 |
The column percentages are given below for each age group. Not surprisingly, the oldest residents of Hull aged 50+ years were the most likely to be living at the same address one year before the Census with over 95% living at the same address. Hull residents aged 16-24 years were the least likely to be living at the same address with only 70% living at the same address at the time of the Census as they had been one year prior to this.
| Born in UK or not | Address one year before Census | <15 | 16-24 | 25-34 | 35-49 | 50-64 | 65+ | Total |
| Born in UK | Infant | 5.8 | 1.2 | |||||
| Same | 79.7 | 60.4 | 67.4 | 71.5 | 87.2 | 94.3 | 77.5 | |
| Student | 0.0 | 5.4 | 0.2 | 0.0 | 0.0 | 0.0 | 0.7 | |
| Different in UK | 7.3 | 17.8 | 12.3 | 5.3 | 3.3 | 2.2 | 7.4 | |
| Non-UK | 0.0 | 0.2 | 0.2 | 0.1 | 0.1 | 0.1 | 0.1 | |
| Total | 92.8 | 83.8 | 79.8 | 77.0 | 90.6 | 96.6 | 86.9 | |
| Not born in UK | Infant | 0.0 | 0.0 | |||||
| Same | 5.6 | 10.3 | 14.6 | 19.8 | 8.3 | 3.2 | 10.4 | |
| Student | 0.0 | 0.9 | 0.1 | 0.0 | 0.0 | 0.0 | 0.1 | |
| Different in UK | 1.0 | 3.6 | 4.2 | 2.5 | 0.9 | 0.2 | 1.9 | |
| Non-UK | 0.5 | 1.4 | 1.2 | 0.8 | 0.2 | 0.1 | 0.7 | |
| Total | 7.2 | 16.2 | 20.2 | 23.0 | 9.4 | 3.4 | 13.1 | |
| All | Infant | 5.8 | 1.2 | |||||
| Same | 85.3 | 70.7 | 81.7 | 91.4 | 95.5 | 97.5 | 87.9 | |
| Student | 0.0 | 6.3 | 0.3 | 0.0 | 0.0 | 0.0 | 0.8 | |
| Different in UK | 8.3 | 21.4 | 16.5 | 7.8 | 4.2 | 2.4 | 9.4 | |
| Non-UK | 0.6 | 1.6 | 1.4 | 0.8 | 0.3 | 0.1 | 0.8 | |
| Total | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
For all ages, Hull residents who were foreign-born were less likely to be living in the same address at the time of the Census compared to one year prior to this, and whilst by definition there was a higher percentage who had been living outside the UK one year prior the Census, the percentage not living at the same address were mainly because they had been living at a different address in the UK one year prior to the Census (rather than living abroad). This could denote more transient populations simply as a result of their generally younger age, but this occurred for all age groups, so suggests that perhaps accommodation is less stable for foreign-born residents of Hull.
| Born in UK or not | Address one year before Census | <15 | 16-24 | 25-34 | 35-49 | 50-64 | 65+ | Total |
| Born in UK | Infant | 6.2 | 1.3 | |||||
| Same | 85.9 | 72.1 | 84.1 | 93.0 | 96.2 | 97.6 | 78.2 | |
| Student | 0.0 | 6.5 | 0.3 | 0.0 | 0.0 | 0.0 | 0.8 | |
| Different in UK | 7.9 | 21.2 | 15.4 | 6.9 | 3.7 | 2.3 | 8.6 | |
| Non-UK | 0.1 | 0.2 | 0.2 | 0.1 | 0.1 | 0.1 | 0.1 | |
| Total | 100 | 100 | 100 | 100 | 100 | 100 | 100 | |
| Not born in UK | Infant | 0.4 | 0.0 | |||||
| Same | 78.6 | 63.6 | 72.3 | 86.0 | 88.4 | 93.4 | 79.3 | |
| Student | 0.0 | 5.3 | 0.6 | 0.1 | 0.1 | 0.0 | 0.1 | |
| Different in UK | 13.8 | 22.4 | 21.0 | 10.7 | 9.1 | 4.4 | 14.7 | |
| Non-UK | 7.1 | 8.7 | 6.2 | 3.3 | 2.4 | 2.2 | 5.0 | |
| Total | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
Local and International Migration in Hull
The mid-year resident population estimates from the Office for National Statistics, give information on the number of births and deaths as well as estimates of migration for successive mid-year estimates. The mid-year population resident population estimates for Hull were 268,677 for 2022 and 271,942 for 2023. Between July 2022 and July 2023, there were 3,067 births and 2,749 deaths among Hull residents between July 2022 and July 2023 equating to a natural reduction in population of 318 people, but the largest differences were due to migration with people leaving Hull to move to other parts of the UK (reducing the population by 1.1%) and migration with people moving into Hull from abroad (increasing the population by 2.1%). It is likely that a number of people moving into Hull from abroad will be students. There were an additional 73 people living in Hull due to other changes such as those due to the prison population or armed forces.
| Component of change | Number of people | Percentage (of 2022 population) |
| Births to Hull residents | 3,067 | 1.1 |
| Deaths to Hull residents | 2,749 | 1.0 |
| Natural change | 318 | 0.1 |
| Internal migration into Hull | 11,686 | 4.3 |
| Internal migration out of Hull | 14,580 | 5.4 |
| Internal migration – net change | -2, 890 | -1.1 |
| International migration into Hull | 7,524 | 2.8 |
| International migration out of Hull | 1,756 | 0.7 |
| International migration – net change | 5,768 | 2.1 |
| Other net change | 73 | 0.0 |
| Overall net change in population | 3,265 | 1.2 |
These components of change are also available for different ages, and as expected the size of the different population changes differs by age. The largest changes occurred in the youngest age group due to births, oldest age group due to deaths and the middle age group due to migration.
The highest levels of both internal and international migration occurred among people aged 25-39 years with a decrease in the population due to internal migration and an increase in the population due to international migration.
| Population or component of change | Aged 0-17 | Aged 18-24 | Aged 25-39 | Aged 40-64 | Aged 65+ |
| Population 2022 | 59,881 | 24,649 | 60,390 | 81,479 | 41,738 |
| Population 2023 | 61,0745 | 24,491 | 62,667 | 81,405 | 42,304 |
| Births | 3,067 | ||||
| Deaths | 15 | 5 | 59 | 470 | 2,200 |
| Natural net change | 3,052 | -5 | -59 | -470 | -2,200 |
| Internal – in | 1,483 | 3,659 | 3,854 | 1,937 | 753 |
| Internal – out | 2,066 | 3,807 | 5,098 | 2,761 | 848 |
| Internal – net | -583 | -148 | -1,244 | -824 | -95 |
| International – in | 2,064 | 986 | 3,517 | 928 | 29 |
| International – out | 170 | 380 | 780 | 404 | 22 |
| International – net | 1,894 | 606 | 2,737 | 524 | 7 |
| Migration net change | 1,311 | 458 | 1,493 | -300 | -88 |
| Special changes* | 0 | -32 | 84 | 52 | -31 |
| Overall change | 4,363 | 421 | 1,518 | -718 | -2,319 |
As a percentage of the 2022 population in terms of migration, the largest percentage increases occurred for people aged 25-39 years as there was a 2.5% increase in the 2023 population from the 2022 population due to migration (made up of a 2.0% decrease in the population due to internal migration and a 4.5% increase in the population due to international migration). The second highest change due to migration occurred in the 0-17 year age groups with an increase of 2.2% in the 2023 population from the 2022 population due to migration (made up of a 1.0% decrease in the population due to internal migration and a 3.2% increase in the population due to international migration). It might be suggested by this, that families with children are leaving Hull to perhaps surrounding areas in East Riding of Yorkshire and people coming into Hull from abroad are also made up of families with children. The third highest change due to migration occurred in the 18-24 year age groups with an increase of 1.9% in the 2023 population from the 2022 population due to migration (made up of a 0.6% decrease in the population due to internal migration and a 2.5% increase in the population due to international migration). Young people do tend to move into cities and a number of these people are likely to be students.
There were fewer people aged 40+ years who moved into or out of Hull particularly among those aged 65+ years. There was an increase in the population aged 40-64 years between 2022 and 2023 due to people moving into Hull from abroad, and whilst this was also the case for those aged 65+ years the numbers were very small. For both age groups, there was also a decrease in the population between 2022 and 2023 due to people moving out of Hull into other parts of the UK (again with numbers relatively small for those aged 65+ years). However, the numbers of people moving out of Hull were greater than the numbers moving into Hull, so there was a decrease in the overall population for both of these age groups due to migration.
| Population or component of change | Aged 0-17 | Aged 18-24 | Aged 25-39 | Aged 40-64 | Aged 65+ |
| Population 2023 | 102.0 | 99.4 | 102.9 | 99.9 | 101.4 |
| Births | 5.1 | ||||
| Deaths | 0.0 | 0.0 | 0.1 | 0.6 | 5.3 |
| Natural net change | 5.1 | -0.0 | -0.1 | -0.6 | -5.3 |
| Internal – in | 2.5 | 14.8 | 6.3 | 2.4 | 1.8 |
| Internal – out | 3.5 | 15.4 | 8.4 | 3.4 | 2.0 |
| Internal – net | -1.0 | -0.6 | -2.0 | -1.0 | -0.2 |
| International – in | 3.4 | 4.0 | 5.8 | 1.1 | 0.1 |
| International – out | 0.3 | 1.5 | 1.3 | 0.5 | 0.1 |
| International – net | 3.2 | 2.5 | 4.5 | 0.6 | 0.0 |
| Migration net change | 2.2 | 1.9 | 2.5 | -0.4 | -0.2 |
| Special changes* | 0.0 | -0.1 | 0.1 | 0.1 | -0.1 |
| Overall change | 7.3 | 1.7 | 2.5 | -0.9 | -5.6 |
Migration Yorkshire Dashboard
Migration Yorkshire have produced a dashboard which examines trends in migration in the Yorkshire region with much of the information available at local authority level. The numbers of migrants is examined over time as well as the top 10 nationalities, and the sex and age profile of the migrants.
Access Migration Yorkshire Dashboard
Health Intelligence Pack for Migrant Health
The Office for Health Improvement & Disparities have published a Health Intelligence Pack for Migrant Health which gives information relation to migrants and their health across local authorities within the Yorkshire and Humber region. The link is as follows, but they have given us permission to display their dashboard on our JSNA website.
Health Intelligence Pack for Migrant Health
The information has not been updated since it was published so there might be later information available.
The local knowledge and intelligence service team have given permission for us to display their health intelligence pack on our JSNA page. You can click on the zoom icon on the bottom right hand side of the page to make the page smaller or larger, and click on the < or > icons at the bottom of the page to move to move back or forward through the pages, or click on the page numbers “1 of 20” themselves to select a specific page. On specific pages, there are options to select different groups, such as select a specific region or local authority, specific years, or filter by nationality etc.
Strategic Need and Service Provision
This section will be updated in due course.
Resources
Migration and health research: past, present and future. Goldenberg SM and Fischer F. BMC Public Health, 2023; 23: 1425. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-023-16363-7
Who counts as a migrant? Definitions and their consequences. The Migration Observatory. https://migrationobservatory.ox.ac.uk/resources/briefings/who-counts-as-a-migrant-definitions-and-their-consequences/
Irregular migration in the UK. The Migration Observatory. https://migrationobservatory.ox.ac.uk/resources/briefings/irregular-migration-in-the-uk/
The health of migrants in the UK. The Migration Observatory. https://migrationobservatory.ox.ac.uk/resources/briefings/the-health-of-migrants-in-the-uk/
Refugee and migrant health. World Health Organisation. https://www.who.int/news-room/questions-and-answers/item/refugee-and-migrant-health
Migrant health guide. UK government. https://www.gov.uk/government/collections/migrant-health-guide
Health intelligence pack for migrant health. Office for Health Improvement & Disparities. Health intelligence pack for migrant health.
Updates
This page was last updated / checked on 11 July 2025.
This page is due to be updated / checked in March 2026.
Air Pollution
This topic area covers statistics and information relating to air pollution in Hull including local strategic need and service provision. Further information is also available about Hull and the environment can be found under Geographical Area within Place, and under Climate Change within Health and Wellbeing Influences.
This page contains information from the Office for Health Improvement & Disparities’ Fingertips. Information is taken ‘live’ from the site so uses the latest available data from Fingertips and displays it on this page. As a result, some comments on this page may relate to an earlier period of time until this page is next updated (see review dates at the end of this page).
Headlines
- Humans interact with the environment constantly. These interactions affect quality of life, years of healthy life lived, and health disparities.
- One measure of air pollution is particulate matter smaller than 2.5 microns (PM2.5) and this is estimated to be 7.2 µg/m3 (annual estimate) for Hull for 2023 which is among the second in the Yorkshire and Humber region.
- For 2023, it is estimated that around 5.4% of all deaths among those aged 30+ years are attributable to air pollution in Hull.
- The air pollution levels for particulate matter smaller than 2.5 microns and the percentage of all deaths attributable to air pollution among people aged 30+ years for 2023 are the same as they were in 2020.
- Based on the Access to Healthy Assets and Hazards Index, the east of the city has the highest levels of nitrogen dioxide with levels particularly high in parts of Drypool, Sutton and Marfleet wards with rates much lower along the wards along the west edge of the Hull boundary. Based on the same index, levels of sulphur dioxide are highest along parts of Drypool, Holderness and Sutton wards along the course of the River Hull, and again the wards along the west edge of the Hull boundary have much lower levels of pollution. Based on the index, levels of particulate matter smaller than 10 microns (PM10) are high in parts of Central, Drypool, Holderness, Marfleet, Sutton and West Carr wards, but the highest levels are in North Carr ward. The lowest levels are the the far east of the city and towards the west boundary although parts of Pickering, Boothferry and Derringham have intermediate levels and it is the wards from north to south from Orchard Park towards Newington & Gipsyville and St Andrew’s & Docklands which also have the lowest levels.
- There is the potential for measures introduced to resolve one environmental problem to be detrimental to other strategies, so full consultation and engagement between the different areas and an assessment of the impacts of any council actions is essential to ensure strategies complement each other.
The Population Affected – Why Is It Important?
Air quality is the term used to describe how polluted the air we breathe is. When air quality is poor, pollutants in the air may be hazardous to people, particularly those with lung or heart conditions. There are a number of different components to air pollution, and monitoring of air quality involves measuring the atmospheric concentrations of a number of particulates and gases. However, people are not only exposed to air pollution outside the home but inside the home too. It is difficult to measure exposure to air pollution at an individual level as it depends on many factors as they are dependent on levels of emissions, the formation of pollutants, weather, topography and the environment. Household chemicals, pets and pests, temperatures, radon, microbes, particulate matter, humidity and ventilation can all influence indoor pollutants.
The UK’s air quality strategy details how the UK aims to achieve prescribed standards and objectives for a suite of air quality concentrations to protect health and the environment. These include nitrogen dioxide (NO2), sulphur dioxide (SO2) and particulate matter smaller than 10 microns (PM10), with an additional requirement for particulate matter smaller than 2.5 microns (PM2.5). Measurements are usually given as micrograms per cubic metre (µg/m3).
As people are generally more affected by one pollutant than another, locally it is felt that presenting the values of the individual pollutants rather than the Air Pollution Index (API) enables people to make more informed personal decisions. The NHS have summarised some research on lung cancer and heart failure in relation to air pollution. For a lung cancer study, each 10μg/m3 increase in PM10 led to a corresponding increase in the hazard ratio of lung cancer incidence of 1.22 (95% confidence interval 1.03 to 1.45) with no association found between lung cancer incidence and PM2.5, mono nitrogen oxide and nitrogen dioxide combined, or nitrogen dioxide. The heart failure study found an increased risk of heart failure hospitalisation or death for increases in carbon monoxide (3.5% increase in risk per increase of one part per million of pollutant), sulphur dioxide (2.4%), nitrogen dioxide (1.7%), PM2.5 (2.1%) and PM10 (1.6%). In both studies, some potential confounders were included in the model, but it is possible important confounders were not included.
Different factors influence different pollutants in relation to air pollution as illustrate by Health Matters from the Office for Health Improvement & Disparities (formerly Public Health England).
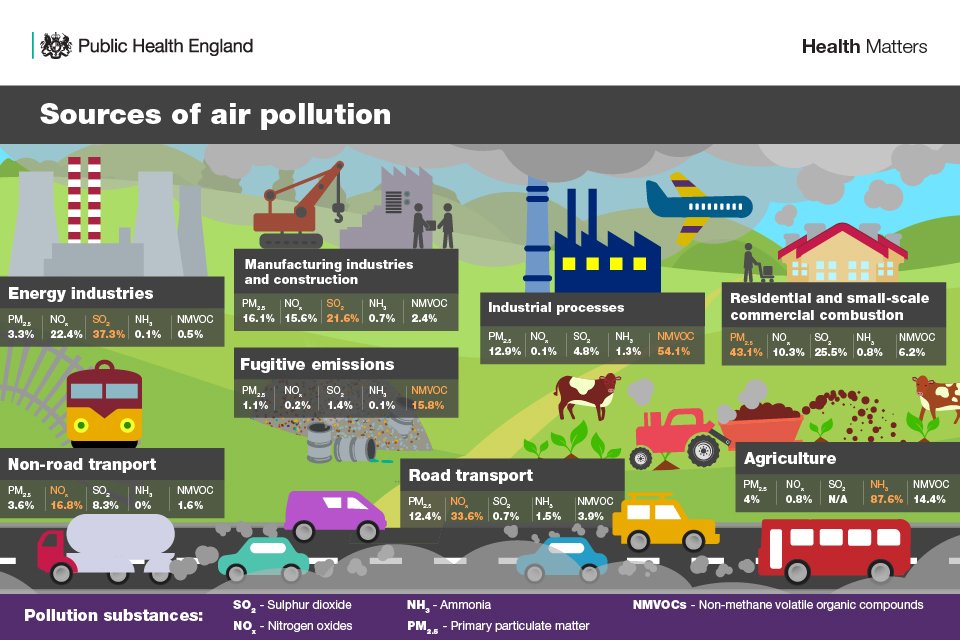
Air pollution affects individuals throughout their entire lifetime.
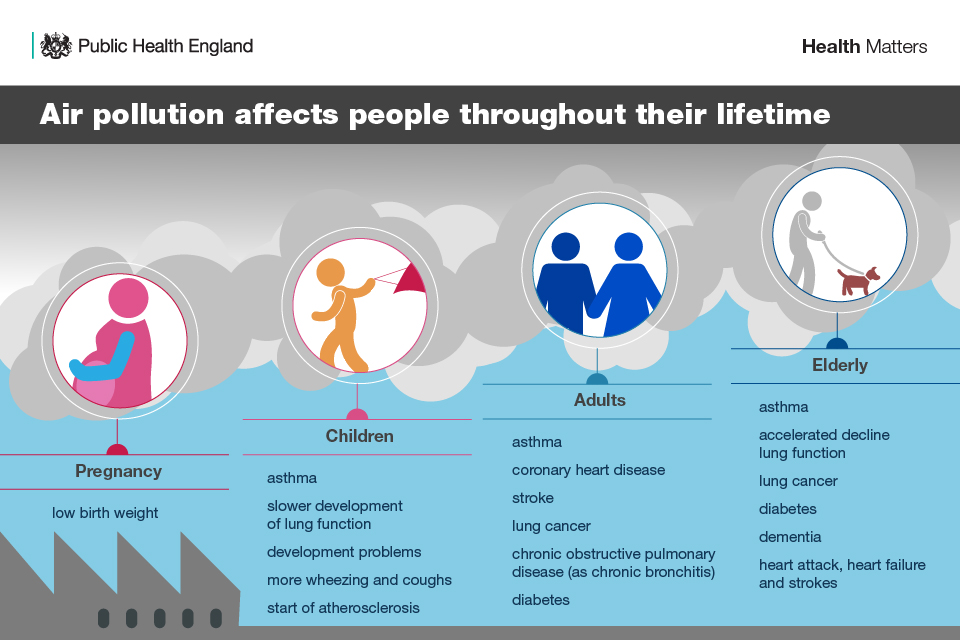
The Hull Picture
Air Quality in Hull
Hull City Council has a very good story to tell regarding air quality so far, and it measures air quality across the city, with results used to inform planning policy and applications as well as the Action Plan Measures in the Council’s Air Quality Strategy and an Annual Status Reports (ASR) which is sent to the Department for Environment, Food and Rural Affairs’ (DEFRA). Levels of mono nitrogen oxide, nitrogen dioxide, mono nitrogen oxide and nitrogen dioxide combined, sulphur dioxide, PM10 and PM2.5 are all measured.
Air quality in Hull is better than most areas of a similar nature, and is generally improving, with only one area exceeding the air quality objectives. This is an area close to the A63, and the road improvements that are ongoing are designed to remove this exceedance. The Council’s Air Quality Strategy aims to ensure that existing levels do not increase, and are reduced further wherever possible. The highest pollution concentrations are along the south edge of Hull (A63), near the train/bus station, and near the industrial areas (up the centre of Hull from South to North approximately route of river and the A1033) and around the Docks (in South-East corner (Marfleet ward) of Hull), although as mentioned only an area around the A63 exceeds the National Air Quality Objectives.
The annual concentration of fine particulate matter (PM2.5 ) at an area level, adjusted to account for population exposure is given on Fingertips. Whilst the estimate of PM2.5 is lower in Hull than England, it is among the highest across the region for 2023.
Compared with benchmark
| Indicator | Period | England | Yorkshire and the Humber region (statistical) | Kingston upon Hull | East Riding of Yorkshire | North East Lincolnshire | North Lincolnshire | York | Craven | Hambleton | Harrogate | Richmondshire | Ryedale | Scarborough | Selby | Barnsley | Doncaster | Rotherham | Sheffield | Bradford | Calderdale | Kirklees | Leeds | Wakefield |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Air pollution: fine particulate matter (new method - concentrations of total PM2.5) (Not applicable Not applicable) | 2023 | 7.0 | 6.8 | 7.2 | 6.4 | 7.3 | 7.0 | 5.9 | - | - | - | - | - | - | - | 6.9 | 7.2 | 7.4 | 7.2 | 6.9 | 6.6 | 7.0 | 7.3 | 7.1 |
| Indicator | Period | England | Yorkshire and the Humber region (statistical) | Kingston upon Hull | East Riding of Yorkshire | North East Lincolnshire | North Lincolnshire | York | Craven | Hambleton | Harrogate | Richmondshire | Ryedale | Scarborough | Selby | Barnsley | Doncaster | Rotherham | Sheffield | Bradford | Calderdale | Kirklees | Leeds | Wakefield |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Air pollution: fine particulate matter (new method - concentrations of total PM2.5) (Not applicable Not applicable) | 2023 | 7.0 | 6.8 | 7.2 | 6.4 | 7.3 | 7.0 | 5.9 | - | - | - | - | - | - | - | 6.9 | 7.2 | 7.4 | 7.2 | 6.9 | 6.6 | 7.0 | 7.3 | 7.1 |
The estimate of PM2.5 in Hull has decreased between 2018 and 2020 in line with decreases seen regionally and for England, although the decrease has been slightly greater in Hull. There was a slight decrease between 2018 and 2019, and it is likely that the greater decrease between 2019 and 2020 could be associated with the COVID-19 pandemic. There has been some variability since 2020, but the estimate for 2023 at 7.2 µg/m3 is the same as it was for 2020.
Compared with benchmark
Air pollution: fine particulate matter (new method - concentrations of total PM2.5) (Not applicable Not applicable)
|
Period
|
Kingston upon Hull |
Yorkshire and the Humber region (statistical)
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2018 | • | - | 9.8 | - | - | 8.2 | 9.5 |
| 2019 | • | - | 9.6 | - | - | 8.9 | 9.6 |
| 2020 | • | - | 7.2 | - | - | 6.6 | 7.5 |
| 2021 | • | - | 7.6 | - | - | 6.7 | 7.4 |
| 2022 | • | - | 7.5 | - | - | 6.8 | 7.8 |
| 2023 | • | - | 7.2 | - | - | 6.8 | 7.0 |
Source: Department for Environment, Food and Rural Affairs
The Access to Healthy Assets and Hazards which includes air pollution levels and was updated in 2024.
The Access to Healthy Assets and Hazards (AHAH) index is designed to allow policy and decision makers to understand which areas have poor environments for health, and to help move away from treating features of the environment in isolation.
The Access to Healthy Assets and Hazards index is comprised of four domains: access to retail services (fast food outlets, gambling outlets, pubs/bars/nightclubs, off licences, tobacconists), access to health services (GP surgeries, A&E hospitals, pharmacies, dentists and leisure centres), the physical environment (green and blue spaces) and levels of air pollution (nitrogen dioxide (NO2), particulate matter smaller than 10 microns (PM10) and sulphur dioxide (SO2)).
In 2024, the Access to Healthy Assets and Hazards Index is very high in Hull with 44.7% of Hull’s population residing in the bottom fifth of areas nationally in relation to the Access to Healthy Assets and Hazards Index. The percentage nationally is 20.9% and across the other 14 lower tier local authorities in the region the range is from 1.3% to 32.6%.
Compared with benchmark
| Indicator | Period | England | Yorkshire and the Humber region (statistical) | Kingston upon Hull | East Riding of Yorkshire | North East Lincolnshire | North Lincolnshire | York | North Yorkshire UA | Barnsley | Doncaster | Rotherham | Sheffield | Bradford | Calderdale | Kirklees | Leeds | Wakefield |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Access to Healthy Assets & Hazards Index (Persons All ages) | 2024 | 20.9 | 18.2 | 44.7 | 9.4 | 23.6 | 10.7 | 1.3 | 13.4 | 10.2 | 6.2 | 9.7 | 13.7 | 32.6 | 5.1 | 13.1 | 30.3 | 18.8 |
| Indicator | Period | England | Yorkshire and the Humber region (statistical) | Kingston upon Hull | East Riding of Yorkshire | North East Lincolnshire | North Lincolnshire | York | North Yorkshire UA | Barnsley | Doncaster | Rotherham | Sheffield | Bradford | Calderdale | Kirklees | Leeds | Wakefield |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Access to Healthy Assets & Hazards Index (Persons All ages) | 2024 | 20.9 | 18.2 | 44.7 | 9.4 | 23.6 | 10.7 | 1.3 | 13.4 | 10.2 | 6.2 | 9.7 | 13.7 | 32.6 | 5.1 | 13.1 | 30.3 | 18.8 |
Despite the very high levels in Hull, the index has decreased considerably since 2016 when nine in ten residents lived in the worst fifth of areas of England in relation to the index, although there was a large decrease between 2016 and 2017 to 46% with only relatively minor changes to 2022 and 2023.
In 2024, it is estimated that 120,220 residents in Hull live within areas defined as the bottom fifth of areas nationally based on the Access to Healthy Assets and Hazards Index.
Compared with benchmark
Access to Healthy Assets & Hazards Index (Persons All ages)
|
Period
|
Kingston upon Hull |
Yorkshire and the Humber region (statistical)
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2016 | • | 233157 | 90.0% | - | - | 22.2% | 21.2% |
| 2017 | • | 120814 | 46.3% | - | - | 14.1% | 21.1% |
| 2022 | • | 114694 | 44.3% | - | - | 19.9% | 22.6% |
| 2024 | • | 120220 | 44.7% | - | - | 18.2% | 20.9% |
Source: Consumer Data Research Centre
Information relating to version 4 of the Access to Healthy Assets and Hazards index is available at lower layer super output area geographical level. There are 33,755 lower layer super output areas in England, and the percentile score has been calculated for each of the 168 lower layer super output areas in Hull. The index was updated in July 2024, and information on the individual components is available. The air pollution data is from the Department for Environment, Farming and Rural Affairs (DEFRA) for 2022.
Levels of air pollution tend to be higher along main arterial travel routes and in areas with higher levels of industry and this is the case for Hull. Furthermore, as the prevailing wind in the UK is predominantly from the south-west, this generally means that air pollution levels tend to be higher in easterly areas.
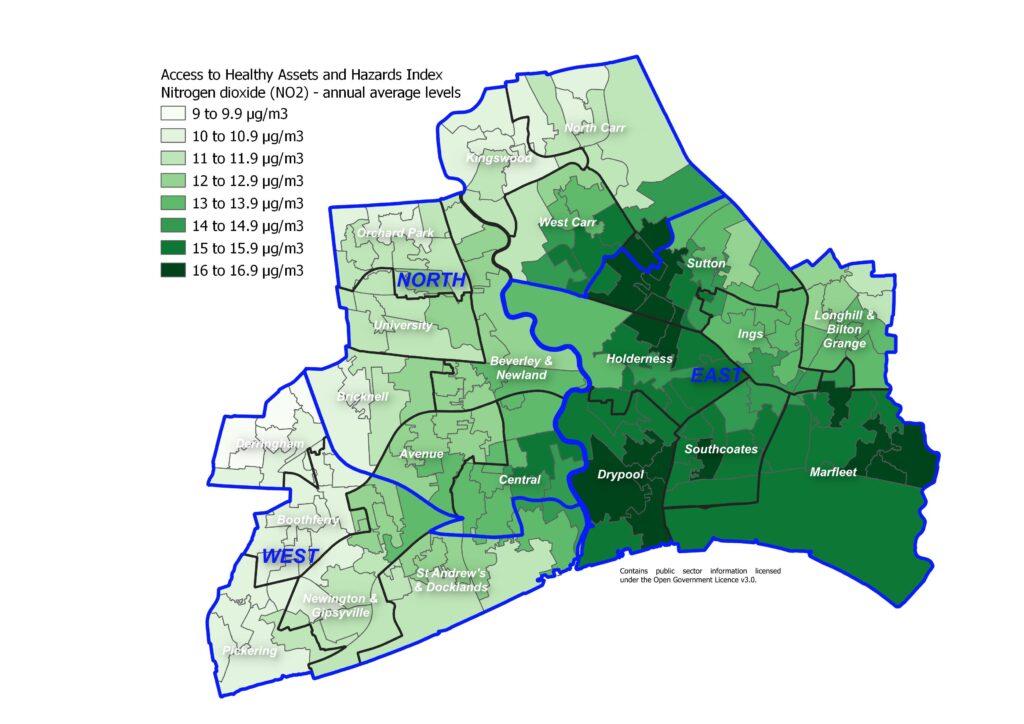
The following map illustrates the average annual levels of sulphur dioxide. There appears to be two pockets of areas with relatively high levels of sulphur dioxide in Hull and areas further away from these two areas tending to have the lowest levels compared to the Hull average.
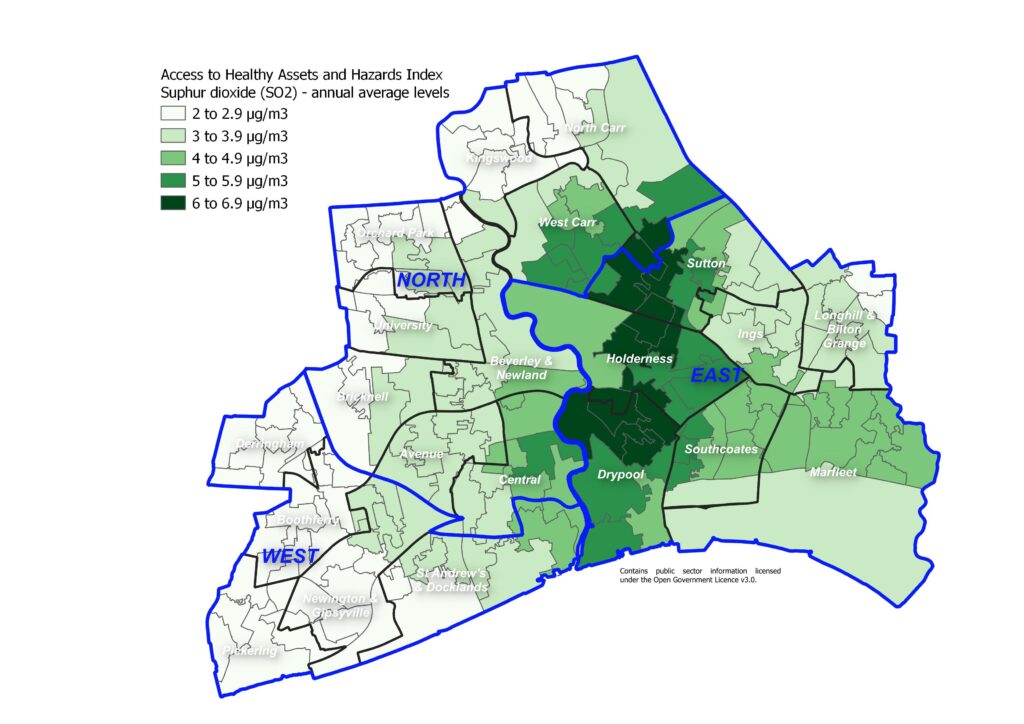
The following map illustrates the average annual levels of particulate matter with size less than 10 microns.
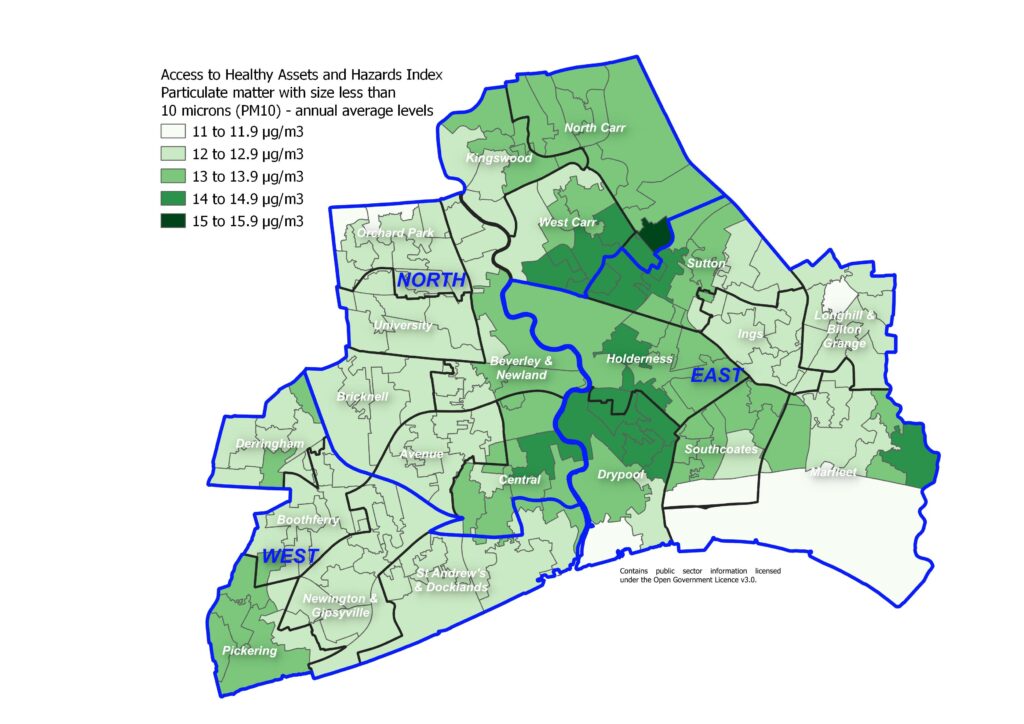
The levels of air pollution in terms of average annual levels of nitrogen dioxide, sulphur dioxide and particulate matter with size less than 10 microns are high relative to other areas of England. This is not particularly surprising as most cities with relatively high density of roads and industry compared to rural areas will tend to have relatively high levels of air pollution. Not surprisingly, the areas with the highest levels of pollution are those with the higher levels of industry and in the east where the prevailing wind will tend to increase levels of air pollution.
The percentile scores range from 68 to 100 so none of Hull’s 168 lower layer super output areas are the the best 60% nationally in terms of air pollution levels. Four in ten of Hull’s lower layer super output areas are in the worst 10% of areas of England in terms air pollution levels, and almost seven in ten of the areas are in the worst 20% nationally. All but two of Hull’s 168 lower layer super output areas are in the worst 30% of areas nationally in terms of air pollution.
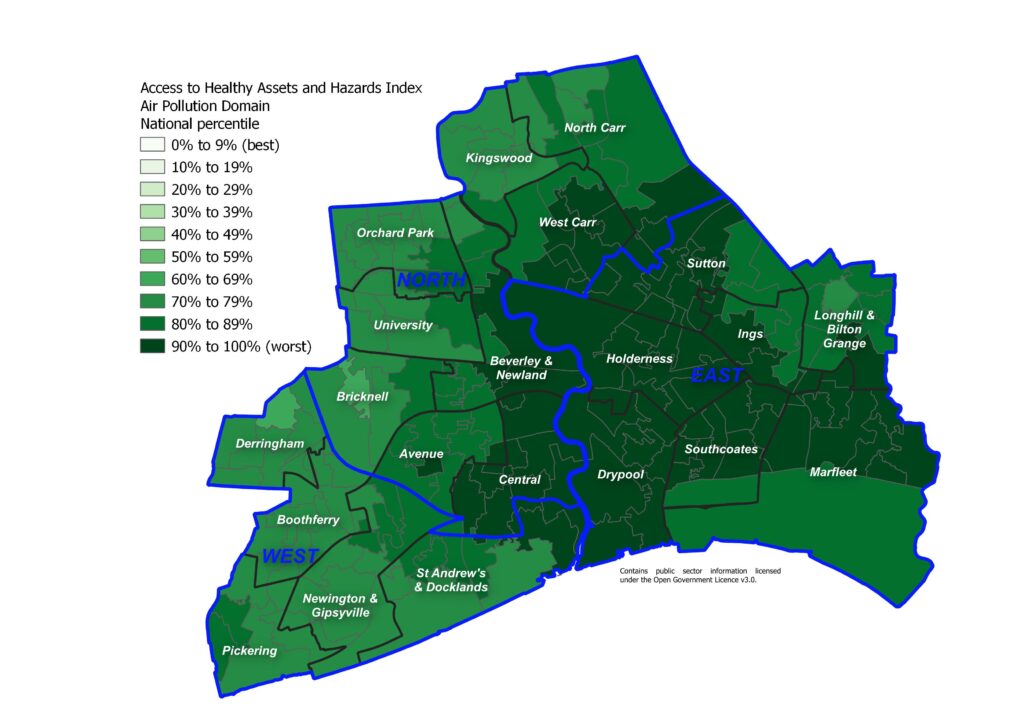
Estimated Mortality Attributable to Air Pollution
The Committee on the Medical Effects of Air Pollutants (COMEAP) estimated that if all man-made particulate pollution were removed, this would lead to an increase in life expectancy of around 6 months although the effect could be as small as one month and as large as a year. To put this into context, the effect on life expectancy of continued smoking is seven years on average. The Office for Health Improvement & Disparities’ Fingertips previously presented the percentage of deaths among those aged 30+ years attributable to air pollution. However, DEFRA’s model for Hull was found to be inaccurate, and as a result it is possible that the percentages of deaths based on these levels of air pollution may also be inaccurate.
More recently, the Office for Health Improvement & Disparities’ have used a new method to calculate the fraction of annual all cause adult mortality attributable to particulate air pollution (PM2.5). It represents the mortality burden associated with long-term exposure to particulate air pollution at current levels, expressed as a percentage of annual deaths from all causes in those aged 30+ years.
From COMPEAP (2022), a 10 µg/m3 increased in PM2.5 equates to a relative risk of 1.08 (i.e. an 8% risk), and using this information a population weighted modelled annual average background PM2.5 concentration x, RR is calculated as (1.08)(x/10) (from Public Health England, 2014). The ‘attributable fraction’ of deaths or fraction of deaths attributable to PM2.5 is expressed as a percentage, calculated as 100*(RR-1)/RR.
Population weighted annual average concentrations of PM2.5 were provided by Ricardo Energy and Environment for all lower tier and unitary local authorities within England, as well as combined at upper tier, regional and national level.
Thus with a estimate of 7.2 µg/m3 for PM2.5 for 2023 above, the relative risk for Hull would be 1.080.72 which is 1.057, and the attributable fraction would be 100*(RR-1)/RR or 100*0.057/1.057 or 5.7, i.e. 5.4% for the fractions of deaths attributable to PM2.5 in Hull for 2023.
The fraction of deaths attributable to air pollution at 5.4% is among the highest in the region.
Compared with benchmark
| Indicator | Period | England | Yorkshire and the Humber region (statistical) | Kingston upon Hull | East Riding of Yorkshire | North East Lincolnshire | North Lincolnshire | York | North Yorkshire UA | Barnsley | Doncaster | Rotherham | Sheffield | Bradford | Calderdale | Kirklees | Leeds | Wakefield |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Air pollution: estimated fraction of mortality attributable to particulate air pollution (Persons 30+ yrs) | 2023 | 5.2 | 5.1 | 5.4 | 4.8 | 5.5 | 5.2 | 4.4 | 4.2 | 5.2 | 5.4 | 5.5 | 5.4 | 5.2 | 5.0 | 5.2 | 5.5 | 5.3 |
| Indicator | Period | England | Yorkshire and the Humber region (statistical) | Kingston upon Hull | East Riding of Yorkshire | North East Lincolnshire | North Lincolnshire | York | North Yorkshire UA | Barnsley | Doncaster | Rotherham | Sheffield | Bradford | Calderdale | Kirklees | Leeds | Wakefield |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Air pollution: estimated fraction of mortality attributable to particulate air pollution (Persons 30+ yrs) | 2023 | 5.2 | 5.1 | 5.4 | 4.8 | 5.5 | 5.2 | 4.4 | 4.2 | 5.2 | 5.4 | 5.5 | 5.4 | 5.2 | 5.0 | 5.2 | 5.5 | 5.3 |
The percentage of deaths attributable to PM2.5 in Hull has decreased from 2018 and 2019 when it was over 7% to 5.4% in 2020. The percentage increased to 5.7% in 2021, but has subsequently fallen to 5.4% for 2023 which is the same as it was for 2020.
Compared with benchmark
Air pollution: estimated fraction of mortality attributable to particulate air pollution (Persons 30+ yrs)
|
Period
|
Kingston upon Hull |
Yorkshire and the Humber region (statistical)
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2018 | • | - | 7.2% | - | - | 6.1% | 7.1% |
| 2019 | • | - | 7.1% | - | - | 6.6% | 7.1% |
| 2020 | • | - | 5.4% | - | - | 5.0% | 5.6% |
| 2021 | • | - | 5.7% | - | - | 5.0% | 5.5% |
| 2022 | • | - | 5.6% | - | - | 5.1% | 5.8% |
| 2023 | • | - | 5.4% | - | - | 5.1% | 5.2% |
Source: Department for Environment, Food and Rural Affairs
The impact of air pollution on health will not affect everyone the same, and it is likely that people living in more deprived areas who are more likely to have more ill health and comorbidities are more likely to be affected by poor air quality compared to people living in less deprived areas. Housing conditions may also be worse in more deprived areas which could impact on indoor air pollution levels.
Strategic Need and Service Provision
Hull’s improving year on year trend relating to air quality has been maintained with the Council’s Air Quality Strategy, and an increase in background levels are prevented. Continuing to raise awareness of the health and financial benefits of good air quality is a key measure in encouraging behaviour change and less polluting lifestyle choices.
It is necessary to work together to maintain and expand an environment that promotes active travel for all ages in order to reduce the impact on air pollution from cars. Food production also has a substantial impact on air pollution, particularly meat and manufactured food products. Raising awareness of this and encouraging people to buy locally produced food could all help to reduce air pollution levels.
It is important that any measures in the proposed climate change strategy and proposed action plan consider the implications on and as far as possible complement those in the Air Quality Strategy, as some could have a detrimental impact on air quality. For example, monitoring during the COVID-19 lockdown indicates that as direct emissions from vehicles decrease (mono nitrogen oxide and nitrogen dioxide combined) it has the potential to result in an increase in the concentrations of other potentially harmful gases, such as ozone, and only a minimal reduction in the emissions of particulate matter. This has implications and will need to be considered when advocating a change to electric vehicles.
An Air Pollution Needs Assessment is currently underway with the aim of providing local information relating to air pollution and the impact on health and wellbeing.
Resources
HM Government, The Clean Growth Strategy: Leading the way to a low carbon future. 2017, HM Government: London.
Office for Health Improvement & Disparities’ Fingertips. https://fingertips.phe.org.uk/
Public Health England (now Office for Health Improvement & Disparities). Estimating local mortality burdens associated with particulate air pollution, 2014. https://www.gov.uk/government/publications/particulate-air-pollution-quantifying-effects-on-mortality
Hull 2020 Carbon Neutral Strategy. Hull City Council, 2020. http://www.hull.gov.uk/environment/pollution/hull-2030-carbon-neutral-strategy
Updates
This page was last updated / checked on 14 July 2025.
This page is due to be updated / checked in February 2026.
Where Do I Find The Information I Want?
Each topic has a separate page, and is arranged under different Main Menu headings as follows: Home, Population, Vulnerable Groups, Adults, Children and Young People, Place, Health and Wellbeing Influences, and Tools and Resources.
To access the Main Menu, click on Show Navigation (or box with lines) in the top right corner of the page, then click on the down arrows to go to Sub Menu items or individual topic pages.
A Contents Page / Site Map has also been produced which gives a list of all the topic pages beneath the Main Menu headings.
Under Home, Hull’s JSNA provides information on what a JSNA is, who it is for, who produces it, and information on where the statistics come from.
Under Home, the Key Facts for Hull which provides a summary of the health and wellbeing needs of Hull’s population.
Under Population, there is information on population estimates and projections, race and ethnicity, life expectancy, and causes of death.
Under the Adults and Children and Young People, there are headings for Health Factors and Lifestyle Factors. Under Adults, Health Factors covers general health, emotional wellbeing and oral health, and information relating to various diseases and medical conditions for adults including other topics such as neurodiversity, end of life and palliative care, falls and frailty, sexual health and suicide. Under Children and Young People, Health Factors covers Special Educational Needs or Disabilities, accidents and injuries, A&E attendances and hospital admissions, screening and vaccinations, and under 18 conceptions for children and young people. Lifestyle Factors includes information relating to lifestyle and behavioural risk factors, such as diet, physical activity, healthy weight, smoking, alcohol, drugs and gambling. There is another subheading for adults for Prevention which covers vaccinations and screening including the NHS Health Check. Within the Children and Young People menu, there are two further submenus: Pregnancy and Infants which covers pregnancy and maternal health, births and infant health, breastfeeding, smoking in pregnancy, stillbirths and infant mortality, and Child Development which covers early years and good child development as well as providing information on Hull’s Early Help and Prevention programme.
Under Vulnerable Groups, there is further information on specific groups such as carers, children in care and care leavers, gender identity and LGTBQ+, Gypsy and Travellers, and people who are homeless, people who have learning disabilities, people who have mental ill health, people who have multiple unmet needs, people with sensory impairment and Veterans.
Under Health and Wellbeing Influences, there is information on some of the wider determinants of health and wellbeing which include deprivation and poverty, housing, air pollution, climate change, schools, education and qualifications, employment, economy and healthy workplaces, young people not in education, employment or training, crime, domestic abuse, and financial resilience.
Under Place, there is further information about Hull as a geographical area, and health and wellbeing profiles for each electoral ward and Area Committee Area in Hull as well information on primary care and Hull’s GP practices and Primary Care Networks (groups of GP practices).
Under Tools and Resources, further information can be found on Hull’s Adult and Young People Health and Wellbeing Surveys and a summary of the prevalence of various diseases and medical conditions at GP practice level throughout Hull (from the Quality and Outcomes Framework data) as well as links to our Glossary, and links to other associated documents such as the Director of Public Health Annual reports, the local Health and Wellbeing Strategy, and Hull’s Pharmaceutical Needs Assessment. This section also provide information on where to report an outbreak of an infectious disease or other health-related issue (such as noise) as well as our contact details if you would like further information or have questions relating to health and wellbeing needs of Hull’s population or relating to Hull’s Joint Strategic Needs Assessment.
If you require further information please Contact Us.
Updates
This page was last updated on 19 March 2025.
This page is due to be updated / checked in March 2026.
Contents Page / Site Map
Each topic has a separate page.
The pages can be accessed through the Main Menu which is shown by clicking on Show Navigation (or by clicking on the square box with lines in at the top right corner of the website).
Once the Main Menu is shown, you can click on the down arrows beside each topic to access all the Sub Menus or individual topic pages.
Under the Main Menu or Sub Menus, all the individual topic pages are listed. Click on the name of the page to access the page you require.
Note that each Main Menu item and Sub Menu item also has a page to itself, so if you click on these main menu or sub menu items you will go to that page rather then the individual topic areas beneath them. Click on the down arrows to go to items below. All these main menu and sub menu pages include links to all the pages below them in the menu hierarchy so you can use these pages to navigate too.
Once you open a page (a Main Menu page, Sub Menu page or an individual topic page) at the top of the screen, it says “You are here: ……” You can click on the links to move back up to the Main Menu or access the Home page from here.
There is a lot of overlap between topic areas, but the following table provides a list of all the topic pages (site map) and where the topics are in the menu hierarchy in relation to the Main Menu and Sub Menus.
At the top of each page, there is a section which gives information on where associated information can be found. For instance, on the Population Estimates page, there is a link to the Population Projections page.
| Main Menu | Sub Menu | Individual Topic Page |
| Home | Hull’s JSNA (about the JSNA) | |
| Home | Key Facts for Hull | |
| Population | Population Estimates | |
| Population | Race and Ethnicity | |
| Population | Population Projections | |
| Population | Life Expectancy and Healthy Life Expectancy | |
| Population | Causes of Death | |
| Vulnerable Groups | Carers | |
| Vulnerable Groups | Looked After Children and Care Leavers | |
| Vulnerable Groups | Gender Identity and LGBTQ+ | |
| Vulnerable Groups | Gypsy and Travellers | |
| Vulnerable Groups | Homelessness | |
| Vulnerable Groups | Learning Disabilities | |
| Vulnerable Groups | Mental Ill Health | |
| Vulnerable Groups | Multiple Unmet Needs | |
| Vulnerable Groups | Sensory Impairment | |
| Vulnerable Groups | Veterans | |
| Adults | Health Factors | Physical Health |
| Adults | Health Factors | Mental Health and Emotional Wellbeing |
| Adults | Health Factors | Cancer |
| Adults | Health Factors | Cardiovascular Disease |
| Adults | Health Factors | Coronavirus (COVID-19) |
| Adults | Health Factors | Dementia |
| Adults | Health Factors | Diabetes |
| Adults | Health Factors | Falls and Frailty |
| Adults | Health Factors | Infectious Diseases |
| Adults | Health Factors | Kidney Disease |
| Adults | Health Factors | Musculoskeletal Disorders |
| Adults | Health Factors | Neurodiversity |
| Adults | Health Factors | Oral Health |
| Adults | Health Factors | Palliative Care and End of Life |
| Adults | Health Factors | Respiratory Disease |
| Adults | Health Factors | Sexual and Reproductive Health |
| Adults | Health Factors | Sexually Transmitted Infections |
| Adults | Health Factors | Suicide and Self-Harm |
| Adults | Lifestyle Factors | Alcohol |
| Adults | Lifestyle Factors | Diet and Nutrition |
| Adults | Lifestyle Factors | Drugs |
| Adults | Lifestyle Factors | Gambling |
| Adults | Lifestyle Factors | Healthy Weight |
| Adults | Lifestyle Factors | Physical Activity |
| Adults | Lifestyle Factors | Smoking and Vaping |
| Adults | Prevention | Screening and the NHS Health Check |
| Adults | Prevention | Vaccinations |
| Children and Young People | Health Factors | Physical Health |
| Children and Young People | Health Factors | Mental Health and Emotional Wellbeing |
| Children and Young People | Health Factors | A&E Attendances and Hospital Admissions |
| Children and Young People | Health Factors | Accidents and Injuries |
| Children and Young People | Health Factors | Children with Special Educational Needs or Disabilities |
| Children and Young People | Health Factors | Neurodiversity |
| Children and Young People | Health Factors | Oral Health |
| Children and Young People | Health Factors | Screening and Vaccinations |
| Children and Young People | Health Factors | Under 18 Conceptions |
| Children and Young People | Lifestyle Factors | Alcohol |
| Children and Young People | Lifestyle Factors | Diet and Nutrition |
| Children and Young People | Lifestyle Factors | Drugs |
| Children and Young People | Lifestyle Factors | Gambling |
| Children and Young People | Lifestyle Factors | Healthy Weight |
| Children and Young People | Lifestyle Factors | Physical Activity |
| Children and Young People | Lifestyle Factors | Smoking and Vaping |
| Children and Young People | Pregnancy and Infants | Pregnancy and Maternal Health |
| Children and Young People | Pregnancy and Infants | Births and Infant Health |
| Children and Young People | Pregnancy and Infants | Breastfeeding |
| Children and Young People | Pregnancy and Infants | Smoking in Pregnancy |
| Children and Young People | Pregnancy and Infants | Stillbirths and Infant Mortality |
| Children and Young People | Child Development | Early Years and Good Child Development |
| Children and Young People | Child Development | Early Help and Prevention Programme |
| Place | Geographical Area | |
| Place | Ward Profiles | |
| Place | Primary Care Profiles | |
| Health and Wellbeing Influences | Air Pollution | |
| Health and Wellbeing Influences | Climate Change | |
| Health and Wellbeing Influences | Crime | |
| Health and Wellbeing Influences | Deprivation and Poverty | |
| Health and Wellbeing Influences | Domestic Abuse | |
| Health and Wellbeing Influences | Employment, Economy and Healthy Workplaces | |
| Health and Wellbeing Influences | Financial Resilience | |
| Health and Wellbeing Influences | Housing and Households | |
| Health and Wellbeing Influences | Schools, Education and Qualifications | |
| Health and Wellbeing Influences | Young People Not in Education, Employment or Training | |
| Tools and Resources | Contact Us | |
| Tools and Resources | Help – Toolkits, Glossary and Finding Information | Glossary |
| Tools and Resources | Help – Toolkits, Glossary and Finding Information | Where Do I Find the Information I Want? |
| Tools and Resources | Help – Toolkits, Glossary and Finding Information | Contents Page / Site Map (this page) |
| Tools and Resources | Surveys Conducted in Hull | Local Surveys Involving Adults |
| Tools and Resources | Surveys Conducted in Hull | Local Surveys Involving Young People |
| Tools and Resources | Surveys Conducted in Hull | Other Local Surveys and Qualitative Research |
| Tools and Resources | Local Quality and Outcomes Framework Data | |
| Tools and Resources | Director of Public Health Annual Reports | |
| Tools and Resources | Health and Wellbeing Strategy | |
| Tools and Resources | Pharmaceutical Needs Assessment | |
| Tools and Resources | Reporting an Outbreak or Other Health-Related Problem |
If you cannot find the information you require, please contact us at [email protected]
Updates
This page was last updated / checked on 1 July 2025.
This page is due to be updated / checked in March 2026.
Geographical Area
This topic area covers statistics and information relating to the Hull’s physical geographical area and some information relating to the environment including local strategic need and service provision. Further demographic, health and wellbeing information relating to specific geographical areas such as electoral wards under Ward Profiles within Place. Further information on the environmental factors of Air Pollution and Climate Change can be found within Health and Wellbeing Influences.
More information relating to the population differences between the NHS geography (based on patients registered with Hull GPs) and the local authority (based on residents of Hull) and the difference in these estimates from different data sources is given on Population Estimates under Population. Further information on the differences in the type of housing and household composition within Hull can be found on Housing and Households under Health and Wellbeing Influences.
This page contains information from the Office for Health Improvement & Disparities’ Fingertips. Information is taken ‘live’ from the site so uses the latest available data from Fingertips and displays it on this page. As a result, some comments on this page may relate to an earlier period of time until this page is next updated (see review dates at the end of this page).
In July 2022, Clinical Commissioning Groups (CCGs) ceased to exist and were replaced by the Integrated Care System. Data will still be available at CCG level for some time after July 2022 so the JSNA will continue to reference CCGs and Hull CCG as well as the larger geographical area Humber, Coast and Vale which included Hull CCG. New data is becoming available for Hull’s Health and Care Partnership and is referred to as sub Integrated Care Board and referenced by 03F for Hull within Fingertips, as well as data being available for the larger local geographical area – the Humber and North Yorkshire Health and Care Partnership or Humber and North Yorkshire Integrated Care Board.
Headlines
- The geographical boundaries in Hull are tight and exclude the more affluent suburban areas unlike other cities. This means that Hull is ranked among the most deprived local authorities in England.
- It is estimated that 45% of Hull’s population live in the bottom fifth of areas nationally based on the Access to Healthy Assets and Hazards index which measures multidimensional features of the built environment including accessibility to retail services (fast food outlets, pubs, gambling stores, etc), health services, green spaces and overall air quality. The index can be considered to be a measure of the unhealthy environments present. The percentage in Hull is far greater than England (21%) and the other 14 local authorities across the Yorkshire and Humber region (range 1.3% to 32.6%). Outside the concentrated density of London (where most local authorities have the majority of the population in the bottom fifth including the City of London where all their population is included in the bottom fifth of areas), Hull has among the highest percentages being fifth highest of the 120 upper-tier local authorities outside London.
- Hull is 71.6 kilometres square and has around 4,000 residents per square kilometre. Hull is in the top 15% of lower-tier local authorities with the highest population density.
- It is likely that some people in Hull move to the ‘leafy suburbs’ in East Riding of Yorkshire just outside Hull’s boundary each year. The more aspirational, successful and motivated people will tend, on average, to have increased mobility, and this affects the employment and skills profile of Hull.
- Owing to Hull’s somewhat isolated location, people may be less likely to be influenced by positive health factors occurring elsewhere.
- The geographical boundaries for Hull local authority are the same as for Hull’s Health & Care Partnership (sub Integrated Care Board area), although the population size if different. The estimate resident population was 271,9742 people from the Office for National Statistics mid-year 2023, but the number of patients registered with Hull GPs was over 314,000 patients as at January 2024 (and around 8% of these patients live in East Riding of Yorkshire). Furthermore, the GP registration file includes almost 24,000 ‘extra’ residents compared to the Office for National Statistics resident population estimates (8% of total residents in the registration file). Some of these ‘extra’ residents are likely to be ‘ghost’ patients who are have moved away but have not registered with another GP in England (either because they haven’t been ill since moving or they moved abroad – some of which may have been students).
The Population Affected – Why Is It Important?
In order to improve health and reduce inequalities, it is important to understand the make-up of the local population, the geographical area and the environment. Features within the geographical areas, such as rivers or the location of residential, commercial and industrial areas, or the way in which boundaries have been derived can all influence the health needs of the local population, and also their access to services.
As the World Health Organisation states “Humans interact with the environment constantly. These interactions affect quality of life, years of healthy life lived, and health disparities.” WHO defines environment, as it relates to health, as all the physical, chemical, and biological factors external to a person, and all the related behaviours. From Healthy People 2020, environmental health consists of preventing or controlling disease, injury, and disability related to the interactions between people and their environment.
The World Health Organisation estimate that 24% of the global disease burden and 23% of all deaths can be attributable to environmental factors, and that this figure is higher for children aged 0-14 years (36% for deaths). The overall figures are lower in high income countries and it is estimated that this figure is around 14% on average in Europe in relation to deaths. However, there are large inequalities both between and within countries.
Environmental factors include indoor and outdoor air pollution, climate change, extreme weather events, flooding, drought, unsafe drinking water, chemical and radiation exposures, leaks and contaminations including contaminated land, exposure to lead, asbestos and other substances and chemicals, exposure to other adverse substances in the home such as mould, noise pollution, light pollution, and a number of other environmental factors.
While Hull has relatively good air quality, air pollution is a major cause of premature death and disease, and is the single largest environmental health risk in Europe according to the European Environmental Agency.
The Intergovernmental Panel on Climate Change state that we are currently experiencing the greatest change in the natural environment in human history. The threat of climate change as a result of the increase of greenhouse gases by human activity is pushing known planetary boundaries in areas such as species loss, air quality, natural resources and extreme weather events. The increasing global population expansion and dietary change is putting pressure on agriculture and land use.
As stated by the government, the transition to a low carbon society to combat these environmental threats provides challenges in energy generation and its use, urban transport to combat air quality and improve physical health and improving the resilience and adaptability of our communities particularly the most vulnerable.
The Hull Picture
About Hull
The city and port of Hull lies on the north bank of the Humber estuary and is positioned at the gateway to Europe. It is linked to the national motorway networks from the west via the M62 and to the south across the Humber Bridge via the M180. Hull’s city boundary is roughly semi-circular with a radius of approximately 4.4 miles or 7 kilometres. The city is compact and highly urbanised. It is one of the most densely populated local authorities in the Yorkshire and Humber region. Hull serves large rural and coastal areas in neighbouring local authorities, and is surrounded by the East Riding of Yorkshire to the north, east and west, and by the Humber estuary to the south. The River Hull runs through the middle of the city from north to south with industries traditionally located around the rivers of Hull and the Humber forming an inverted T-shape of industrial areas in Hull. Hull is flat and low lying which has previously resulted in problems with flooding (in 2007 due to heavy rainfall and in 2013 due to a tidal surge). With the tight urban boundary, many small towns and villages in neighbouring East Riding of Yorkshire are located on the periphery of the boundary, and generally constitute the ‘leafy suburb’ areas of the city. As a result of these more affluent suburb areas falling outside the city boundary (unlike many other local authorities where parts of these suburb areas fall within a city’s boundary), Hull is among the most deprived local authorities in England.
The Hull travel-to-work areas, which covers a large percentage of East Riding of Yorkshire, has one of the highest levels of commuter self-containment in the country. This means that Hull has high levels of visitor populations who visit Hull for work, retail and leisure purposes.
Hull has some outstanding cultural and historic assets, many of national and international significance. Hull has a good distribution of parks and open spaces, and green space makes up around a third of land use (34.4%). The largest land use is then followed by domestic gardens (20.6%), roads (13.0%), domestic buildings (8.6%), non-domestic buildings (6.4%), water (2.5%), paths (1.6%) and rail (0.6%), with the remaining 12.3% defined as other land uses. Hull is a total of 7,154 hectares.
Since Hull was announced as the UK’s City of Culture 2017, numerous multi-million pound investments have revitalised and transformed the city centre. Investments of more than £1 billion have flowed into the city, creating thousands of jobs, and over £3 billion in total from public and private investment. Thousands of volunteers helped deliver the cultural programme in 2017 with nine in ten people in Hull taking part in City of Culture events. Visitor numbers increased dramatically. Following on from its success, the City of Culture legacy has been embedded in every stage of the UK City of Culture journey and has been the topic of the 2016 Director of Public Health Annual report with a ten-year Cultural Strategy 2016-2026 launched in a bid to sustain the economic boom and “put culture and the arts at the heart of Hull’s regeneration and development”.
Hull’s Tight Geographical Boundaries
In relation to the characteristics of Hull, one problem relatively unique to Hull is its tight geographical boundaries. Most cities such as Hull are relatively deprived, but most other local authority or NHS boundaries include some more affluent suburban areas. Hull has very few affluent suburbs within its boundaries, and it is estimated that a number of people in Hull move to the ‘leafy suburbs’ in East Riding of Yorkshire just outside Hull’s boundary each year. The people that tend to move will often do so because of children and better schools, better quality and choice of housing, etc. The more aspirational, successful and motivated people will tend, on average, to have increased mobility. This also affects the employment and skills profile of Hull. Furthermore, owing to Hull’s somewhat isolated location, people may be less likely to be influenced by positive health factors and changes occurring elsewhere in other geographical areas. Due to Hull’s high levels of deprivation and tight boundaries, Hull is often at the bottom of national league tables and among the ‘worst’ for various indicators for both health and the wider determinants of health. As a result, there are often negative comments made about Hull, which can influence attitudes, health and lifestyle. Within local qualitative research projects, there were certainly some residents that had a “what’s the point?” attitude with regard to their health and lifestyle changes, however, others felt that this was just an excuse “You can lead a healthy lifestyle anywhere, it’s not the place – I staunchly defend Hull– it’s about choices”.
From the Office for National Statistics population estimates for 2022, Hull is 71.6 kilometres square and has an estimated 3,756 residents per square kilometre. Hull is in the top 15% of lower-tier local authorities in terms of having high population density.
Hull’s Location Within the Yorkshire and Humber Region
Hull is one of 15 County and Unitary Authorities, and one of 21 District Authorities in the Yorkshire and Humber region (North Yorkshire County Authority is split into seven District Authorities).

Hull’s Electoral Wards
There were 23 wards in Hull prior to May 2018 and this had been the case for more than a decade. In May 2018, the number of wards in Hull reduced to 21, and the boundary of every single ward changed. Some changes were relatively minor, but other changes were much more substantial. The names of around half of the wards remained the same despite changes to all the boundaries. These also ranged from relatively minor changes to entirely new names for some wards. Prior to April 2023, Hull was divided into seven Area Committee Areas each covering three wards with North Carr, Kingswood, and West Carr in Foredyke Area, Beverley & Newland, Orchard Park, and University in Northern Area, Ings, Longhill & Bilton Grange, and Sutton in East Area, Holderness, Marfleet, and Southcoates in Park Area, Drypool, Newington & Gipsyville, and St Andrew’s & Docklands in Riverside Area, Boothferry, Derringham, and Pickering and West Area, and Avenue, Bricknell, and Central in Wyke Area.
As at April 2023, there are three Area Committee Areas of North, East and West as illustrated in the map below.
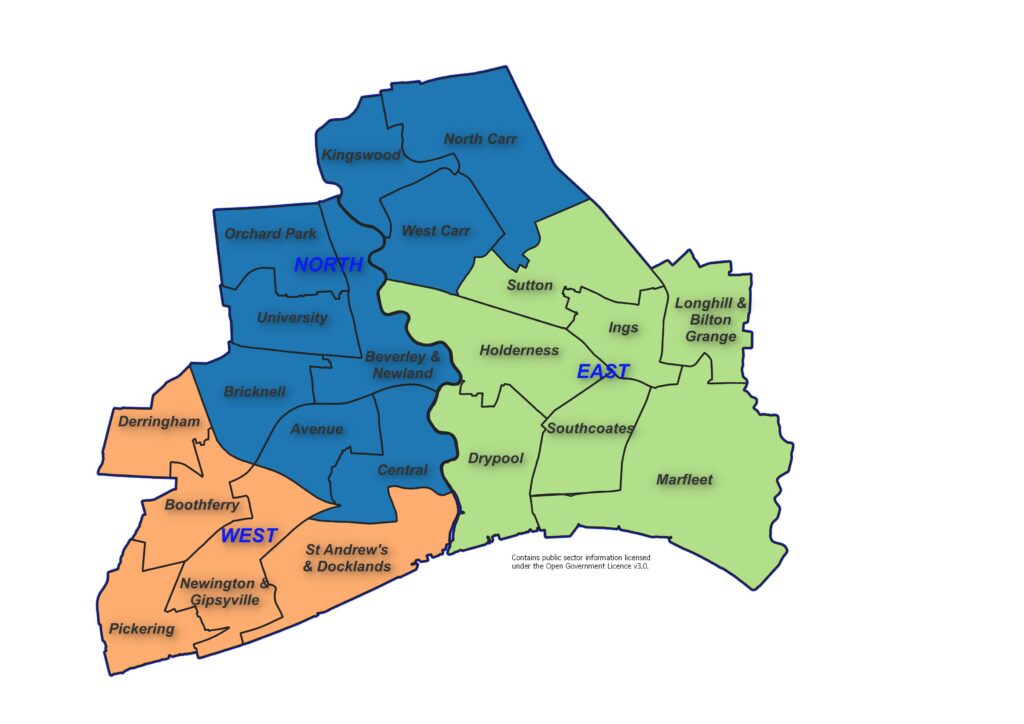
Geographical Boundaries Relating to the NHS
The other key geographical boundary for Hull in terms of health relate to those associated with the NHS. Prior to April 2013, the NHS comprised of Primary Care Trusts (PCTs), and between April 2013 and June 2022, the local NHS geographical area was made up from Clinical Commissioning Groups (CCGs). There were also Sustainability and Transformational Partnerships (STPs) made up of a number of local CCGs. Prior to July 2022, Hull was included within the Humber, Coast and Vale (HCV) STP (which included five other local CCGs: North Yorkshire, Vale of York, East Riding of Yorkshire, North Lincolnshire and North East Lincolnshire). The STPs were later transformed into Health and Care Partnerships (HCPs), and there have been further changes to the NHS geography in July 2022 with Integrated Care Systems.
The Integrated Care System (ICS) is made of up two core statutory elements at system level formerly came into effect on 1 July 2022 when CCGs ceased to exist. The ICSs are where major decisions are made, and overarching strategies agreed. The Integrated Care Boards (ICB) replace CCGs and are focused on the core NHS services, with responsibilities including NHS funding, commissioning and workplace planning. The Integrated Care Partnerships (ICP) have a broad focus, covering ICB-wide strategy, public health, social care, and wider issues impacting the health and wellbeing of the population. There will continue to a Place element within the ICS, and this will involve the planning of localised services and secondary and community care. NHS England sees ‘place’ as the key driver of change within ICSs and they are expected to be where the majority of work actually occurs. Data will continue to available at CCG level for some time and as a result CCG will still be referenced within our Joint Strategic Needs Assessment, and will gradually be replaced over time as the new system is embedded and new data becomes available at the new geographical levels.
The Office for Health Improvement & Disparities’ Fingertips includes some information at sub-ICB level, and Hull is referenced by its CCG code of 03F.
All areas within the Humber and North Yorkshire Integrated Care Board are:
- 02Y – East Riding of Yorkshire
- 03F – Hull
- 03H – North East Lincolnshire
- 03K – North Lincolnshire
- 03Q – Vale of York
- 42D – North Yorkshire
Hull’s Place element is Hull’s Health and Care Partnership, and the Humber, Coast and Vale Health and Care Partnership also ceased to exist and Hull is included in the Humber and North Yorkshire Health and Care Partnership or the Humber and North Yorkshire Integrated Care Board (ICB).
The geographical boundary of the local authority is the same as the boundary for the NHS in Hull, although the population size if different. The resident population is estimated to be 271,942 people in 2023, but the number of patients registered with Hull GPs in January 2024 is 314,119 patients (and around 8% of these patients live in East Riding of Yorkshire). For more information about the difference between the resident population and registered population, see Population Estimates under Population.
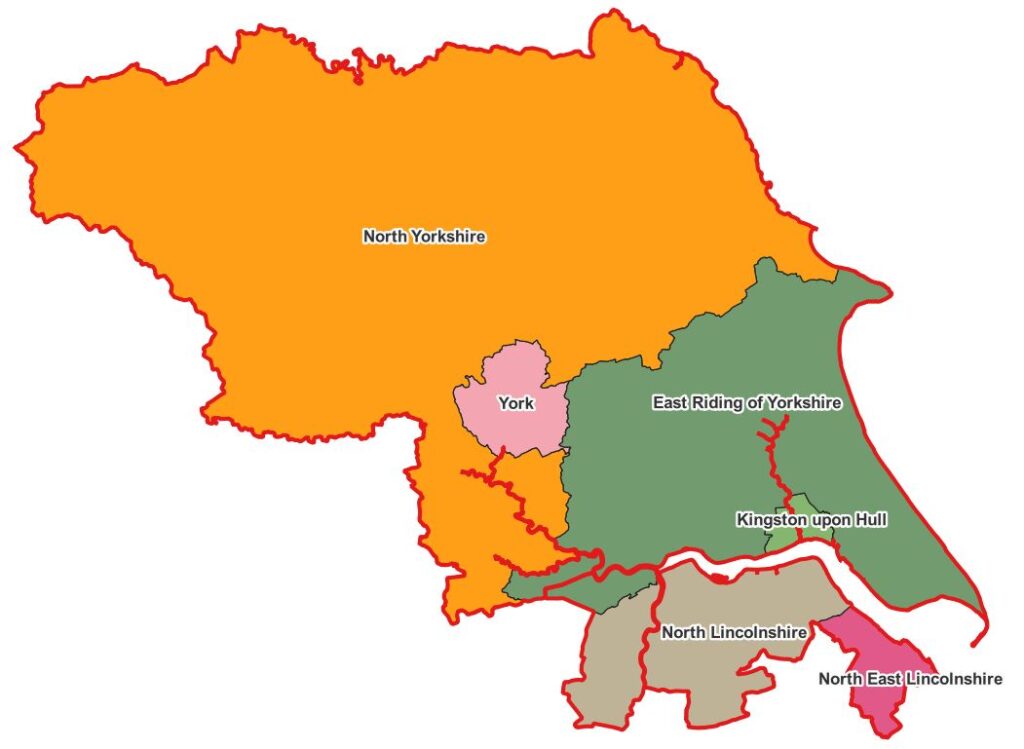
Percentage Visiting Natural Environment For Health or Exercise Purposes
The Office for Health Improvement & Disparities’ Fingertips gives an estimate of the percentage of people who have taken a visit to the natural environment for health or exercise purposes over the previous seven days. The information has not been updated so is quite out-of-date, but nevertheless gives an indication of the utilisation of outdoor space and comparison with other local authorities across the region. Furthermore, these percentages could well have changed both during and after the COVID-19 pandemic.
Compared with benchmark
| Indicator | Period | England | Yorkshire and the Humber region (statistical) | Kingston upon Hull | East Riding of Yorkshire | North East Lincolnshire | North Lincolnshire | York | Barnsley | Doncaster | Rotherham | Sheffield | Bradford | Calderdale | Kirklees | Leeds | Wakefield | North Yorkshire Cty |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Utilisation of outdoor space for exercise or health reasons (Persons 16+ yrs) | Mar 2015 - Feb 2016 | 17.9 | 17.5 | 18.0 | 16.8 | 22.0 | 6.4 | 20.9 | 14.5 | 19.3 | 13.5 | 15.3 | 12.4 | 20.4 | 17.6 | 20.5 | 16.6 | 17.8 |
| Indicator | Period | England | Yorkshire and the Humber region (statistical) | Kingston upon Hull | East Riding of Yorkshire | North East Lincolnshire | North Lincolnshire | York | Barnsley | Doncaster | Rotherham | Sheffield | Bradford | Calderdale | Kirklees | Leeds | Wakefield | North Yorkshire Cty |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Utilisation of outdoor space for exercise or health reasons (Persons 16+ yrs) | Mar 2015 - Feb 2016 | 17.9 | 17.5 | 18.0 | 16.8 | 22.0 | 6.4 | 20.9 | 14.5 | 19.3 | 13.5 | 15.3 | 12.4 | 20.4 | 17.6 | 20.5 | 16.6 | 17.8 |
Fingertips also provides information on the trends over time relating to this indicator prior to this indicator finishing in 2016. The percentages in Hull were lower than England for the four periods 2011-12 to 2014-15 but in the last reporting period of 2015-16, the percentage in Hull was slightly higher than England.
Compared with benchmark
Utilisation of outdoor space for exercise or health reasons (Persons 16+ yrs)
|
Period
|
Kingston upon Hull |
Yorkshire and the Humber region (statistical)
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| Mar 2011 - Feb 2012 | • | - | 11.7% | 8.1% | 15.2% | 15.2% | 14.0% |
| Mar 2012 - Feb 2013 | • | - | 11.0% | 7.5% | 14.6% | 16.5% | 15.3% |
| Mar 2013 - Feb 2014 | • | - | 13.0% | 9.5% | 16.4% | 18.3% | 17.1% |
| Mar 2014 - Feb 2015 | • | - | 14.3% | 10.8% | 17.8% | 19.4% | 17.9% |
| Mar 2015 - Feb 2016 | • | - | 18.0% | 14.0% | 22.0% | 17.5% | 17.9% |
Source: Office for Health Improvement and Disparities
Environmental Factors
Access to Healthy Assets and Hazards Index
The Access to Healthy Assets and Hazards (AHAH) index is designed to allow policy and decision makers to understand which areas have poor environments for health, and to help move away from treating features of the environment in isolation.
The Access to Healthy Assets and Hazards index is comprised of four domains: access to retail services (fast food outlets, gambling outlets, pubs/bars/nightclubs, off licences, tobacconists), access to health services (GP surgeries, A&E hospitals, pharmacies, dentists and leisure centres), the physical environment (green and blue spaces) and levels of air pollution (nitrogen dioxide (NO2), particulate matter smaller than 10 microns (PM10) and sulphur dioxide (SO2)). The Access to Healthy Assets and Hazards index provides a summary of an area’s relative performance on these indicators (the second and third domains conceptualised as health promoting and the first (access to retail) as health demoting. It therefore provides information on how conducive to good health an area is relative to other areas, for the specific indicators.
Public Health England’s (now the Office for Health Improvement & Disparities) Spatial Planning for Health document states that an ‘ever-increasing body of research indicates that the environment in which we live is inextricably linked to our health across the life course. For example, the design of our neighbourhoods can influence physical activity levels, travel patterns, social connectivity, mental and physical health and wellbeing outcomes.’ The indicator is intended to support interventions to improve the health promoting qualities of the environment, and is primarily aimed at those working in public health roles in local authorities.
The Access to Healthy Assets and Hazards index is constructed given equal weight to the different measures and domains. It is therefore designed as a balanced description of an area with regard to these domains, and not as a summary of the health impacts on the population.
Overall Index
The Access to Healthy Assets and Hazards index is originally produced at lower layer super output area geographical level as an average of values for constituent postcodes but has been presented at local authority level in the Office for Health Improvement & Disparities’ Fingertips.
The Access to Healthy Assets and Hazards index is presented as percentage of the total population residing in lower super output areas defined as in the bottom 20% of all areas on the Access to Healthy Assets and Hazards Index as a percentage of the total population of the area.
In 2024, the Access to Healthy Assets and Hazards Index is very high in Hull with 44.7% of Hull’s population residing in the bottom fifth of areas nationally in relation to the Access to Healthy Assets and Hazards Index. The percentage nationally is 20.9% and across the other 14 lower tier local authorities in the region the range is from 1.3% to 32.6%.
In London, 23 of the 33 upper-tier local authorities have a higher percentage of their populations living within areas in the bottom fifth of areas nationally in relation to the Access to Healthy Assets and Hazards Index due to the high population density of many London local authorities. This includes 11 London upper-tier local authorities where three-quarters or more of their populations are living within areas in the bottom fifth of areas nationally in relation to the Access to Healthy Assets and Hazards Index including the City of London where all its population fall into this category. Outside London, Hull has the fifth highest percentage among the 120 upper-tier local authorities outside London being lower than Thurrock (74%), Liverpool (53%), Leicester (47%) and Oldham (45%).
Compared with benchmark
| Indicator | Period | England | Yorkshire and the Humber region (statistical) | Kingston upon Hull | East Riding of Yorkshire | North East Lincolnshire | North Lincolnshire | York | North Yorkshire UA | Barnsley | Doncaster | Rotherham | Sheffield | Bradford | Calderdale | Kirklees | Leeds | Wakefield |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Access to Healthy Assets & Hazards Index (Persons All ages) | 2024 | 20.9 | 18.2 | 44.7 | 9.4 | 23.6 | 10.7 | 1.3 | 13.4 | 10.2 | 6.2 | 9.7 | 13.7 | 32.6 | 5.1 | 13.1 | 30.3 | 18.8 |
| Indicator | Period | England | Yorkshire and the Humber region (statistical) | Kingston upon Hull | East Riding of Yorkshire | North East Lincolnshire | North Lincolnshire | York | North Yorkshire UA | Barnsley | Doncaster | Rotherham | Sheffield | Bradford | Calderdale | Kirklees | Leeds | Wakefield |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Access to Healthy Assets & Hazards Index (Persons All ages) | 2024 | 20.9 | 18.2 | 44.7 | 9.4 | 23.6 | 10.7 | 1.3 | 13.4 | 10.2 | 6.2 | 9.7 | 13.7 | 32.6 | 5.1 | 13.1 | 30.3 | 18.8 |
Despite the very high levels in Hull, the index has decreased considerably since 2016 when nine in ten residents lived in the worst fifth of areas of England in relation to the index, although there was a large decrease between 2016 and 2017 to 46% with only relatively minor changes to 2022 and 2023.
In 2024, it is estimated that 120,220 residents in Hull live within areas defined as the bottom fifth of areas nationally based on the Access to Healthy Assets and Hazards Index.
Compared with benchmark
Access to Healthy Assets & Hazards Index (Persons All ages)
|
Period
|
Kingston upon Hull |
Yorkshire and the Humber region (statistical)
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2016 | • | 233157 | 90.0% | - | - | 22.2% | 21.2% |
| 2017 | • | 120814 | 46.3% | - | - | 14.1% | 21.1% |
| 2022 | • | 114694 | 44.3% | - | - | 19.9% | 22.6% |
| 2024 | • | 120220 | 44.7% | - | - | 18.2% | 20.9% |
Source: Consumer Data Research Centre
Information relating to version 4 of the Access to Healthy Assets and Hazards index is available at lower layer super output area geographical level. There are 33,755 lower layer super output areas in England, and the percentile score has been calculated for each of the 168 lower layer super output areas in Hull. The index was updated in July 2024. The air pollution data is from the Department for Environment, Farming and Rural Affairs (DEFRA) for 2022. Locations of health facilities data is available quarterly so the data will relate to data from 2024, and retail facilities location data and the blue and green space indicators relate to data within the last year or so.
As Hull is a city and a relatively densely populated city with tight boundaries, it does mean that there is not far to travel with regard to access to healthcare in that that most of the population are as short drive away from the nearest dentist, GP, hospital and pharmacy. This results in Hull having a relatively good score in relation to to the health index. However, this also means that drive times are low to ‘unhealthy’ places such as fast food outlets, gambling outlets, pubs/bars/nightclubs, off licences and tobacconists. Areas with more dense areas of industry and cities with more roads will also tend to have higher levels of pollution than more rural areas. Hull tends to have a relatively high number of green spaces (as mentioned above around one-third of Hull is green space) and with the proximity of the Humber estuary and the River Hull, there is also only a short drive to the nearest blue space in Hull.
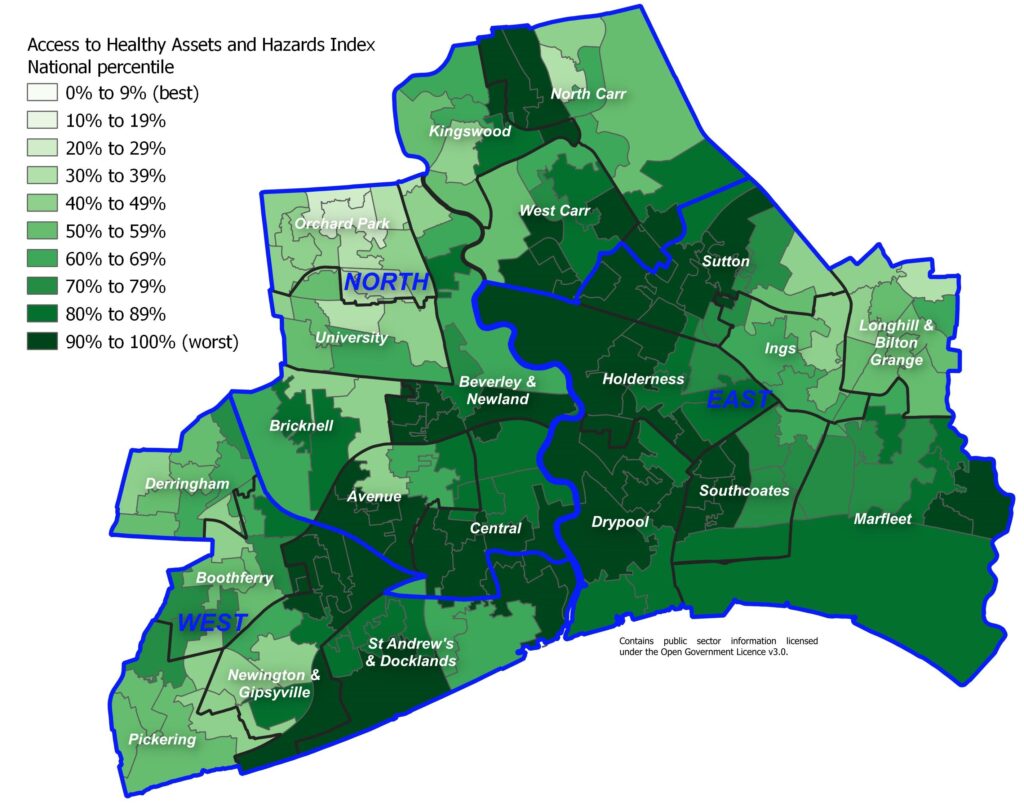
Usefulness and Problems Associated with the Index
It is useful to examine the index as a whole, but with the caveats associated with some of the individual components of the index, it is also useful to examine the individual components to assess potential issues or hazards for people living in the different areas of the city. The individual components of the index are mapped below.
Whilst the index is useful to examine the distribution of assets and hazards, it is also imperative that local knowledge is used to assess individuals components of the index and to recognise that the index does not portray the full picture with regards to healthy assets and hazards for the following reasons:
- Many of the indicators are based on drive times with an inherent assumption that residents have access to a car or van. In a city with good transport networks and problems with parking, car ownership tends to be lower than more rural areas and car ownership is lower in more deprived areas of the city as well as areas closer to the city centre. From the 2021 Census, 35% of household had no cars or vans in the household compared to 23% for England. If people need to rely on public transport, cycling or walking then it is likely that travel times are longer. This is particularly the case if it is necessary to catch more than one bus and also there could be cost implications too. In many cases, from anecdotal evidence, people in Hull are less likely to travel to services if they need to catch more than one bus, and some of the more deprived areas of Hull do not have direct services into the city centre.
- Drive times to the nearest dentist does not reflect any access, and it is likely that most dental surgeries are not accepting new NHS clients so access to dental services in Hull is difficult particularly for people living in deprived areas who are less able to pay for private dental services.
- Drive times to the nearest blue space and the ‘greenness’ of the immediate area does not reflect quality of that space or accessibility. As Hull is on the Humber estuary and has the River Hull running through the city, most areas in Hull have low drive times to the nearest blue space, but the banks of the Humber estuary and River Hull are not necessarily places where most people would want to spend much leisure time. Green space is measured by satellites as the average Normalised Difference Vegetation Index as close to summer equinox as possible. The Normalised Difference Vegetation Index takes a value from zero (no vegetation or dead vegetation) to one (very healthy vegetation) and the measure of green space in the Access to Healthy Assets and Hazards index uses the average Normalised Difference Vegetation Index for an 80 metre radius around the postcode centroid for each postcode (the rational is that the average extent of a postcode in the UK is around 160 metres by 160 metres). Therefore, it is essentially measuring the ‘greenness’ of an area. This does not necessarily equate to assess and quality of that space. Other people’s gardens would be included in the green space measure. Furthermore, even if the green space is a public space, other factors may influence its use such as feelings of safety (and feelings of safety do differ by deprivation in Hull).
- Drive times to other facilities such as those related to healthcare or leisure facilities do also not take into other factors related to access such as cost, quality or waiting times, etc.
- The measure will not include informal networks in relation to illegal products such as tobacco or alcohol. The majority of alcohol is purchased in off-licences, shops and supermarkets which are not taken into account as the nearest pub, bar or nightclub is included in the index.
- Access to fresh fruit and vegetables are very important in relation to having a healthy lifestyle and there are many areas in Hull where there is a lack of such access which include some of the more deprived areas such as Orchard Park.
Some of the indicators counter each other in that Hull’s tight boundaries mean that there is a relatively high concentration of health-related and ‘unhealthy’ retail facilities so these domains balance each other out. The same is true for blue and green space as areas of the city close to the River Hull have less green space. This is another reason why it is useful to examine the indicators and domains separately.
Health Domain
As mentioned above, drive times do not fully capture access to high quality healthcare as quality, waiting times, access and lack of a car or van is not taken into account. This will particularly be the case for access to dentistry due to the lack of NHS dentists and the potentially prohibitive cost of private dentistry in the most poorest areas of the city. Nevertheless, the maps will show areas of Hull that are more accessible in terms of drive times to the nearest dentists, GPs, hospital and pharmacy.
The following map illustrates the distance from the nearest dentist in terms of driving time. All residents live within a six minute drive of their nearest dental surgery, but this does not necessarily mean that they have access to dental care particularly NHS dental care.
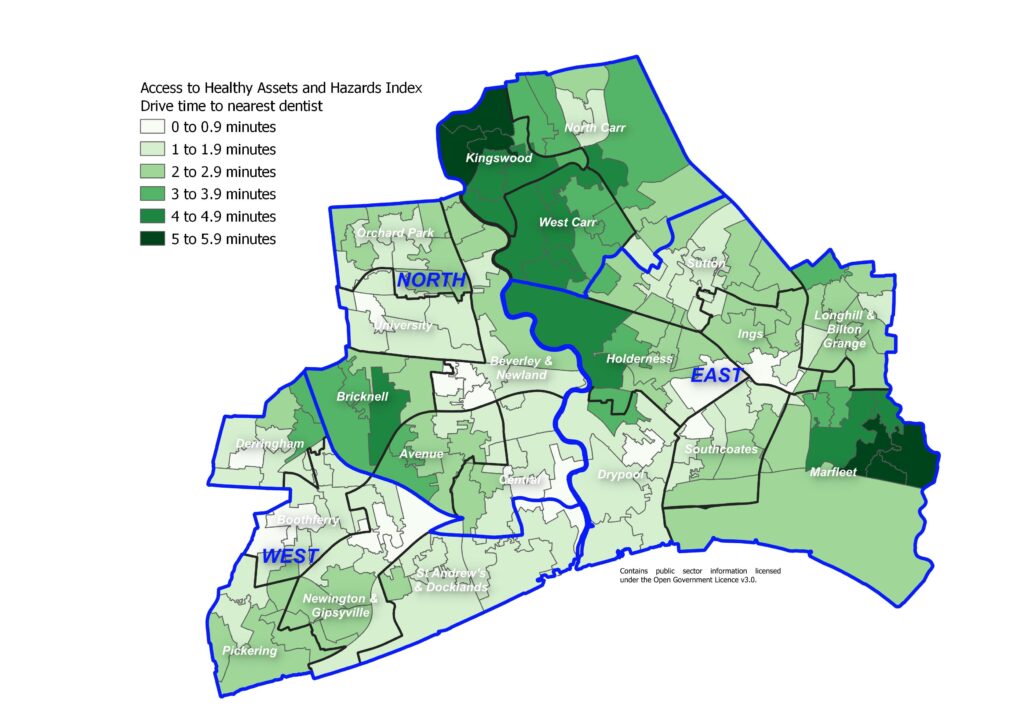
The following map illustrates the distance from the nearest GP in terms of driving time. All residents live within a five minute drive of their nearest GP surgery
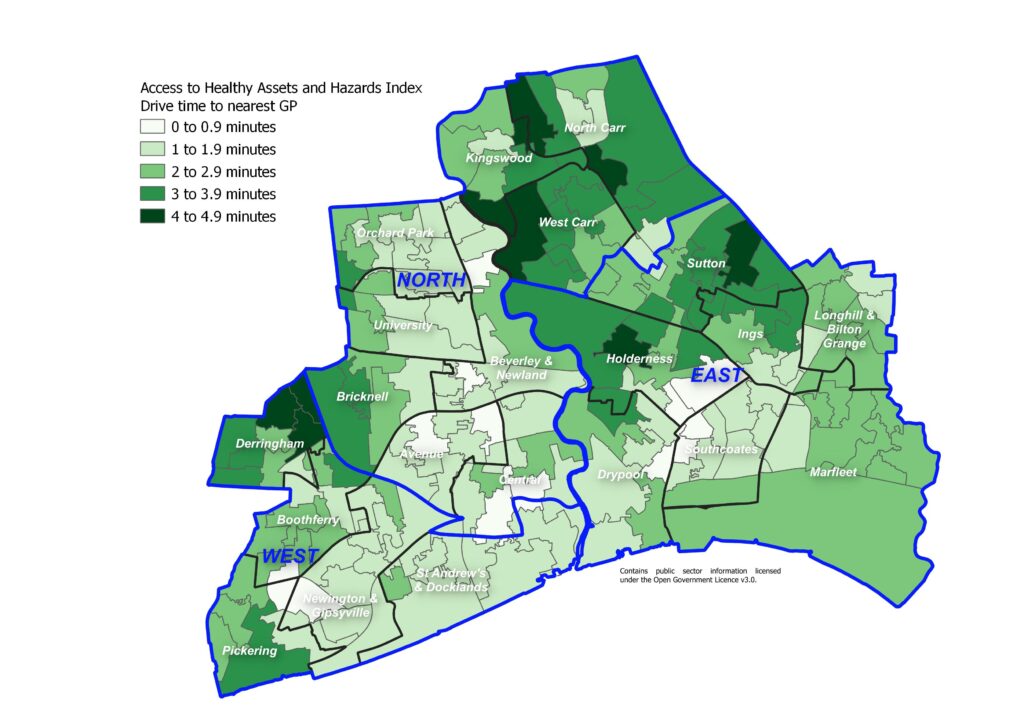
The following map illustrates the distance from the nearest hospital in terms of driving time. All residents live within a five minute drive of their nearest hospital.
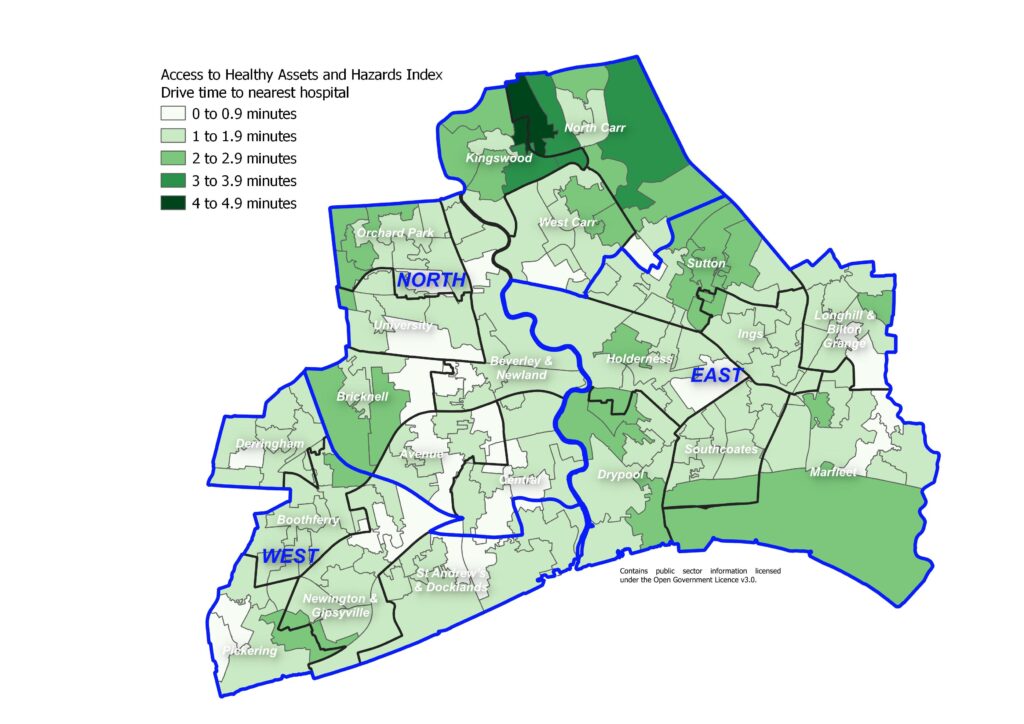
The following map illustrates the distance from the nearest pharmacy in terms of driving time. All residents live within a five minute drive of their nearest pharmacy.
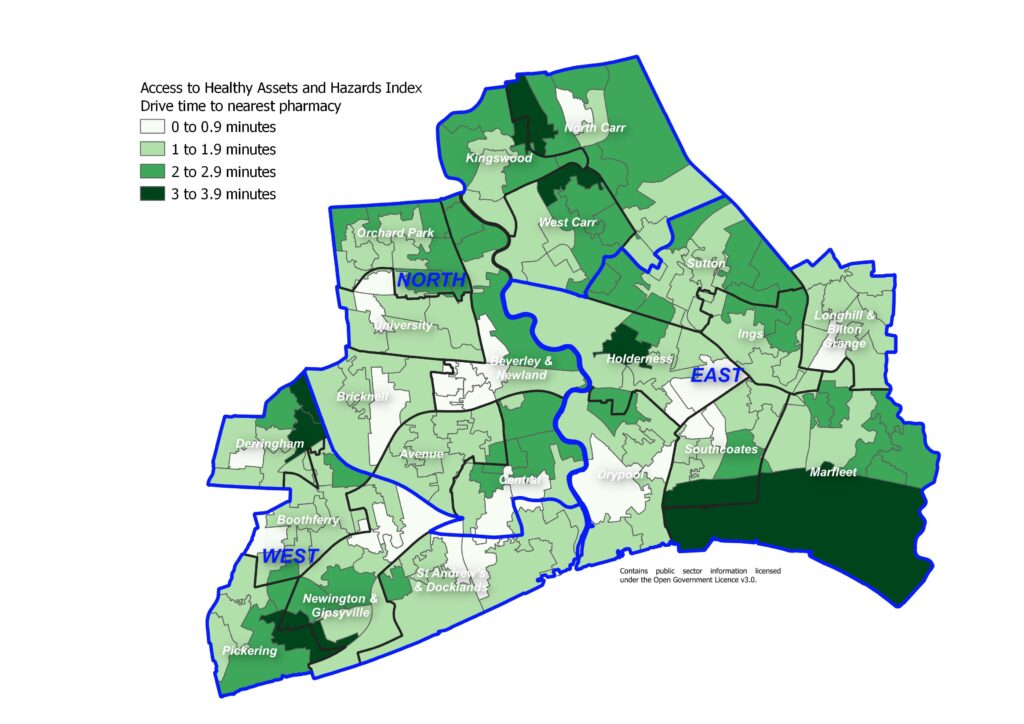
With Hull being a compact city with low drive times to health facilities, the majority of areas of Hull perform well in relation to the other geographical areas across the country particularly areas of Hull around the city centre, up Beverley Road (on the boundary splitting Avenue and Central wards, and splitting University and Orchard Park wards from Beverley & Newland) along Holderness Road (on the boundary splitting Southcoates from Holderness), along Anlaby Road where the hospital lies (splitting the southern boundary of Central from St Andrew’s & Docklands), along Cottingham Road (splitting University and Bricknell wards) and Spring Bank West (which runs from Central through parts of Avenue towards Boothferry). Areas to the north and east of the city such as Kingswood, North Carr, West Carr, Holderness, Sutton and Marfleet tend to have higher drive times to health facilities compared to other areas of Hull. The percentile scores range from 2 to 83 so none of Hull’s 168 lower layer super output areas are the the worst 10% nationally in terms of drive times to health facilities.
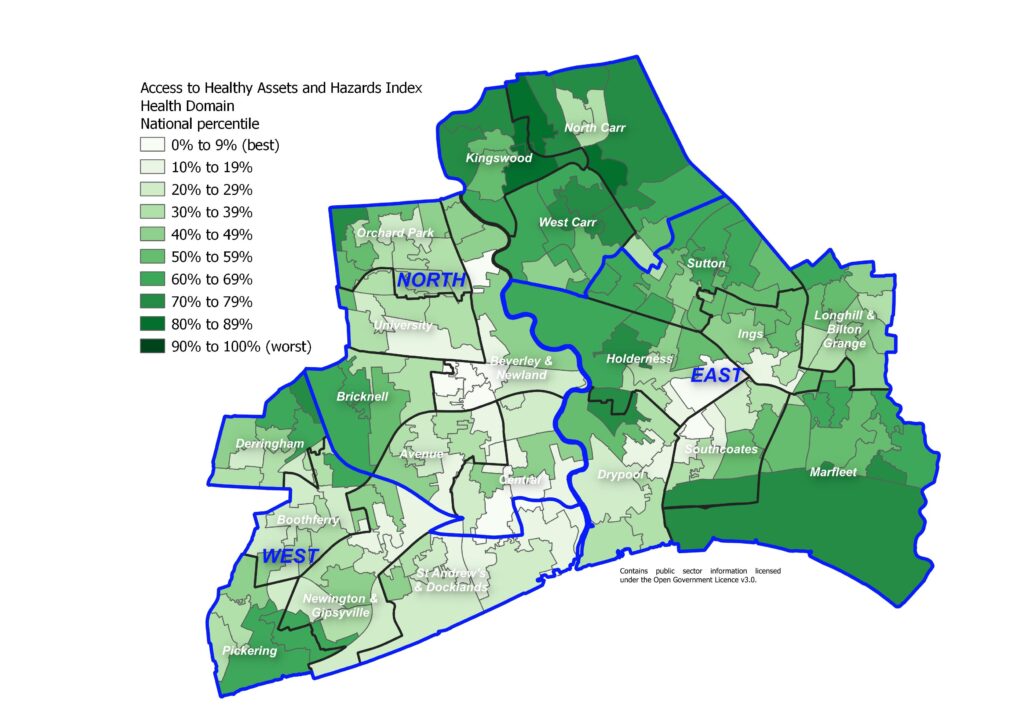
Retail Environment
The following map illustrates the distance from the nearest fast food outlet in terms of driving time. It can be seen that the majority of Hull residents live in an area where it is only a couple of minutes drive from the nearest fast food outlet, and all areas of Hull are within a five minute drive of fast food.
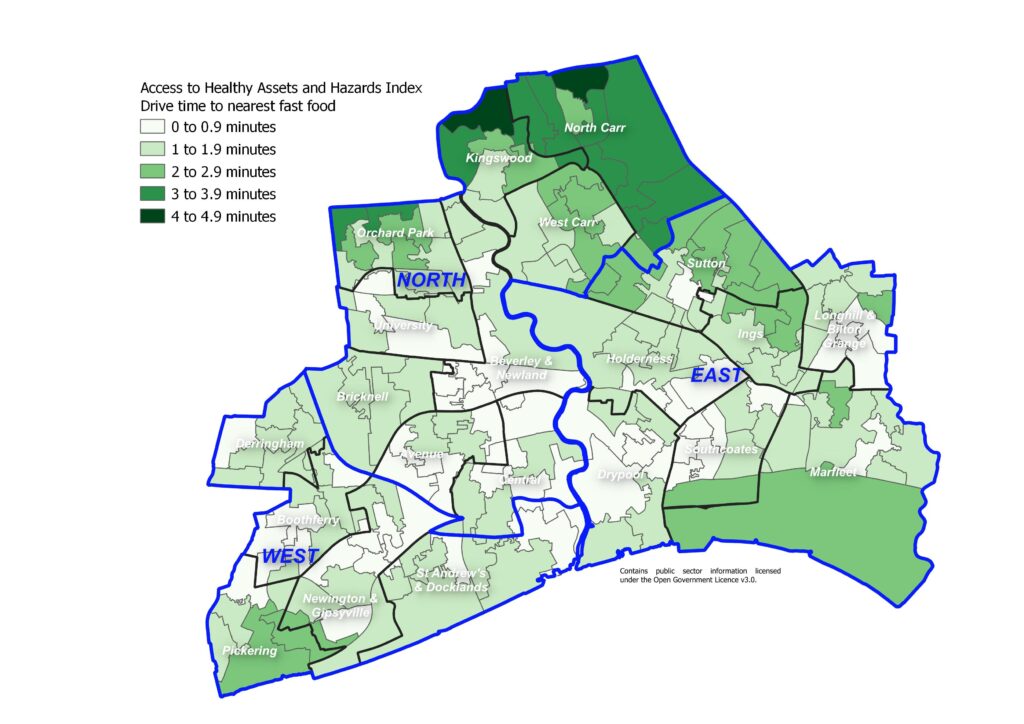
Information relating to the density of fast food outlets can also be found under Diet and Nutrition Among Adults under Lifestyle Factors under Adults.
The following map illustrates the distance from the nearest pub, bar or nightclub in terms of driving time. The majority of residents of Hull live within a five minute drive of the nearest pub, bar or nightclub with only some areas to the north of the city in Kingswood and North Carr having a slightly longer drive time, although all residents live within an eight minute drive of the nearest pub, bar or nightclub.
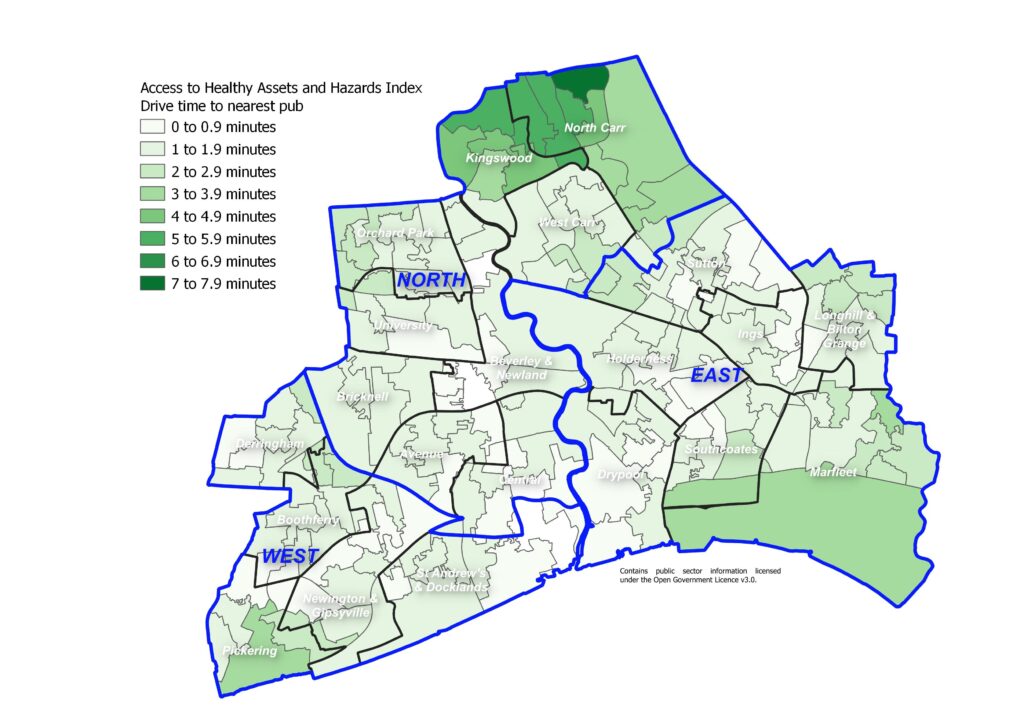
The following map illustrates the distance from the nearest gambling outlet in terms of driving time. The majority of residents of Hull live within a five minute drive of the nearest gambling outlet with only some areas to the north of the city in Kingswood and North Carr having a slightly longer drive time, although all residents live within an eight minute drive of the nearest gambling outlet.
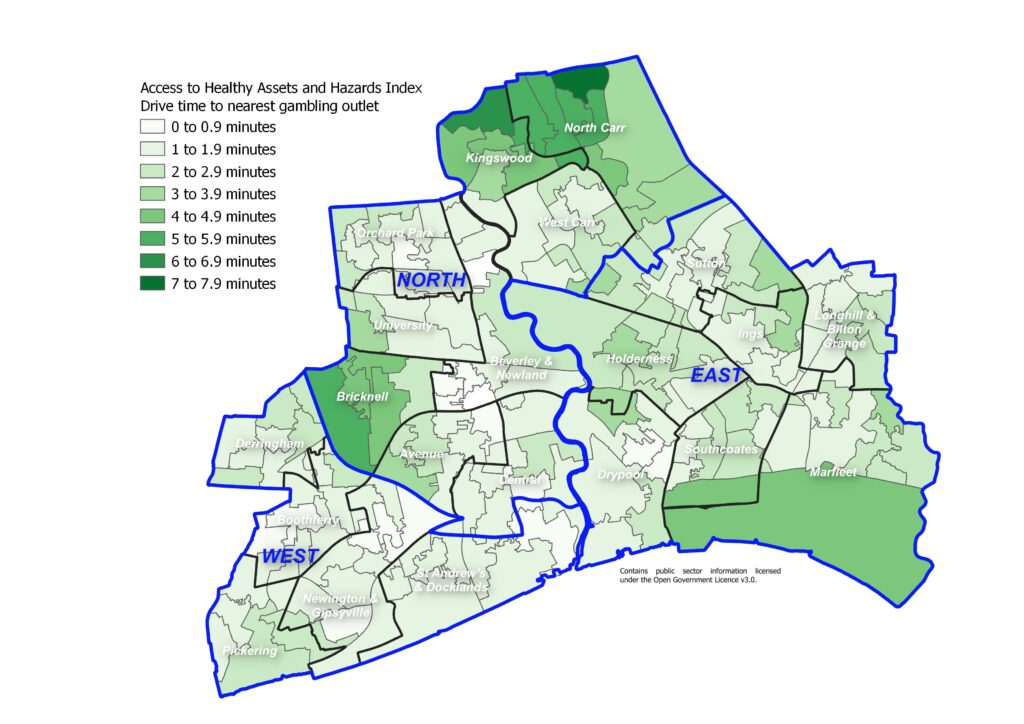
The following map illustrates the distance from the nearest tobacconist or vape store in terms of driving time. As with pubs, bars and nightclubs and with gambling outlets, the majority of residents of Hull live within a short minute drive of the nearest tobacconist or vape store with only some areas to the north of the city in Kingswood and North Carr having a slightly longer drive time, although all residents live within an an 11 minute drive of the nearest tobacconist or vape store.
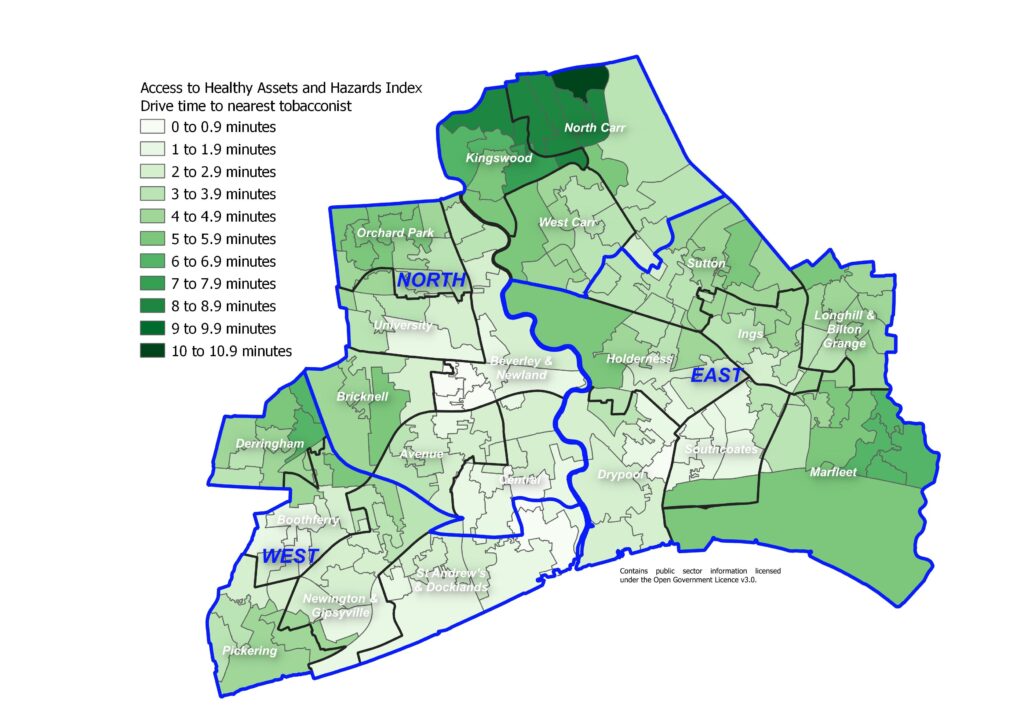
The following map illustrates the distance from the nearest leisure centre in terms of driving time. The majority of residents living around the city centre, to the south west of the city, and around the University are only a few minutes drive from the nearest leisure centre. Residents living on the north, north west and east boundaries of Hull have a slightly longer drive time, although all residents are within a nine minute drive of the nearest leisure centre.
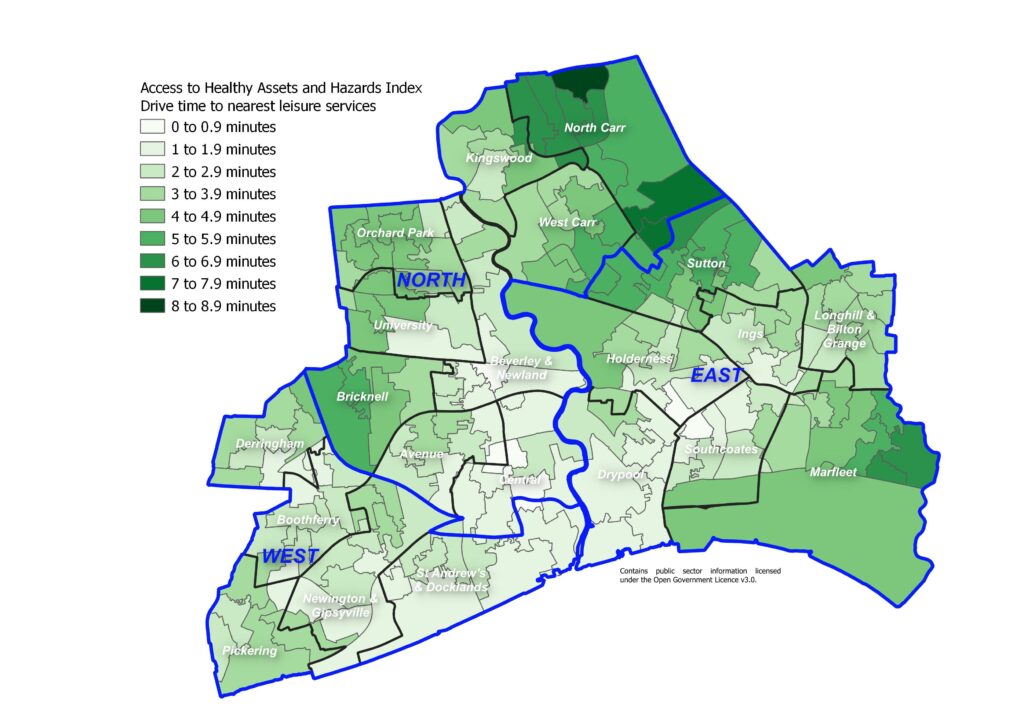
With Hull being a compact city with low drive times to retail facilities, the majority of areas of Hull perform poorly in relation to the other geographical areas across the country with relatively low drive times to fast food outlets, pubs, tobacconists and gambling outlets). The worst areas in Hull tend to be similar areas to those which performed well on the health domain as they are areas close to main roads with a relatively high number of retail and health units. These areas include areas around the city centre, up Beverley Road, along Holderness Road, along Anlaby Road (all the way along from Central ward to Hull’s boundary in Boothferry, along Hessle Road (in St Andrew’s & Docklands and Newington & Gipsyville wards), along Cottingham Road and along part of Sutton Road (within Beverley & Newland ward linking West Carr and Orchard Park wards). Areas to the north and east of the city such as Kingswood, North Carr, West Carr, Holderness, Sutton and Marfleet tend to have higher drive times to health facilities compared to other areas of Hull. The percentile scores range from 13 to 100 so none of Hull’s 168 lower layer super output areas are the the best 10% nationally in terms of drive times to retail facilities. Seven in ten of Hull’s lower layer super output areas are in the worst 50% of areas of England in terms of short distances from fast food outlets, pubs, tobacconists and gambling outlets. Areas in Kingswood and North Carr in particular are among the best areas in terms of the retail domain.
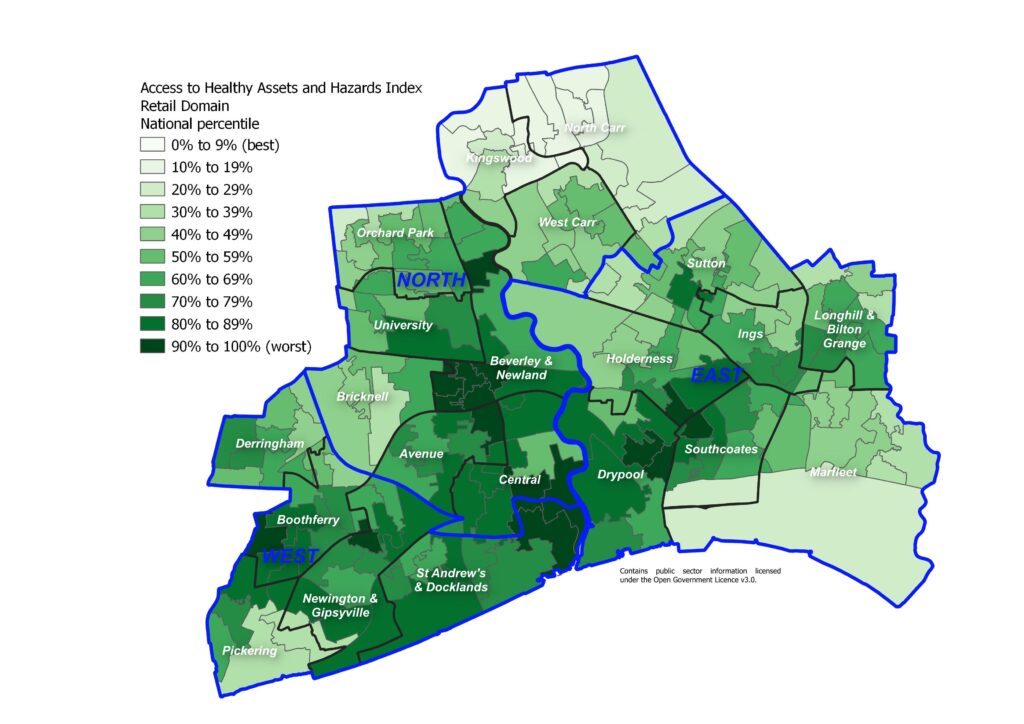
Access to Blue and Green Space
As mentioned above, drive times do not fully capture access to good quality, safe blue and green space where residents want to spend their time for health-related reasons.
The following map illustrates the distance from nearest blue space in terms of driving time.
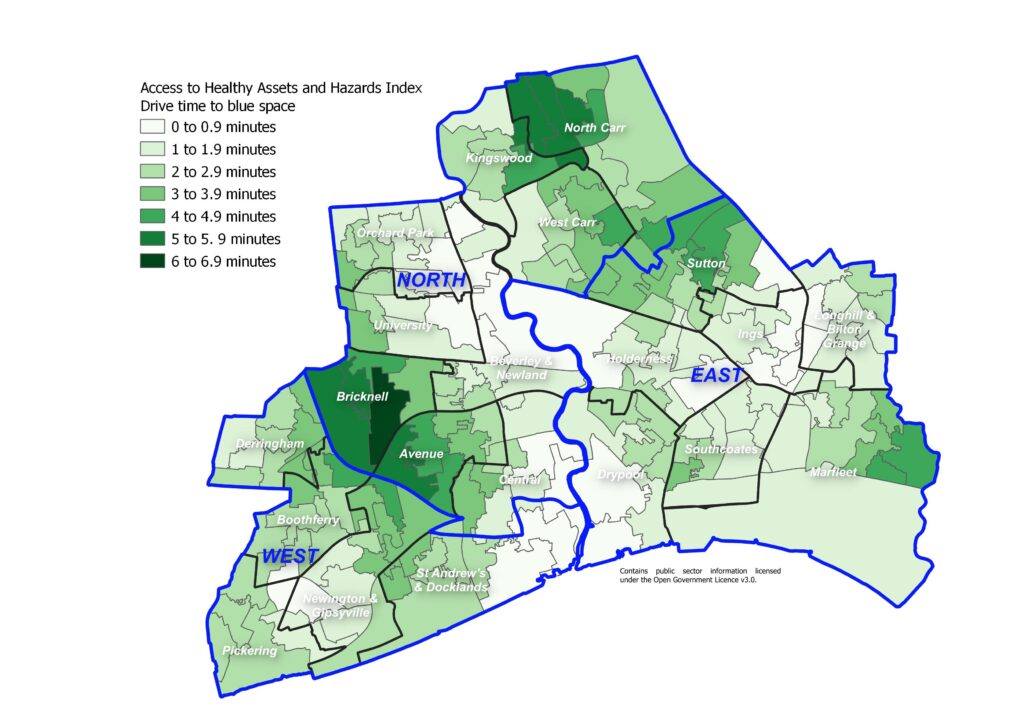
As mentioned above, green space is measured by satellites as the average Normalised Difference Vegetation Index as close to summer equinox as possible. The Normalised Difference Vegetation Index takes a value from zero (no vegetation or dead vegetation) to one (very healthy vegetation) and the measure of green space in the Access to Healthy Assets and Hazards index uses the average Normalised Difference Vegetation Index for an 80 metre radius around the postcode centroid for each postcode (the rational is that the average extent of a postcode in the UK is around 160 metres by 160 metres). Therefore, it is essentially measuring the ‘greenness’ of an area. This does not necessarily equate to assess and quality of that space. Other people’s gardens would be included in the green space measure. Furthermore, even if the green space is a public space, other factors may influence its use such as feelings of safety (and feelings of safety do differ by deprivation in Hull).
It can be seen that there is less green space in the more industrial areas of the city (an inverted T-shape along the south boundary following the A63 and from south to north following the route of the River Hull up the middle of the city).
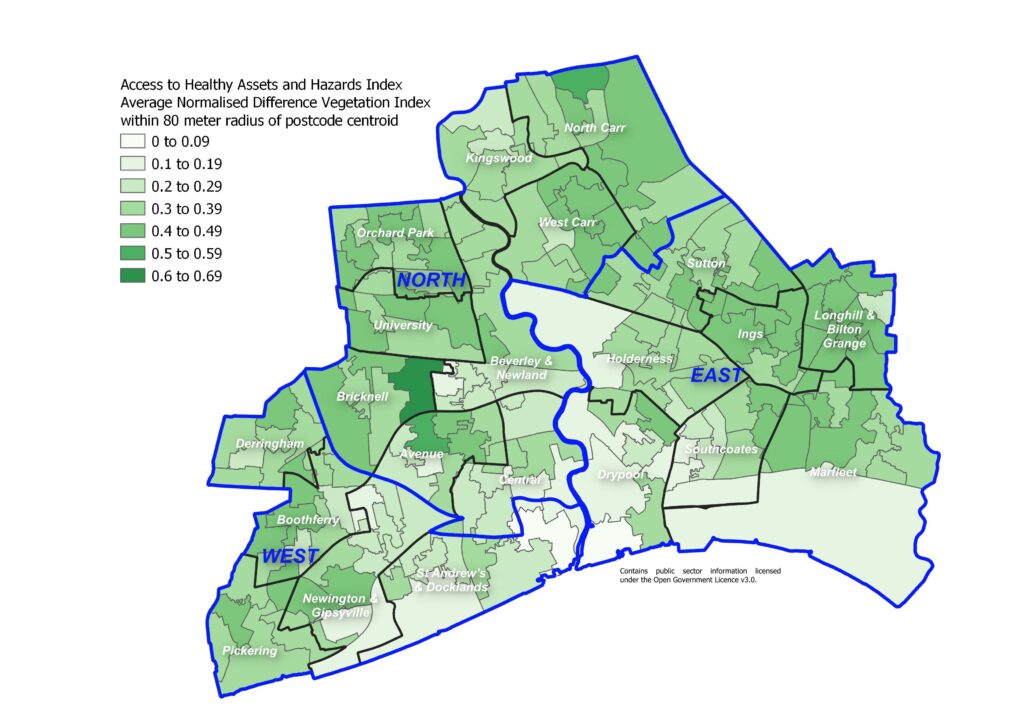
Given that drive times to the nearest blue and green space in Hull is relatively low, it is perhaps a surprise that Hull has such a range of areas from best to worst in terms of drive time to blue space and green space nearby with the percentile scores ranging from 3 to 99 in Hull. However, to an extent the blue and greens spaces counterbalance each other. The more industrial areas of Hull generally tend to be close to blue space, but tend to have the lowest scores for ‘greenness’. So this might be a factor in explaining the range in Hull.
Areas around the west from Bricknell in the north to St Andrew’s & Docklands and Newington & Gipsyville in the south, areas near Drypool and Southcoates, and areas near Kingswood and North Carr tend to be the worst areas in Hull in terms of access to blue and green space.
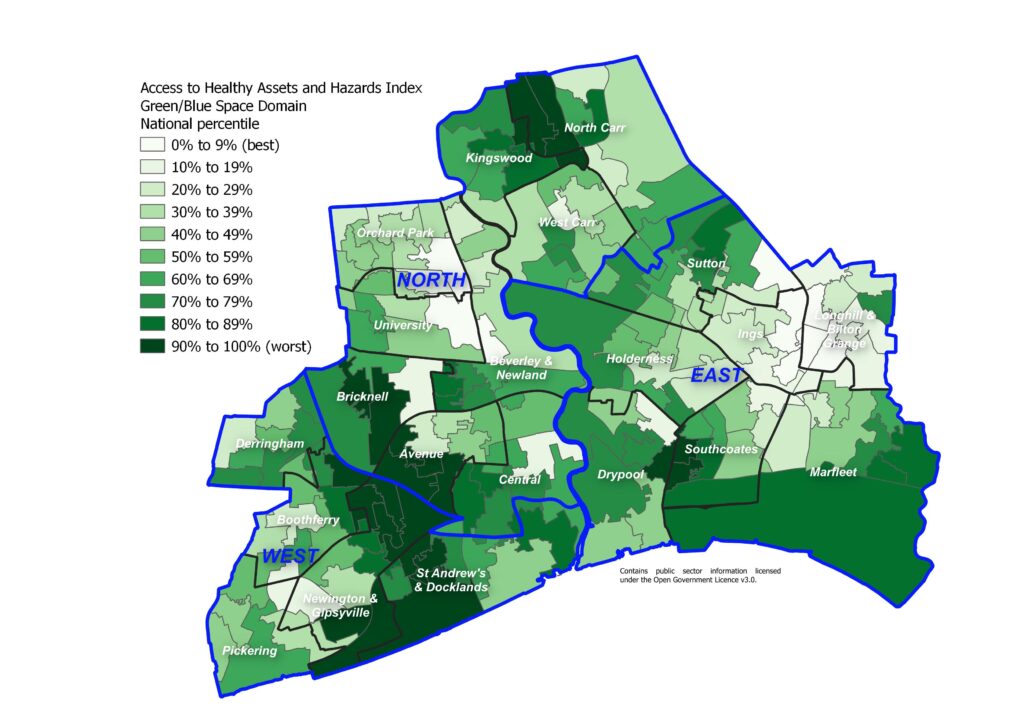
Air Pollution
The following map illustrates the average annual levels of nitrogen dioxide. Levels of air pollution tend to be higher along main arterial travel routes and in areas with higher levels of industry and this is the case for Hull. Furthermore, as the prevailing wind in the UK is predominantly from the south-west, this generally means that air pollution levels tend to be higher in easterly areas.
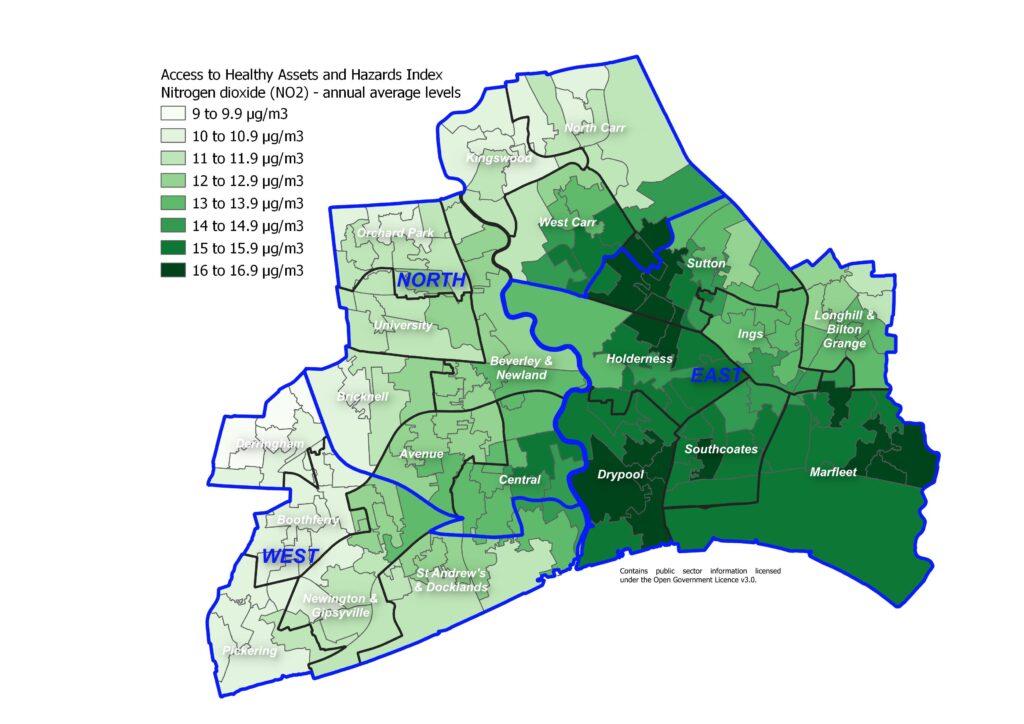
The following map illustrates the average annual levels of sulphur dioxide. There appears to be two pockets of areas with relatively high levels of sulphur dioxide in Hull and areas further away from these two areas tending to have the lowest levels compared to the Hull average.
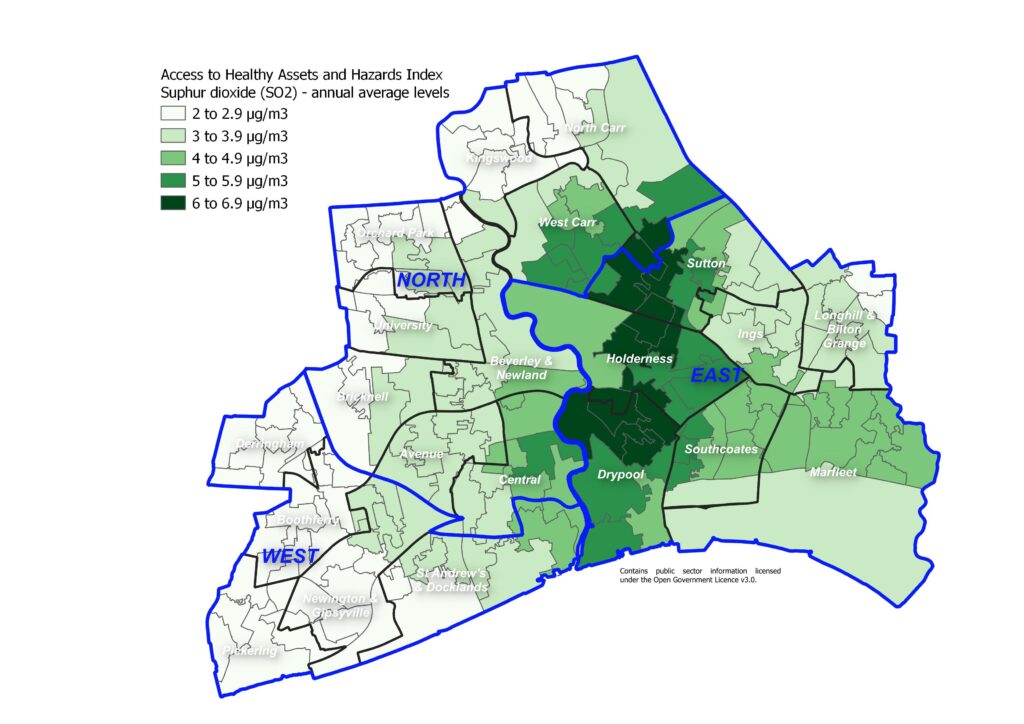
The following map illustrates the average annual levels of particulate matter with size less than 10 microns.
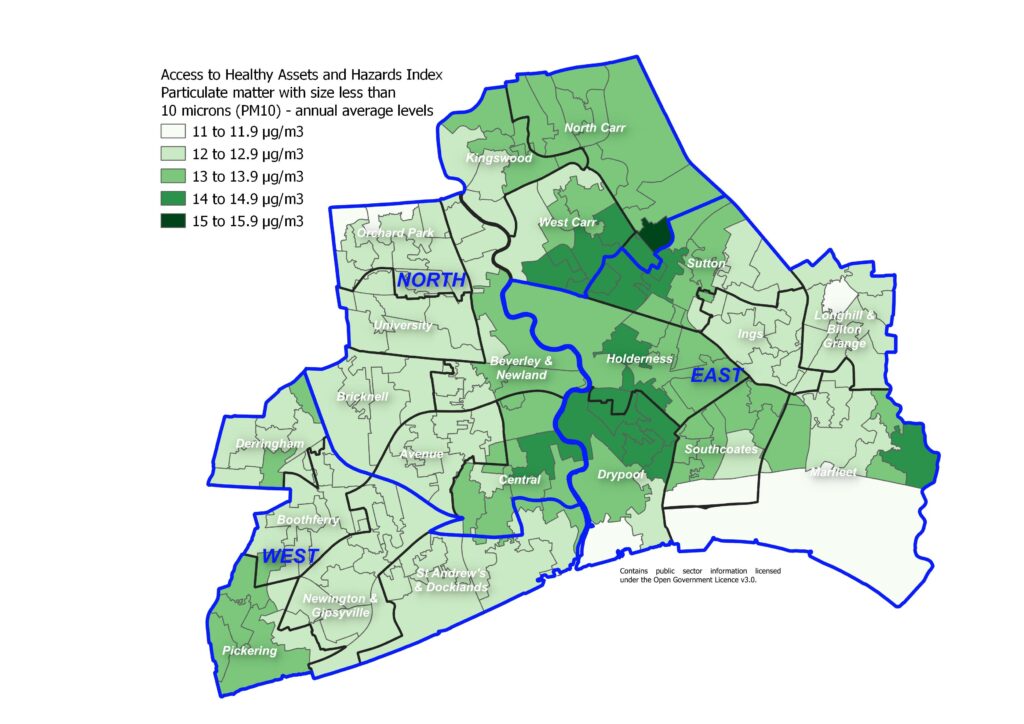
The levels of air pollution in terms of average annual levels of nitrogen dioxide, sulphur dioxide and particulate matter with size less than 10 microns are high relative to other areas of England. This is not particularly surprising as most cities with relatively high density of roads and industry compared to rural areas will tend to have relatively high levels of air pollution. Not surprisingly, the areas with the highest levels of pollution are those with the higher levels of industry and in the east where the prevailing wind will tend to increase levels of air pollution.
The percentile scores range from 68 to 100 so none of Hull’s 168 lower layer super output areas are the the best 60% nationally in terms of air pollution levels. Four in ten of Hull’s lower layer super output areas are in the worst 10% of areas of England in terms air pollution levels, and almost seven in ten of the areas are in the worst 20% nationally. All but two of Hull’s 168 lower layer super output areas are in the worst 30% of areas nationally in terms of air pollution.
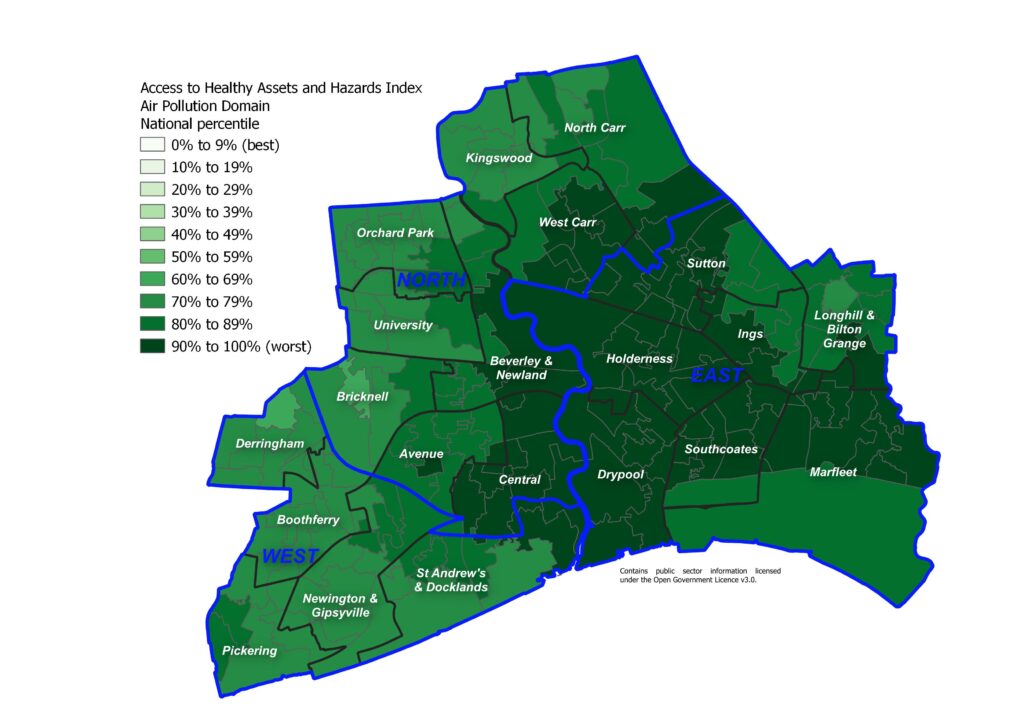
Further information on the environmental factors of Air Pollution and Climate Change can be found within Health and Wellbeing Influences.
Strategic Need and Service Provision
Most of the above factors in terms of physical and organisational boundaries are fixed and not amenable to change. However in the absence of altered local authority boundaries, they reinforce the need for close and collaborative working with local geographic partners, particularly in the East Riding of Yorkshire, and areas included within the the Humber and North Yorkshire Health and Care Partnership. The upside of Hull’s tight boundaries is that access to central services in Hull City Centre is relatively good for the majority of the public, with good transport links radiating to and from the City Centre. Links such as bus routes are often less good between communities “around the edge” of Hull, which may be physically near to one another but not have easy access.
The aim of the Humber and North Yorkshire Health and Care Partnership is to work together to help everyone have the best start in life, live well and grow older well. Making sure that every child has the best start in life, making sure that everyone can access the right care and support when their health changes, supporting people to be independent and in control as they get older, and making sure that people can talk about what they want to happen when when they die. Their priorities are as follows:
- Helping people to look after themselves and stay well;
- Making sure services are joined across health and care;
- Making sure we have the right care in certain areas; and
- Making sure we are using our resources well.
The Humber and North Yorkshire Health and Care Partnership’s approach may be different across the different geographical areas depending on the characteristics within each area.
There has been significant recent investment in Hull
revealed within Hull’s City Plan both before, during and after the City of
Culture year of 2017.
The ambitions of the Hull’s City Plan are to make Hull the leading hub for renewable energy industries (UK Energy City), make Hull a world-class visitor destination (Destination Hull) by capitalising on Hull’s role as UK City of Culture 2017, the multi-million pound investment into the city’s cultural and tourism infrastructure, and making Hull a place of opportunity for all, building strong and resilient communities by focusing on safeguarding the most vulnerable, prevention and early intervention, and making money go further (Community and Opportunity). Significant progress has already been made in these areas, and it is necessary to ensure that this momentum is built upon and developed within the wider context of the need to de-carbonise the economy to reduce the impact of climate change and ensure effective resilience to climate change.
Since January 2013, Hull City Council has held the highest Green Accreditation for its environmental management system, Investors in the Environment and undertaken work to reduce its carbon emissions in line with its corporate targets. It has also undertaken climate adaptation risk assessment for Housing, Museums and Gallery, Waste Management, and Parks and Transport services.
It is necessary to work together to maintain and expand an environment that promotes physical activity and active lifestyle opportunities in everyday settings for all ages. There is also a need to work with partners to ensure the design of the built environment discourages crime and fear of crime.
We need to increase access to traditional environmental spaces including parks, nature areas, gardens, cycle paths, recreational paths and water courses to improve physical and mental well-being and ensure that these are maintained in a sustainable way.
There should be support for sustainable and seasonal approaches to food use within the City to support healthy eating within health and care environments through the Green Kitchen Standard and support residents in cooking and eating healthily.
In terms of improving the environment for the people of Hull, it is important that any measures in the proposed climate change strategy and proposed action plan consider the implications on and as far as possible complement those in the Air Quality Strategy, as some could have a detrimental impact on air quality. For example, monitoring during the COVID-19 lockdown indicates that as direct emissions from vehicles decrease (mono nitrogen oxide and nitrogen dioxide combined) it has the potential to result in an increase in the concentrations of other potentially harmful gases, such as ozone, and only a minimal reduction in the emissions of particulate matter. This has implications and will need to be considered when advocating a change to electric vehicles.
Resources
Ward and Area Committee Area Profiles
Humber and North Yorkshire Health and Care Partnership. https://humberandnorthyorkshire.org.uk/
Public Health England (now Office for Health Improvement & Disparities). Spatial Planning for Health: An evidence resource for planning and designing healthier places, 2017.
https://assets.publishing.service.gov.uk/media/5b59b090e5274a3ff828c70c/spatial_planning_for_health.pdf
Updates
This page was last updated / checked on 19 March 2025.
This page is due to be updated / checked in October 2025.