Index
This topic area covers statistics and information relating to dementia in Hull including local strategic need and service provision.
This page contains information from the Office for Health Improvement & Disparities’ Fingertips. Information is taken ‘live’ from the site so uses the latest available data from Fingertips and displays it on this page. As a result, some comments on this page may relate to an earlier period of time until this page is next updated (see review dates at the end of this page).
Headlines
- Dementia is a syndrome (a group of related symptoms) associated with an ongoing decline of the brain resulting in global impairment. The changes associated with dementia eventually lead to dramatic decline in an individual’s level of functioning. The prevalence increases with age, and the projected numbers are anticipated to increase due to the ageing population.
- Nationally, Alzheimer’s disease has the sixth highest disability adjusted life years (DALYs) and thus has a substantial impact on the quality of people’s lives as well as substantially affecting the lives of carers.
- There were 2,010 patients registered with Hull GPs who had been diagnosed with dementia in 2022/23 representing 0.62% of all registered patients which was lower than England (0.7%). In 2019/20, there were 2,293 patients registered with Hull GPs, but this fell to 1,990 for 2020/21 presumably due to the high mortality rate from COVID-19. The numbers reduced further to 1,915 for 2021/22, although increased for 2022/23.
- NHS England have assigned a national target and ambitions for the dementia diagnosis rate. This has resulted in an increase in the percentage diagnosed out of the estimated number with dementia (estimated by applying age-specific prevalence estimates to the Hull’s population structure). However, with the high mortality rate from COVID-19 in 2020 and 2021 among people with diagnosed dementia, the model has not been adjusted and the percentage diagnosed has fallen relatively sharply from 78.4% in 2020 to 65.1% in 2022. It is likely that the true percentage remains around 78% but that the model is no longer adequately estimating the number of people with dementia, although the increased mortality rate alone does not account for the reduction in the diagnosis rate. It is possible that fewer new cases of dementia were diagnosed during 2020 and 2021 perhaps due to people being less willing or able to attend medical appointments during the COVID-19 pandemic.
- Nationally, three-quarters of people with dementia also have other diseases or medical conditions. Diagnosing other conditions becomes more difficult as the severity of the dementia increases, which can result in other health needs remaining unmet. Persistent stigma against the dementia label can also be a contributing factor for this.
- Mortality rates from dementia are high with around one in ten deaths having dementia as the primary cause of death. The mortality rate from COVID-19 was high among people with dementia. From local analyses, one-fifth of people who died of COVID-19 in Hull during 2020 and 2021 had dementia listed as a secondary cause of death on their death certificate. Given the association between dementia prevalence and age, and between COVID-19 mortality and age, then it is perhaps not surprising that mortality rates were relatively high. It is estimated that an additional 40 people with dementia died during 2020 and 2021. It is possible that people with dementia were more adversely affected compared to similarly-aged people because it was more difficult for them to social distance.
- Due to the ageing population, it is projected that the numbers of people with dementia will increase substantially in Hull over the next 15-20 years.
The Population Affected – Why Is It Important?
Dementia is a common condition and Alzheimer’s Society in 2019 estimated that about 850,000 people were affected in the UK. In 2022/23, from Quality and Outcomes Framework data, 460,330 patients registered with GPs in England had been diagnosed with dementia representing 0.7% of the entire population. There will be additional people with dementia but will not have been diagnosed with dementia. The risk of developing dementia increases with age, and usually occurs in people aged 65+ years. Dementia is a syndrome (a group of related symptoms) associated with an ongoing global decline of the brain and its abilities. This includes problems with memory loss, thinking speed, mental agility, language, understanding and judgement. People with dementia can become apathetic or uninterested in their usual activities, and have problems controlling their emotions. They may also find social situations challenging, lose interest in socialising, and aspects of their personality may change. They may lose empathy (understanding and compassion), may have hallucinations (see or hear things that other people do not), or may make false claims or statements. As dementia affects a person’s mental abilities, they may find planning and organising difficult. Maintaining their independence may also become a problem. A person with dementia will therefore usually need help from friends or relatives, including help with decision making. Most types of dementia can’t be cured, but if it is detected early there are ways to slow it down and maintain mental function.
With the ageing population, the numbers of people with dementia will increase. It is predicted that the numbers of people aged 65+ years with dementia in England will increase from an estimated 679,000 in 2015 to 1,073,500 by 2030, an increase of 58%.
Nationally, Alzheimer’s disease has the sixth highest disability adjusted life years and thus has a substantial impact on the quality of people’s lives as well as substantially affecting the lives of carers.
The diagnosed prevalence of dementia can be examined from data collected as part of the Quality and Outcomes Framework within primary care. Quality of care indicators are also included, and it means that high percentage of the patients diagnosed with dementia have an annual review which gives medical staff the opportunity to provide information, assess their patients and help improve their patients health and wellbeing. Local analysis of the QOF data has been completed with prevalence calculated for each GP practice and Primary Care Network group.
The Hull Picture
Prevalence
The Office for Health Improvement & Disparities’ Fingertips gives the percentage of patients registered with Hull GPs who are diagnosed with dementia. For 2022/23, the prevalence of diagnosed dementia among patients registered with Hull GPs was the lowest across the Humber and North Yorkshire Integrated Care Board at 0.8%, and slightly below England (0.7%).
Compared with benchmark
| Indicator | Period | England | NHS Humber and North Yorkshire Integrated Care Board - QOQ | Humber and North Yorkshire ICB - 02Y | Humber and North Yorkshire ICB - 03F | Humber and North Yorkshire ICB - 03H | Humber and North Yorkshire ICB - 03K | Humber and North Yorkshire ICB - 03Q | Humber and North Yorkshire ICB - 42D |
|---|---|---|---|---|---|---|---|---|---|
Dementia: QOF prevalence (all ages) (Persons All ages) | 2022/23 | 0.7 | 0.8 | 1.0 | 0.6 | 0.8 | 0.8 | 0.7 | 1.0 |
| Indicator | Period | England | NHS Humber and North Yorkshire Integrated Care Board - QOQ | Humber and North Yorkshire ICB - 02Y | Humber and North Yorkshire ICB - 03F | Humber and North Yorkshire ICB - 03H | Humber and North Yorkshire ICB - 03K | Humber and North Yorkshire ICB - 03Q | Humber and North Yorkshire ICB - 42D |
|---|---|---|---|---|---|---|---|---|---|
Dementia: QOF prevalence (all ages) (Persons All ages) | 2022/23 | 0.7 | 0.8 | 1.0 | 0.6 | 0.8 | 0.8 | 0.7 | 1.0 |
Between 2011/12 and 2015/16, the prevalence of dementia among patients registered with Hull GPs has increased quite sharply in Hull as it has in England. An increase would be expected over time given the ageing population, but it is likely that an increase is attributed to NHS England assigning a national target and ambitions for the dementia diagnosis rate.
In 2019/20, there were 2,293 patients registered with Hull GPs who had been diagnosed with dementia representing 0.8% of all the registered population, but this fell to 1,990 patients (0.7%) for 2020/21 and fell further to 1,915 (0.6%) for 2021/22. although this has increased for 2022/23 to 2,011 (0.6%). A high number of deaths from COVID-19 mentioned dementia on the death certificates and this is likely to be the main – but likely not sole – reason for the reduced number of patients with dementia registered with Hull GPs particularly for 2020/21. From a local analysis of mortality rates for 2020 and 2021 (within Causes of Death), it is estimated that around 40 more people with dementia died during 2020 and 2021 than a ‘normal’ or ‘average’ year.
There was also a similar pattern of decrease between 2019/20 and 2022/23 for England and across the Humber and North Yorkshire Integrated Care Board, but the initial decrease in Hull between 2019/20 and 2020/21 greater.
Compared with benchmark
Dementia: QOF prevalence (all ages) (Persons All ages)
|
Period
|
Humber and North Yorkshire ICB - 03F |
NHS Humber and North Yorkshire Integrated Care Board - QOQ
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2011/12 | • | 1289 | 0.4% | 0.4% | 0.5% | - | 0.5% |
| 2012/13 | • | 1362 | 0.5% | 0.4% | 0.5% | - | 0.6% |
| 2013/14 | • | 1529 | 0.5% | 0.5% | 0.6% | - | 0.6% |
| 2014/15 | • | 1861 | 0.6% | 0.6% | 0.7% | - | 0.7% |
| 2015/16 | • | 2002 | 0.7% | 0.6% | 0.7% | - | 0.8% |
| 2016/17 | • | 2132 | 0.7% | 0.7% | 0.7% | - | 0.8% |
| 2017/18 | • | 2193 | 0.7% | 0.7% | 0.8% | - | 0.8% |
| 2018/19 | • | 2262 | 0.8% | 0.7% | 0.8% | - | 0.8% |
| 2019/20 | • | 2293 | 0.8% | 0.7% | 0.8% | 0.9% | 0.8% |
| 2020/21 | • | 1990 | 0.7% | 0.6% | 0.7% | 0.8% | 0.7% |
| 2021/22 | • | 1915 | 0.6% | 0.6% | 0.7% | 0.8% | 0.7% |
| 2022/23 | • | 2011 | 0.6% | 0.6% | 0.7% | 0.8% | 0.7% |
Source: Quality and Outcomes Framework (QOF), NHS England
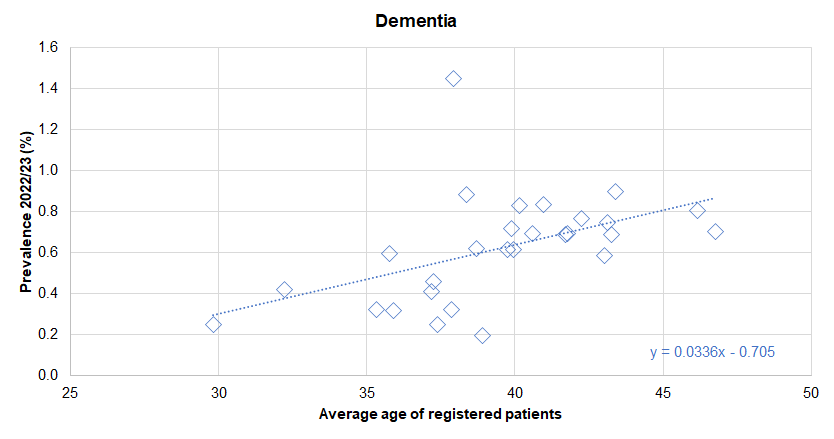
From the local analysis of the national Quality and Outcomes Framework datasets, there was a statistically significant association between average age of the practice patients and the prevalence of diagnosed dementia across the 28 practices in Hull for 2022/23. If the practices were divided into five approximately equal sized groups based on average age of patients (with each fifth having approximately one-fifth of the total registered patients in Hull) then the prevalence increased from 0.4% for the practices serving the youngest practice patients to 0.7% for the practices serving the oldest practice patients. For every increase in the average age of the patients of 10 years, the prevalence of dementia increased by 0.3 percentage points. Further analysis of diagnosed disease by the average age of practice patients is within the file above and within Local Analysis of Quality and Outcomes Framework Data.
There was no statistically significant association between the prevalence of diagnosed dementia and the average deprivation score of registered patients (using the Index of Multiple Deprivation 2019) across the 28 practices.
Fingertips also presents the data for single years for those aged 65+ years for 2020. The prevalence for Hull (03F) at 4.16% is the highest across the Humber and North Yorkshire Integrated Care Board, and higher than England (3.97%) and the ICB average (3.67%).
Compared with benchmark
| Indicator | Period | England | NHS Humber and North Yorkshire Integrated Care Board - QOQ | Humber and North Yorkshire ICB - 02Y | Humber and North Yorkshire ICB - 03F | Humber and North Yorkshire ICB - 03H | Humber and North Yorkshire ICB - 03K | Humber and North Yorkshire ICB - 03Q | Humber and North Yorkshire ICB - 42D |
|---|---|---|---|---|---|---|---|---|---|
Dementia: Recorded prevalence (aged 65 years and over) (Persons 65+ yrs) | 2020 | 3.97 | 3.71 | 3.67 | 4.16 | 3.96 | 3.42 | 3.42 | 3.75 |
| Indicator | Period | England | NHS Humber and North Yorkshire Integrated Care Board - QOQ | Humber and North Yorkshire ICB - 02Y | Humber and North Yorkshire ICB - 03F | Humber and North Yorkshire ICB - 03H | Humber and North Yorkshire ICB - 03K | Humber and North Yorkshire ICB - 03Q | Humber and North Yorkshire ICB - 42D |
|---|---|---|---|---|---|---|---|---|---|
Dementia: Recorded prevalence (aged 65 years and over) (Persons 65+ yrs) | 2020 | 3.97 | 3.71 | 3.67 | 4.16 | 3.96 | 3.42 | 3.42 | 3.75 |
In 2020, the prevalence of dementia decreased in Hull as it did in England, although to a lesser extent in England (14% versus 9%). As the 2020 file was taken from the December 2020 data extract, it is likely that the mortality rate from COVID-19 was an influential factor in the reduction in prevalence.
Compared with benchmark
Dementia: Recorded prevalence (aged 65 years and over) (Persons 65+ yrs)
|
Period
|
Humber and North Yorkshire ICB - 03F |
NHS Humber and North Yorkshire Integrated Care Board - QOQ
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2017 | • | 2158 | 4.73% | 4.54% | 4.93% | 4.14% | 4.33% |
| 2018 | • | 2195 | 4.76% | 4.57% | 4.96% | 4.17% | 4.32% |
| 2019 | • | 2237 | 4.81% | 4.62% | 5.01% | 4.08% | 4.34% |
| 2020 | • | 1951 | 4.16% | 3.98% | 4.35% | 3.71% | 3.97% |
Source: NHS Digital, Recorded Dementia Diagnoses publications, December data files
Age-gender specific prevalence estimates for dementia have been estimated given the characteristics of the population in the Cognitive Function and Ageing Study II among people aged 65+ years. These estimates have been applied to the age gender structure of the populations of each geographical area authority to estimate the number of people with diagnosed and undiagnosed dementia.
This estimated number of people with dementia has been then compared with the number diagnosed on the GP disease registers. For 2023, it was estimated that 67.8% of people with diagnosed and undiagnosed dementia among patients registered with Hull GPs (03F).
Compared with benchmark
| Indicator | Period | England | NHS Humber and North Yorkshire Integrated Care Board - QOQ | Humber and North Yorkshire ICB - 02Y | Humber and North Yorkshire ICB - 03F | Humber and North Yorkshire ICB - 03H | Humber and North Yorkshire ICB - 03K | Humber and North Yorkshire ICB - 03Q | Humber and North Yorkshire ICB - 42D |
|---|---|---|---|---|---|---|---|---|---|
Estimated dementia diagnosis rate (aged 65 and older) (Persons 65+ yrs) | 2023 | 63.0 | 58.1 | 57.5 | 67.8 | 59.4 | 53.4 | 53.3 | 59.1 |
| Indicator | Period | England | NHS Humber and North Yorkshire Integrated Care Board - QOQ | Humber and North Yorkshire ICB - 02Y | Humber and North Yorkshire ICB - 03F | Humber and North Yorkshire ICB - 03H | Humber and North Yorkshire ICB - 03K | Humber and North Yorkshire ICB - 03Q | Humber and North Yorkshire ICB - 42D |
|---|---|---|---|---|---|---|---|---|---|
Estimated dementia diagnosis rate (aged 65 and older) (Persons 65+ yrs) | 2023 | 63.0 | 58.1 | 57.5 | 67.8 | 59.4 | 53.4 | 53.3 | 59.1 |
In 2020, it was estimated that 2,207 out of 2,815 people (78.4%) with dementia had been diagnosed, but in 2021, it was estimated that 1,920 out of 2,783 (69.0%) were diagnosed and this further fell to 1,838 people out of 2,823 (65.1%) in 2022.
The estimated number of people with dementia (diagnosed and undiagnosed) using the modelled estimate remained relatively unchanged for 2020 (2,815 people), 2021 (2,783 people) and 2022 (2,823 people), yet we know that the mortality rate was much higher among patients with dementia in 2020 (and perhaps 2021) due to COVID-19. Between 2019/20 and 2021/22, there was a reduction of 16% in the number of people with diagnosed dementia on the Quality and Outcomes Framework GP disease registers (2,293 to 1,915), yet the model estimates remained relatively unchanged.
The percentage diagnosed can increase a great deal in a short period of time if there are high levels of patients undiagnosed and a case-finding exercise is undertaken, but the same argument does not apply for a decrease in the percentage. There is no plausible reason why the percentage diagnosed would fall by a large amount unless there is a substantial change to the nursing or care homes within the area or a change to geographical boundaries (e.g. a care home specialising in dementia patients moves to another local authority). Yet the percentage has fallen from 78% to 65% in a two year period.
Thus, it is likely that the percentage diagnosed remains around 78%, but that the model has not taken into account the high COVID-19 mortality rate among patients with dementia and is producing an artificially high estimate of the number of people with diagnosed and undiagnosed dementia. However, it is estimated that around 40 additional people with dementia died during 2020 and 2021, so this does not account fully for the sharp decrease in the percentage diagnosed. It is possible that there were fewer new cases of dementia diagnosed during 2020 and 2021 due to the COVID-19 pandemic, for instance, people – particularly frail and vulnerable people – with symptoms may have been less likely to visit their GP during this time and thus less likely to be diagnosed with dementia.
The numbers diagnosed and the percentage diagnosed has increased in the last year to 1,916 people diagnosed in 2023 representing an estimated 67.8% of all people with diagnosed and undiagnosed dementia. However, this is considerably lower than the numbers prior to the pandemic, and whilst the pandemic may account for some of the difference, it is not clear why the overall numbers and percentage diagnosed have decreased so much, although the pattern nationally is similar albeit not reducing as much.
Compared with benchmark
Estimated dementia diagnosis rate (aged 65 and older) (Persons 65+ yrs)
|
Period
|
Humber and North Yorkshire ICB - 03F |
NHS Humber and North Yorkshire Integrated Care Board - QOQ
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2017 | • | 2083 | 76.8 | 68.4 | 84.0 | - | 67.9 |
| 2018 | • | 2130 | 77.1 | 68.7 | 84.3 | - | 67.5 |
| 2019 | • | 2188 | 78.3 | 69.8 | 85.7 | 66.2 | 68.7 |
| 2020 | • | 2207 | 78.4 | 69.8 | 85.7 | 64.3 | 67.4 |
| 2021 | • | 1920 | 69.0 | 61.3 | 75.5 | 58.5 | 61.6 |
| 2022 | • | 1838 | 65.1 | 57.8 | 71.3 | 57.5 | 62.0 |
| 2023 | • | 1916 | 67.8 | 60.2 | 74.2 | 58.1 | 63.0 |
Source: NHS Digital
Hospital Admissions
The directly standardised hospital admission rate for emergency admissions among people aged 65+ years with dementia is 29% higher than England. The rate is given as the number of all emergency admissions per 100,000 population (in the European Standard Population) regardless of the primary cause of the admission where either the primary cause or any of the secondary causes of the admission are recorded as dementia. There were 4,351 emergency admissions among patients registered with Hull GPs (03F) who were aged 65+ years who have dementia in 2019/20.
Compared with benchmark
| Indicator | Period | England | NHS Humber and North Yorkshire Integrated Care Board - QOQ | Humber and North Yorkshire ICB - 02Y | Humber and North Yorkshire ICB - 03F | Humber and North Yorkshire ICB - 03H | Humber and North Yorkshire ICB - 03K | Humber and North Yorkshire ICB - 03Q | Humber and North Yorkshire ICB - 42D |
|---|---|---|---|---|---|---|---|---|---|
Dementia: Direct standardised rate of emergency admissions (aged 65 years and over) - CCG responsibility (Persons 65+ yrs) | 2019/20 | 3517 | 3117 | 3095 | 4351 | 2752 | 3225 | 3215 | 2629 |
| Indicator | Period | England | NHS Humber and North Yorkshire Integrated Care Board - QOQ | Humber and North Yorkshire ICB - 02Y | Humber and North Yorkshire ICB - 03F | Humber and North Yorkshire ICB - 03H | Humber and North Yorkshire ICB - 03K | Humber and North Yorkshire ICB - 03Q | Humber and North Yorkshire ICB - 42D |
|---|---|---|---|---|---|---|---|---|---|
Dementia: Direct standardised rate of emergency admissions (aged 65 years and over) - CCG responsibility (Persons 65+ yrs) | 2019/20 | 3517 | 3117 | 3095 | 4351 | 2752 | 3225 | 3215 | 2629 |
There were over 4,800 emergency admissions per 100,000 population in 2016/17 and 2017/18, but this fell to 4,242 admissions per 100,000 population in 2018/19, and then increased to 4,351 admissions per 100,000 population in 2019/20. Over the same four years, there were around 3,400 admissions per 100,000 population for England.
There were 1,940 emergency hospital admissions among patients with dementia registered with Hull GPs during 2019/20.
Compared with benchmark
Dementia: Direct standardised rate of emergency admissions (aged 65 years and over) - CCG responsibility (Persons 65+ yrs)
|
Period
|
Humber and North Yorkshire ICB - 03F |
NHS Humber and North Yorkshire Integrated Care Board - QOQ
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2016/17 | • | 2120 | 4881 | 4673 | 5095 | - | 3365 |
| 2017/18 | • | 2110 | 4866 | 4658 | 5081 | 3211 | 3471 |
| 2018/19 | • | 1865 | 4242 | 4050 | 4440 | 3072 | 3480 |
| 2019/20 | • | 1940 | 4351 | 4158 | 4551 | 3117 | 3517 |
Source: NHS Digital
Deaths
The directly standardised mortality rate for people aged 65+ years with dementia who are registered with Hull GPs (03F) is over 40% higher than England. The rate is given as the number of deaths per 100,000 population (in the European Standard Population) where the underlying cause of death or contributory cause of death is classified as dementia or Alzheimer’s disease.
Compared with benchmark
| Indicator | Period | England | NHS Humber and North Yorkshire Integrated Care Board - QOQ | Humber and North Yorkshire ICB - 02Y | Humber and North Yorkshire ICB - 03F | Humber and North Yorkshire ICB - 03H | Humber and North Yorkshire ICB - 03K | Humber and North Yorkshire ICB - 03Q | Humber and North Yorkshire ICB - 42D |
|---|---|---|---|---|---|---|---|---|---|
Direct standardised rate of mortality: People with dementia (aged 65 years and over) (Persons 65+ yrs) | 2019 | 849 | 848 | 874 | 1196 | 1106 | 722 | 776 | 725 |
| Indicator | Period | England | NHS Humber and North Yorkshire Integrated Care Board - QOQ | Humber and North Yorkshire ICB - 02Y | Humber and North Yorkshire ICB - 03F | Humber and North Yorkshire ICB - 03H | Humber and North Yorkshire ICB - 03K | Humber and North Yorkshire ICB - 03Q | Humber and North Yorkshire ICB - 42D |
|---|---|---|---|---|---|---|---|---|---|
Direct standardised rate of mortality: People with dementia (aged 65 years and over) (Persons 65+ yrs) | 2019 | 849 | 848 | 874 | 1196 | 1106 | 722 | 776 | 725 |
The mortality rate for dementia for people aged 65+ years has increased in Hull between 2016 and 2019.
There were 435 such deaths among Hull residents aged 65+ years in 2019.
Compared with benchmark
Direct standardised rate of mortality: People with dementia (aged 65 years and over) (Persons 65+ yrs)
|
Period
|
Humber and North Yorkshire ICB - 03F |
NHS Humber and North Yorkshire Integrated Care Board - QOQ
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2016 | • | 388 | 1076 | 971 | 1190 | - | 866 |
| 2017 | • | 429 | 1203 | 1090 | 1324 | 913 | 901 |
| 2018 | • | 428 | 1178 | 1068 | 1297 | 897 | 904 |
| 2019 | • | 435 | 1196 | 1085 | 1315 | 848 | 849 |
Source: Public Health England (Office for National Statistics Mortality File)
Using the local mortality data file, there were 13,135 deaths in total over the five years 2018 to 2022, with 1,110 having the primary cause of death as dementia on the death certificate representing 8.5% of all deaths. An additional 769 (5.9%) deaths had dementia listed as a secondary cause of death on the death certificate.
Over this five year period, there was an average of 222 deaths per year where dementia was the primary cause of death with relatively small levels of year-on-year variability ranging from 242 to 250 per year for 2018-2020, and 186 and 187 in 2021 and 2022. This discrepancy may be due to COVID-19, as deaths from COVID were mostly among the elderly, as are most dementia deaths, so many who might have died in from dementia in subsequent years had died from COVID-19. On average, there were 133 deaths per year on average where dementia was listed as a secondary cause of death, ranging between 124 and 225 deaths per year, with the highest figure occurring in 2020 when COVID-19 deaths in Hull peaked at 406, of which 106 (26%) had dementia listed as a secondary cause of death. If we exclude 2020, the variability was relatively low with the numbers ranging from 124 to 153 per year).
During 2019, fewer people with dementia died at their usual place of residence in Hull compared to England, with a likely higher percentage dying in hospital.
Compared with benchmark
COVID-19 Deaths Among People With Dementia
During the two year period 2018 to 2019, there were 495 deaths where dementia was given as the underlying cause of death (9.8% of all deaths), and this was similar for the two year period 2020 to 2021 (429 deaths representing 9.1% of all deaths).
However, there were a further 267 deaths in 2018-19 where dementia was given as a secondary / contributing cause of death on the death certificate compared to 377 such deaths in 2020-21. Of these 377 deaths in 2020-21, 149 had the underlying cause of death as COVID-19 (out of the 713 COVID-19 deaths) with the remaining 228 deaths due to other causes.
Thus, during the two year period 2018-19, there were 762 deaths where dementia was the underlying cause of death or a secondary cause of death compared to 806 such deaths in 2020-21. Thus it is estimated that around 40 more deaths among people with dementia occurred during 2020-21 compared to the average of 2018-19.
Projected Numbers with Dementia
The Projecting Adult Needs and Service Information (PANSI) and the Projecting Older People Population Information Service (POPPI) provide current estimates and future projections at local authority level of the number of people with different health needs for those aged 16-64 and 65+ years respectively.
They use estimates for the estimated prevalence from different surveys and research which have generally been derived at a national level (generally different prevalence estimates for different age groups for men and women separately). They then apply these prevalence figures to Hull’s population. For instance, if the prevalence among males in England in a specific age group is 5% and there are an estimated 500 men living in Hull in that age groups, they would estimate there were 25 men in that age group living in Hull with that condition. For many conditions, there is an increased prevalence in populations with higher levels of deprivation, and in most cases, deprivation is not taken into consideration. Thus in many cases, these estimates for Hull are likely to underestimate the numbers in Hull due to the high levels of deprivation in Hull.
Further definitions are available from www.pansi.org.uk and www.poppi.org.uk.
They estimate that over 60 people in Hull aged 18-64 years have early-onset dementia.
| Gender | Age | 2020 | 2025 | 2030 | 2035 | 2040 |
| Males | 30-39 | 2 | 2 | 1 | 1 | 1 |
| Males | 40-49 | 3 | 3 | 3 | 3 | 3 |
| Males | 50-59 | 20 | 18 | 17 | 16 | 17 |
| Males | 60-64 | 14 | 15 | 14 | 13 | 12 |
| Males | Total 18-64 | 38 | 38 | 36 | 33 | 33 |
| Females | 30-39 | 2 | 2 | 2 | 2 | 2 |
| Females | 40-49 | 3 | 3 | 4 | 4 | 4 |
| Females | 50-59 | 12 | 11 | 10 | 10 | 11 |
| Females | 60-64 | 8 | 9 | 8 | 8 | 7 |
| Females | Total 18-64 | 26 | 26 | 24 | 23 | 22 |
They estimate that there are almost 2,600 residents of Hull aged 65+ years who have dementia. Note that this is the number of Hull residents and includes people with undiagnosed dementia. It will also differ from the figures mentioned above as these relate to patients registered with Hull GPs (there are around 300,000 patients registered with Hull GPs but the Office for National Statistics estimates that there are around 260,000 residents of Hull). They estimate that the numbers with dementia aged 65+ years will increase to around 3,500 people by 2040.
| Age | 2020 | 2025 | 2030 | 2035 | 2040 |
| 65-69 | 193 | 210 | 233 | 220 | 202 |
| 70-74 | 332 | 314 | 341 | 387 | 366 |
| 75-79 | 420 | 551 | 521 | 582 | 653 |
| 80-84 | 598 | 587 | 785 | 751 | 852 |
| 85-89 | 565 | 595 | 595 | 807 | 772 |
| 90+ | 472 | 436 | 460 | 519 | 672 |
| Total 65+ | 2,581 | 2,693 | 2,935 | 3,265 | 3,516 |
Co-Morbidity
Currently it is not possible to determine the exact numbers of people in Hull with dementia and other conditions. However national estimates from the Office for Health Improvement & Disparities (formerly Public Health England) identified the following:
- A total of 77% of patients with dementia had at least one of the specific health conditions considered within their study. This compared to 68% in the ‘all patient’ group for the same list of health conditions (excluding dementia).
- For patients with dementia, 44% had a diagnosis of hypertension, between 17% and 20% had a diagnosis of diabetes, stroke or transient ischaemic attack (mini stroke), coronary heart disease or depression, while between 9% and 11% had a diagnosis of Parkinsonism, chronic obstructive pulmonary disease or asthma.
- The prevalence rate for eight of the 10 specific health conditions is higher for patients with dementia when compared to the all patient group. The prevalence rates for hypertension and asthma are lower than the all patient group.
- Patients with dementia are more likely to have multiple health conditions. A total of 22% with three or more comorbidities and 8% with four or more comorbidities, compared to 11% and 3% respectively in the all patient group.
- The proportion of patients aged 85 years and older with two or more other health conditions recorded in the primary care notes is lower than the proportion in age groups under 85 years. Diagnosing comorbidities in patients with dementia can be more difficult to achieve as the severity of dementia increases. However, it can lead to comorbid conditions being under-diagnosed and thus health needs of patients remaining unmet.
Strategic Need and Service Provision
Many of the disabling effects of dementia can be combated using the social model of disability, and Hull is seeking to become a Dementia Friendly City by providing advice and training to people. Universal services will be adapted to be dementia-friendly to enable people with dementia to independently access banks, shops, and other community hubs. This will enable them to feel more empowered and confident which in turn will increase wellbeing whilst reducing their reliance on carers and on paid support. They can also choose to participate and contribute to meaningful activities which will improve their self-esteem.
It is also important that a person with dementia has other medical conditions and diseases diagnosed and treated appropriately to lessen the burden on the individuals, carers and overall health care system.
There is a need to work with partners to ensure that there is a shared understanding of people’s needs and that services are integrated, high quality and accessible in ways that offer people appropriate choices such as care organised around care hubs. There is a need to work together to promote self-care, reablement or mutual support in community settings so this is viewed as the norm and reduce reliance on residential or home care. The most vulnerable citizens should be identified so their specific needs are addressed in the way they wish. The Care Act 2014 focuses around meeting needs and promoting wellbeing rather than simply the provision of services and on preventing, reducing or delaying the development of need, so individual needs should be assessed holistically within the context of their support network and each individual’s circumstances considered to provide the most appropriate care, help and support for that individual. These individual needs will need to consider the caring arrangements, and how carers need to be supported in their role, and that their health needs do not suffer.
People (supported by their carers where necessary) should be encouraged to attend their NHS Health Check if they are eligible, and people already diagnosed with dementia should attend their annual reviews (generally within primary care) so that they get the best on-going treatment for their condition.
Resources
NHS Digital. Quality and Outcomes Framework. https://qof.digital.nhs.uk/
The Office for Health Improvement & Disparities’ Fingertips. https://fingertips.phe.org.uk/
Projecting Older People Population Information Service – POPPI. www.poppi.org.uk
Projecting Older People Population Information Service – PANSI. www.pansi.org.uk
NHS. Dementia guide. www.nhs.uk. 2013, NHS: London.
Newton, J.N., et al., Changes in health in England, with analysis by English regions and areas of deprivation, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet, 2015. 386(10010): p. 2257-2274.
Updates
This page was last updated / checked on 22 January 2024.
This page is due to be updated / checked in June 2024.