Index
This topic area covers statistics and information relating to mental ill health in Hull including local strategic need and service provision. Further information relating to Mental Health and Emotional Wellbeing (and Self-Harm and Suicide for adults) is given under Health Factors within Adults and within Children and Young People. A needs assessment was completed in Hull during 2023 for people with multiple unmet needs which included people who had poor mental health. The report – which was finalised in 2024 – is available within Multiple Unmet Needs under Vulnerable Groups.
This page contains information from the Office for Health Improvement & Disparities’ Fingertips. Information is taken ‘live’ from the site so uses the latest available data from Fingertips and displays it on this page. As a result, some comments on this page may relate to an earlier period of time until this page is next updated (see review dates at the end of this page).
Headlines
- Severe mental illness affects around 1% of the population, and almost 2% of the population in the most deprived fifth of areas of England (which encompasses just over half of Hull). With an estimated resident population of around 272,000 in 2023, this equates to between 2,720 and 5,440 residents of Hull affected by severe mental ill health.
- Mental ill health is also a significant risk factor for suicide.
- It has profound effects not just on the individual including on their physical health, but on their families, community and on the health system. People with severe mental illness die on average 15 to 20 years earlier than the general population.
- In 2023/24, 2,928 (0.93%) patients registered with Hull GPs were diagnosed with severe mental illness (with a diagnosis of schizophrenia, bipolar affective disorder and other psychosis). This is marginally lower than the prevalence for England at 0.96%, but as severe mental illness is associated with deprivation, it is likely that there are additional people in Hull with severe mental illness who have not been diagnosed and who are not included on the GP severe mental illness register.
- Just under three-quarters of adults in contact with secondary mental health services are in stable and appropriate accommodation, and around one in nine are in paid employment.
- In 2014/15, over half of people with severe mental illness in Hull smoked.
- The premature (under 75) mortality is significantly higher among adults aged 18-74 years with severe mental ill health (defined as having a referral to secondary mental health services in the five years preceding death (excluding learning disabilities and autism) compared to people without severe mental ill health. Premature mortality rates among people with severe mental ill health is also statistically significantly higher in Hull compared to England.
- For deaths registered during 2021-23, the premature mortality among adults with severe mental ill health in Hull was almost twice as high as England (198 versus 111 deaths per 100,000 population). This is also the case for premature deaths from cardiovascular disease, cancer and respiratory disease. Whilst the premature mortality rate from liver disease among adults with severe mental ill health was also statistically significantly higher in Hull compared to England, the differential was lower as it was 57% higher.
- There were 3,314 premature deaths registered in Hull during 2021-23 (around 60 were prior to the age of 18 years) so around 3,250 premature deaths in total among those aged 18-74 years. Around one-third (1,035) had been referred to secondary mental health services in the previous five years. These figures were around one-quarter for cardiovascular deaths (210 out of 774), just under one-fifth for cancer (200 out of 1,037), around four in ten for liver disease (70 out of 174) and around one-third for respiratory disease (115 out of 342). The disease-specific figures are approximate as the number of premature deaths among people referred to secondary mental health services have been rounded to the nearest five and the total has the potential to include a very small number of children and young people aged under 18 years.
- Measures of the excess premature mortality rate have been presented and illustrate the degree to which premature mortality rates among adults with severe mental ill health are higher compared to adults without severe mental ill health. Overall, premature mortality rate is 159% higher in Hull among adults with severe mental ill health are higher compared to adults without severe mental ill health for deaths registered during 2021-23 (114% for cardiovascular disease, 50% for cancer, 256% for liver disease and 227% for respiratory disease).
- Premature mortality rates in Hull among all individuals are much higher than England, so when the excess premature mortality rate is compared to England, the percentages are statistically significantly lower.
- The COVID-19 pandemic has had a significant impact on people’s mental health and emotional wellbeing, and the effects of which could be an increased need for services in the coming years. Furthermore, the pandemic has tended to have had a more adverse affect on people living in the most deprived areas thus increasing the inequalities gap.
The Population Affected – Why Is It Important?
The World Health Organization states:
- There are many different mental disorders, with different presentations. They are generally characterised by a combination of abnormal thoughts, perceptions, emotions, behaviour and relationships with others.
- Mental disorders include: depression, bipolar disorder, schizophrenia and other psychoses, dementia, and developmental disorders including autism.
- There are effective strategies for preventing mental disorders such as depression.
- There are effective treatments for mental disorders and ways to alleviate the suffering caused by them.
- Access to health care and social services capable of providing treatment and social support is key.
The Global Burden of Disease estimates that in 2013 depressive disorders ranked eighth highest for causes of disability-adjusted life years in England.
The Surrey and Borders Partnership NHS Foundation Trust provided a useful summary of severe mental illness. They state that there are many types of mental illness but most of them can be classified as either psychotic or neurotic. Neurotic conditions are related to ‘normal’ emotions but are more extreme, and are the most common types of mental illness. Being clinically depressed is a far deeper experience than ‘feeling depressed’, and has a marked effect on life, preventing the patient from looking after themselves or being able to work, and in extreme cases can lead to suicide. Other examples of neurotic illnesses are phobias, obsessive compulsive disorder and anxiety. Psychotic conditions are unrelated to normal emotions, and the word psychosis is used to describe symptoms or experiences that happen together. These symptoms cause the patient to not experience reality like most people. Symptoms may include hallucinations, delusions, thought disorder, lack of insight and not recognising that they are unwell, and appearing unusually excited or withdrawn and avoiding contact with other people. Examples include schizophrenia, bipolar disorder (manic depression) and psychotic depression.
In their Severe Mental Illness and Physical Health Inequalities briefing in 2018, The Office for Health Improvement & Disparities (formerly Public Health England) give a prevalence of around 1% for severe mental illness, although it is slightly higher among women compared to men, and higher among those aged 35-74 years compared to those aged 15-34 years. The prevalence is around 0.5% for people living in the least deprived fifth of areas of England compared to around 1.8% for people living in the most deprived fifth of areas of England.
NHS England discuss the serious inequalities with regard to serious mental health and links to physical health. They state that serious mental illness obviously has a huge effect on mental wellbeing, but can also influence physical health. People with serious mental health are more likely to have poor physical health, and people with poor physical health are more likely to have poor mental health. People with serious mental illness are also more likely to have unhealthily lifestyles further affecting health and wellbeing. There is a recognition that smoking rates are very high with around one-third of people with mental health problems and two-thirds of people in psychiatric units smoking. In The Office for Health Improvement & Disparities’ 2018 briefing, the mortality rates of people with severe mental illness with the general population, and people with severe mental illness:
- die on average 15 to 20 years earlier than the general population.
- have 3.7 times higher death rate for ages under 75 years than the general population.
- experience a widening gap in death rates over time.
They go on to state that two in three deaths from physical illnesses can be prevented among people with severe mental illness.
The diagnosed prevalence of severe mental illness can be examined from data collected as part of the Quality and Outcomes Framework within primary care. Severe mental illness was defined as having a diagnosis of schizophrenia, bipolar affective disorder or other psychosis. Quality of care indicators are also included, and it means that high percentage of the patients diagnosed with severe mental illness have annual reviews which gives medical staff the opportunity to provide information and encourage their patients to improve their lifestyle behaviours to improve their health, and lower their risk of morbidity and mortality from their condition. Local analysis of the QOF data has been completed with prevalence calculated for each GP practice and Primary Care Network group.
The Hull Picture
Severe Mental Ill Health Among Patients Registered to Hull GPs
The Office for Health Improvement & Disparities’ Fingertips presents information from the Quality and Outcomes Framework on severe mental illness (schizophrenia, bipolar affective disorder or other psychosis).
The sub Integrated Care Board areas which include Hull are within the Humber and North Yorkshire Integrated Care Board. In Fingertips, the sub-ICB area referenced by 03F relates to Hull (see Integrated Care Board for the codes relating to the other local sub-ICB areas).
In 2023/24, there were 2,928 patients registered with Hull GPs diagnosed with severe mental illness which is very similar to the prevalence in England (0.93% versus 0.96%).
There is a strong association between deprivation and severe mental illness, and whilst the prevalence in Hull is slightly lower than England in 2023/24. It is likely that a higher percentage of people have severe mental illness but have not been diagnosed in Hull due to the high levels of deprivation in Hull.
Compared with benchmark
| Indicator | Period | England | NHS Humber and North Yorkshire Integrated Care Board - QOQ | Humber and North Yorkshire ICB - 02Y | Humber and North Yorkshire ICB - 03F | Humber and North Yorkshire ICB - 03H | Humber and North Yorkshire ICB - 03K | Humber and North Yorkshire ICB - 03Q | Humber and North Yorkshire ICB - 42D |
|---|---|---|---|---|---|---|---|---|---|
Mental Health: QOF prevalence (Persons All ages) | 2023/24 | 1.0 | 0.8 | 0.7 | 0.9 | 0.9 | 0.8 | 0.8 | 0.9 |
| Indicator | Period | England | NHS Humber and North Yorkshire Integrated Care Board - QOQ | Humber and North Yorkshire ICB - 02Y | Humber and North Yorkshire ICB - 03F | Humber and North Yorkshire ICB - 03H | Humber and North Yorkshire ICB - 03K | Humber and North Yorkshire ICB - 03Q | Humber and North Yorkshire ICB - 42D |
|---|---|---|---|---|---|---|---|---|---|
Mental Health: QOF prevalence (Persons All ages) | 2023/24 | 1.0 | 0.8 | 0.7 | 0.9 | 0.9 | 0.8 | 0.8 | 0.9 |
On the whole, the prevalence has been slowly increasing in Hull. It is not known if this reflects an increased prevalence or higher rates of diagnosis and better recording. The prevalence in Hull has been very similar to England especially between 2017/18 and 2022/23, although has fallen in Hull in the last year by a greater amount than the decrease for England so the recorded prevalence in Hull is now marginally lower than England.
Compared with benchmark
Mental Health: QOF prevalence (Persons All ages)
|
Period
|
Humber and North Yorkshire ICB - 03F |
NHS Humber and North Yorkshire Integrated Care Board - QOQ
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2012/13 | • | 2340 | 0.8% | 0.8% | 0.8% | 0.7% | 0.8% |
| 2013/14 | • | 2394 | 0.8% | 0.8% | 0.9% | 0.7% | 0.9% |
| 2014/15 | • | 2487 | 0.9% | 0.8% | 0.9% | 0.7% | 0.9% |
| 2015/16 | • | 2575 | 0.9% | 0.8% | 0.9% | 0.8% | 0.9% |
| 2016/17 | • | 2688 | 0.9% | 0.8% | 0.9% | 0.8% | 0.9% |
| 2017/18 | • | 2774 | 0.9% | 0.9% | 1.0% | 0.8% | 0.9% |
| 2018/19 | • | 2927 | 1.0% | 0.9% | 1.0% | 0.8% | 1.0% |
| 2019/20 | • | 2808 | 0.9% | 0.9% | 1.0% | 0.8% | 0.9% |
| 2020/21 | • | 2878 | 0.9% | 0.9% | 1.0% | 0.8% | 0.9% |
| 2021/22 | • | 2938 | 1.0% | 0.9% | 1.0% | 0.8% | 1.0% |
| 2022/23 | • | 3076 | 1.0% | 1.0% | 1.0% | 0.9% | 1.0% |
| 2023/24 | • | 2928 | 0.9% | 0.9% | 1.0% | 0.8% | 1.0% |
Source: NHS England
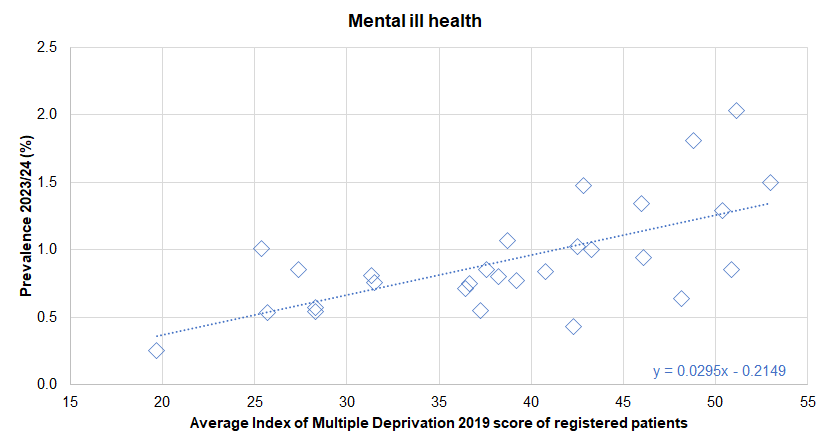
There was a statistically significant association between average deprivation score of registered patients (based on the Index of Multiple Deprivation 2019) and the prevalence of diagnosed severe mental ill health across the 28 practices in Hull for 2023/24. The prevalence was 0.7% among practices serving the patients living in the least deprived areas of Hull compared to 1.4% among practices serving the patients living in the least deprived areas of Hull. For every increase in the deprivation score of 10 units, the prevalence of severe mental ill health increased by 0.3 percentage points. Further analysis of diagnosed disease by the average deprivation score of practice patients is given within Local Analysis of Quality and Outcomes Framework Data.
There was no statistically significant association between the prevalence of diagnosed severe mental ill health and the average age of registered patients across the 28 practices.
Stable and Appropriate Accommodation Among Secondary Mental Health Service Users
Fingertips presents information on the percentage of people in contact with secondary mental health services who are in stable and appropriate accommodation. For 2020/21, the percentage in Hull at 70% was much higher than England (58%), although the percentages were considerably higher among Hull women (78%) compared to Hull men (63%).
Compared with benchmark
| Indicator | Period | England | Yorkshire and the Humber region (statistical) | Kingston upon Hull | East Riding of Yorkshire | North East Lincolnshire | North Lincolnshire | York | North Yorkshire UA | Barnsley | Doncaster | Rotherham | Sheffield | Bradford | Calderdale | Kirklees | Leeds | Wakefield |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Adults in contact with secondary mental health services who live in stable and appropriate accommodation (Persons 18-69 yrs) | 2020/21 | 58.0 | 65.0 | 70.0 | 84.0 | 78.0 | 33.0 | 73.0 | 73.0 | 83.0 | 43.0 | 65.0 | 42.0 | 77.0 | 71.0 | 73.0 | 15.0 | 72.0 |
Adults in contact with secondary mental health services who live in stable and appropriate accommodation (Male 18-69 yrs) | 2020/21 | 56.0 | 62.0 | 63.0 | 78.0 | 76.0 | 36.0 | 70.0 | 70.0 | 80.0 | 39.0 | 59.0 | 41.0 | 75.0 | 69.0 | 71.0 | 14.0 | 68.0 |
Adults in contact with secondary mental health services who live in stable and appropriate accommodation (Female 18-69 yrs) | 2020/21 | 59.0 | 69.0 | 78.0 | 90.0 | 80.0 | 30.0 | 76.0 | 76.0 | 86.0 | 50.0 | 72.0 | 42.0 | 79.0 | 74.0 | 75.0 | 16.0 | 77.0 |
| Indicator | Period | England | Yorkshire and the Humber region (statistical) | Kingston upon Hull | East Riding of Yorkshire | North East Lincolnshire | North Lincolnshire | York | North Yorkshire UA | Barnsley | Doncaster | Rotherham | Sheffield | Bradford | Calderdale | Kirklees | Leeds | Wakefield |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Adults in contact with secondary mental health services who live in stable and appropriate accommodation (Persons 18-69 yrs) | 2020/21 | 58.0 | 65.0 | 70.0 | 84.0 | 78.0 | 33.0 | 73.0 | 73.0 | 83.0 | 43.0 | 65.0 | 42.0 | 77.0 | 71.0 | 73.0 | 15.0 | 72.0 |
Adults in contact with secondary mental health services who live in stable and appropriate accommodation (Male 18-69 yrs) | 2020/21 | 56.0 | 62.0 | 63.0 | 78.0 | 76.0 | 36.0 | 70.0 | 70.0 | 80.0 | 39.0 | 59.0 | 41.0 | 75.0 | 69.0 | 71.0 | 14.0 | 68.0 |
Adults in contact with secondary mental health services who live in stable and appropriate accommodation (Female 18-69 yrs) | 2020/21 | 59.0 | 69.0 | 78.0 | 90.0 | 80.0 | 30.0 | 76.0 | 76.0 | 86.0 | 50.0 | 72.0 | 42.0 | 79.0 | 74.0 | 75.0 | 16.0 | 77.0 |
The percentage of people in contact with secondary mental health services who are in settled accommodation increased in Hull between 2011/12 and 2017/18, but has subsequently fallen over the last three years. Despite the recent fall, the percentage in Hull has been consistently and significantly higher than England.
Compared with benchmark
Adults in contact with secondary mental health services who live in stable and appropriate accommodation (Persons 18-69 yrs)
|
Period
|
Kingston upon Hull |
Yorkshire and the Humber region (statistical)
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2011/12 | • | - | 61.6% | 58.8% | 64.8% | 55.3% | 54.6% |
| 2012/13 | • | - | 58.8% | 55.6% | 61.9% | 63.1% | 58.5% |
| 2013/14 | • | - | 56.2% | 52.3% | 60.0% | 63.2% | 60.8% |
| 2014/15 | • | - | 68.5% | 64.8% | 72.0% | 67.2% | 59.7% |
| 2015/16 | • | - | 73.4% | 70.2% | 76.4% | 64.7% | 58.6% |
| 2016/17 | • | - | 77.0% | 74.1% | 79.7% | 71.0% | 54.0% |
| 2017/18 | • | - | 78.0% | 75.2% | 80.6% | 69.0% | 57.0% |
| 2018/19 | • | - | 75.0% | 71.9% | 77.8% | 70.0% | 58.0% |
| 2019/20 | • | - | 73.0% | 69.4% | 76.3% | 67.0% | 58.0% |
| 2020/21 | • | - | 70.0% | 65.9% | 73.8% | 65.0% | 58.0% |
Source: NHS England, Adult Social Care and Outcomes Framework
Adults in contact with secondary mental health services who live in stable and appropriate accommodation (Male 18-69 yrs)
|
Period
|
Kingston upon Hull |
Yorkshire and the Humber region (statistical)
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2011/12 | • | - | 54.4% | 50.4% | 58.8% | 54.0% | 53.8% |
| 2012/13 | • | - | 54.0% | 49.8% | 59.2% | 61.0% | 57.3% |
| 2013/14 | • | - | 50.7% | 45.2% | 56.2% | 61.5% | 59.4% |
| 2014/15 | • | - | 65.2% | 59.9% | 70.1% | 65.0% | 58.4% |
| 2015/16 | • | - | 69.5% | 64.9% | 73.7% | 61.8% | 57.4% |
| 2016/17 | • | - | 74.0% | 69.8% | 77.8% | 69.0% | 53.0% |
| 2017/18 | • | - | 75.0% | 70.9% | 78.7% | 66.0% | 56.0% |
| 2018/19 | • | - | 71.0% | 66.5% | 75.1% | 66.0% | 56.0% |
| 2019/20 | • | - | 68.0% | 62.7% | 72.8% | 64.0% | 56.0% |
| 2020/21 | • | - | 63.0% | 57.2% | 68.4% | 62.0% | 56.0% |
Source: NHS England, Adult Social Care and Outcomes Framework
Adults in contact with secondary mental health services who live in stable and appropriate accommodation (Female 18-69 yrs)
|
Period
|
Kingston upon Hull |
Yorkshire and the Humber region (statistical)
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2011/12 | • | - | 69.4% | 65.5% | 73.6% | 56.7% | 55.5% |
| 2012/13 | • | - | 63.4% | 59.4% | 68.1% | 65.2% | 59.8% |
| 2013/14 | • | - | 61.9% | 56.4% | 67.1% | 65.1% | 62.4% |
| 2014/15 | • | - | 72.3% | 67.0% | 77.0% | 69.7% | 61.3% |
| 2015/16 | • | - | 77.9% | 73.4% | 81.9% | 68.0% | 60.0% |
| 2016/17 | • | - | 81.0% | 77.0% | 84.4% | 73.0% | 56.0% |
| 2017/18 | • | - | 80.0% | 76.1% | 83.4% | 72.0% | 59.0% |
| 2018/19 | • | - | 79.0% | 74.7% | 82.7% | 73.0% | 60.0% |
| 2019/20 | • | - | 79.0% | 74.0% | 83.3% | 71.0% | 59.0% |
| 2020/21 | • | - | 78.0% | 72.3% | 82.8% | 69.0% | 59.0% |
Source: NHS England, Adult Social Care and Outcomes Framework
Employment Among Secondary Mental Health Service Users
The inequalities gap in the employment rate among people in contact with secondary mental health services and who are on a Care Plan Approach is high in Hull at 62.2 percentage points. During 2020/21, the overall employment rate was 73.2% (not shown) with an employment rate of 11% for people in contact with secondary mental health services giving an inequalities gap of 62.2 percentage points.
Compared with benchmark
| Indicator | Period | England | Yorkshire and the Humber region (statistical) | Kingston upon Hull | East Riding of Yorkshire | North East Lincolnshire | North Lincolnshire | York | North Yorkshire UA | Barnsley | Doncaster | Rotherham | Sheffield | Bradford | Calderdale | Kirklees | Leeds | Wakefield |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Percentage of people in employment (Persons 16-64 yrs) | 2023/24 | 75.7 | 73.1 | 69.3 | 76.8 | 69.3 | 74.0 | 78.0 | 78.3 | 70.2 | 75.8 | 66.7 | 72.5 | 67.4 | 74.1 | 73.3 | 73.5 | 74.5 |
Gap in the employment rate for those who are in contact with secondary mental health services (aged 18 to 69) and on the Care Plan Approach, and the overall employment rate (Persons 18-69 yrs) | 2020/21 | 66.1 | 62.8 | 62.2 | 55.8 | 60.5 | 68.5 | 56.6 | 56.2 | 62.5 | 67.6 | 68.9 | 63.3 | 62.0 | 63.5 | 59.9 | 69.2 | 66.6 |
The percentage of the population who are in contact with secondary mental health services and on the Care Plan Approach, that are in paid employment (aged 18 to 69) (Persons 18-69 yrs) | 2020/21 | 9.0 | 11.0 | 11.0 | 19.0 | 13.0 | 5.0 | 20.0 | 20.0 | 10.0 | 4.0 | 8.0 | 6.0 | 8.0 | 12.0 | 11.0 | 9.0 | 8.0 |
| Indicator | Period | England | Yorkshire and the Humber region (statistical) | Kingston upon Hull | East Riding of Yorkshire | North East Lincolnshire | North Lincolnshire | York | North Yorkshire UA | Barnsley | Doncaster | Rotherham | Sheffield | Bradford | Calderdale | Kirklees | Leeds | Wakefield |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Percentage of people in employment (Persons 16-64 yrs) | 2023/24 | 75.7 | 73.1 | 69.3 | 76.8 | 69.3 | 74.0 | 78.0 | 78.3 | 70.2 | 75.8 | 66.7 | 72.5 | 67.4 | 74.1 | 73.3 | 73.5 | 74.5 |
Gap in the employment rate for those who are in contact with secondary mental health services (aged 18 to 69) and on the Care Plan Approach, and the overall employment rate (Persons 18-69 yrs) | 2020/21 | 66.1 | 62.8 | 62.2 | 55.8 | 60.5 | 68.5 | 56.6 | 56.2 | 62.5 | 67.6 | 68.9 | 63.3 | 62.0 | 63.5 | 59.9 | 69.2 | 66.6 |
The percentage of the population who are in contact with secondary mental health services and on the Care Plan Approach, that are in paid employment (aged 18 to 69) (Persons 18-69 yrs) | 2020/21 | 9.0 | 11.0 | 11.0 | 19.0 | 13.0 | 5.0 | 20.0 | 20.0 | 10.0 | 4.0 | 8.0 | 6.0 | 8.0 | 12.0 | 11.0 | 9.0 | 8.0 |
The inequalities gap has also been increasing for people in contact with secondary mental health services in relation to employment with the latest year 2020/21 having the highest gap of 62.2 percentage points.
Overall, 56 people aged 18-69 years in contact with secondary mental health services and on the Care Plan Approach in Hull are in paid employment for 2020/21.
Compared with benchmark
Percentage of people in employment (Persons 16-64 yrs)
|
Period
|
Kingston upon Hull |
Yorkshire and the Humber region (statistical)
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2011/12 | • | 104100 | 60.8% | 58.0% | 63.6% | 67.5% | 70.2% |
| 2012/13 | • | 105800 | 62.1% | 59.3% | 64.9% | 69.6% | 71.0% |
| 2013/14 | • | 106300 | 63.1% | 60.1% | 66.1% | 69.9% | 71.7% |
| 2014/15 | • | 109600 | 65.3% | 62.4% | 68.2% | 71.0% | 72.9% |
| 2015/16 | • | 112500 | 66.9% | 63.9% | 69.9% | 72.2% | 73.9% |
| 2016/17 | • | 115600 | 68.8% | 65.5% | 72.1% | 72.8% | 74.4% |
| 2017/18 | • | 118400 | 70.8% | 67.7% | 73.9% | 73.5% | 75.2% |
| 2018/19 | • | 120100 | 71.1% | 67.9% | 74.3% | 73.7% | 75.6% |
| 2019/20 | • | 124700 | 74.0% | 70.5% | 77.5% | 74.0% | 76.2% |
| 2020/21 | • | 123500 | 73.2% | 69.3% | 77.1% | 73.8% | 75.1% |
| 2021/22 | • | 118700 | 70.5% | 66.5% | 74.5% | 74.3% | 75.4% |
| 2022/23 | • | 120800 | 71.5% | 67.1% | 75.9% | 74.4% | 75.7% |
| 2023/24 | • | 117500 | 69.3% | 63.9% | 74.7% | 73.1% | 75.7% |
Source: NOMIS, Official Census and Labour Market Statistics
Gap in the employment rate for those who are in contact with secondary mental health services (aged 18 to 69) and on the Care Plan Approach, and the overall employment rate (Persons 18-69 yrs)
|
Period
|
Kingston upon Hull |
Yorkshire and the Humber region (statistical)
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2011/12 | • | - | 56.0 | 52.9 | 59.1 | 57.9 | 61.3 |
| 2012/13 | • | - | 54.7 | 51.4 | 58.0 | 59.6 | 62.2 |
| 2013/14 | • | - | 58.4 | 55.0 | 61.8 | 62.2 | 64.7 |
| 2014/15 | • | - | 60.3 | 56.9 | 63.7 | 62.6 | 66.1 |
| 2015/16 | • | - | 60.1 | 56.6 | 63.6 | 64.0 | 67.2 |
| 2016/17 | • | - | 59.8 | 56.0 | 63.6 | 63.8 | 67.4 |
| 2017/18 | • | - | 60.8 | 57.1 | 64.5 | 64.5 | 68.2 |
| 2018/19 | • | - | 61.1 | 57.3 | 64.9 | 63.7 | 67.6 |
| 2019/20 | • | - | 61.9 | 57.6 | 66.2 | 63.0 | 67.2 |
| 2020/21 | • | - | 62.2 | 57.5 | 66.9 | 62.8 | 66.1 |
Source: OHID, based on NHS England and Office for National Statistics data
The percentage of the population who are in contact with secondary mental health services and on the Care Plan Approach, that are in paid employment (aged 18 to 69) (Persons 18-69 yrs)
|
Period
|
Kingston upon Hull |
Yorkshire and the Humber region (statistical)
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2017/18 | • | 91 | 10.0% | 8.2% | 12.1% | 9.0% | 7.0% |
| 2018/19 | • | 82 | 10.0% | 8.1% | 12.2% | 10.0% | 8.0% |
| 2019/20 | • | 74 | 12.0% | 9.7% | 14.8% | 11.0% | 9.0% |
| 2020/21 | • | 56 | 11.0% | 8.6% | 14.0% | 11.0% | 9.0% |
Source: OHID, based on NHS England data
Smoking Prevalence Among People with Severe Mental Ill Health
In 2014/15, over half of people in Hull with severe mental illness smoked. Smoking prevalence in the general population in Hull has reduced in Hull from around 23% to 19% so it is possible that the prevalence of smoking could have reduced among people with severe mental illness. However, it is likely that – even if it has reduced slightly – the prevalence of smoking is still very high among people in Hull with severe mental illness and that the prevalence is still much higher in this group compared to the general population.
Compared with benchmark
| Indicator | Period | England | Yorkshire and the Humber region (statistical) | Kingston upon Hull | East Riding of Yorkshire | North East Lincolnshire | North Lincolnshire | York | North Yorkshire UA | Barnsley | Doncaster | Rotherham | Sheffield | Bradford | Calderdale | Kirklees | Leeds | Wakefield |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Smoking prevalence in adults (aged 18 and over) with serious mental illness (SMI) (Persons 18+ yrs) | 2014/15 | 40.5 | 42.3 | 52.3 | 38.0 | 47.8 | 40.8 | 36.7 | 35.1 | 43.7 | 42.8 | 45.0 | 41.2 | 44.6 | - | 42.3 | 42.4 | 42.5 |
| Indicator | Period | England | Yorkshire and the Humber region (statistical) | Kingston upon Hull | East Riding of Yorkshire | North East Lincolnshire | North Lincolnshire | York | North Yorkshire UA | Barnsley | Doncaster | Rotherham | Sheffield | Bradford | Calderdale | Kirklees | Leeds | Wakefield |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Smoking prevalence in adults (aged 18 and over) with serious mental illness (SMI) (Persons 18+ yrs) | 2014/15 | 40.5 | 42.3 | 52.3 | 38.0 | 47.8 | 40.8 | 36.7 | 35.1 | 43.7 | 42.8 | 45.0 | 41.2 | 44.6 | - | 42.3 | 42.4 | 42.5 |
Mortality
Mortality Rates
Whilst severe mental health can shorten life dramatically, many mental health conditions can have a significant impact on daily life and quality of life.
The direct standardised mortality rates per 100,000 population (standardised to the European Standard Population) among 18-74 year olds with severe mental ill health is 79% higher in Hull compared to England for 2021-23 with 198 deaths per 100,000 population in Hull compared to 111 per 100,000 population for England. The mortality rates in Hull are around double those of England for people with severe mental ill health in relation to cardiovascular disease, cancer and respiratory disease, and are around 57% higher for liver disease.
Compared to England, these mortality rates were 79% higher in Hull for all causes, 99% higher for cardiovascular disease, 89% higher for cancer, 57% higher for liver disease and 104% higher for respiratory disease (more than double).
Severe mental ill health is defined as having a referral to secondary mental health services in the five years preceding death (excluding learning disabilities and autism).
The rates are given out of all the population of Hull aged 18-74 years (not just those with severe mental illness).,
Compared with benchmark
| Indicator | Period | England | Yorkshire and the Humber region (statistical) | Kingston upon Hull | East Riding of Yorkshire | North East Lincolnshire | North Lincolnshire | York | North Yorkshire UA | Barnsley | Doncaster | Rotherham | Sheffield | Bradford | Calderdale | Kirklees | Leeds | Wakefield |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Premature mortality in adults with severe mental illness (SMI) (Persons 18-74 yrs) | 2021 - 23 | 110.8 | 120.5 | 198.4 | 86.5 | 156.7 | 103.8 | 113.5 | 92.7 | 154.2 | 140.8 | 143.0 | 115.9 | 117.2 | 117.3 | 120.9 | 126.0 | 110.1 |
Premature mortality due to cardiovascular diseases in adults with severe mental illness (SMI) (Persons 18-74 yrs) | 2021 - 23 | 20.4 | 22.5 | 40.5 | 17.3 | 34.9 | 22.0 | 17.5 | 15.5 | 29.6 | 25.5 | 30.9 | 20.4 | 25.7 | 21.0 | 26.1 | 19.5 | 16.4 |
Premature mortality due to cancer in adults with severe mental illness (SMI) (Persons 18-74 yrs) | 2021 - 23 | 20.5 | 21.4 | 38.8 | 15.3 | 27.3 | 19.4 | 23.4 | 15.7 | 27.9 | 24.5 | 24.1 | 19.9 | 17.2 | 18.5 | 20.0 | 26.9 | 17.6 |
Premature mortality due to liver disease in adults with severe mental illness (SMI) (Persons 18-74 yrs) | 2021 - 23 | 8.9 | 9.8 | 14.0 | 6.1 | 14.7 | 11.5 | 12.6 | 9.6 | 11.2 | 16.4 | 12.4 | 9.0 | 7.1 | 7.1 | 10.1 | 7.7 | 8.9 |
Premature mortality due to respiratory disease in adults with severe mental illness (SMI) (Persons 18-74 yrs) | 2021 - 23 | 11.1 | 12.0 | 22.6 | 6.2 | 18.2 | 11.0 | 10.3 | 7.2 | 14.0 | 13.4 | 17.5 | 10.9 | 13.0 | 11.1 | 13.1 | 13.8 | 9.3 |
| Indicator | Period | England | Yorkshire and the Humber region (statistical) | Kingston upon Hull | East Riding of Yorkshire | North East Lincolnshire | North Lincolnshire | York | North Yorkshire UA | Barnsley | Doncaster | Rotherham | Sheffield | Bradford | Calderdale | Kirklees | Leeds | Wakefield |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Premature mortality in adults with severe mental illness (SMI) (Persons 18-74 yrs) | 2021 - 23 | 110.8 | 120.5 | 198.4 | 86.5 | 156.7 | 103.8 | 113.5 | 92.7 | 154.2 | 140.8 | 143.0 | 115.9 | 117.2 | 117.3 | 120.9 | 126.0 | 110.1 |
Premature mortality due to cardiovascular diseases in adults with severe mental illness (SMI) (Persons 18-74 yrs) | 2021 - 23 | 20.4 | 22.5 | 40.5 | 17.3 | 34.9 | 22.0 | 17.5 | 15.5 | 29.6 | 25.5 | 30.9 | 20.4 | 25.7 | 21.0 | 26.1 | 19.5 | 16.4 |
Premature mortality due to cancer in adults with severe mental illness (SMI) (Persons 18-74 yrs) | 2021 - 23 | 20.5 | 21.4 | 38.8 | 15.3 | 27.3 | 19.4 | 23.4 | 15.7 | 27.9 | 24.5 | 24.1 | 19.9 | 17.2 | 18.5 | 20.0 | 26.9 | 17.6 |
Premature mortality due to liver disease in adults with severe mental illness (SMI) (Persons 18-74 yrs) | 2021 - 23 | 8.9 | 9.8 | 14.0 | 6.1 | 14.7 | 11.5 | 12.6 | 9.6 | 11.2 | 16.4 | 12.4 | 9.0 | 7.1 | 7.1 | 10.1 | 7.7 | 8.9 |
Premature mortality due to respiratory disease in adults with severe mental illness (SMI) (Persons 18-74 yrs) | 2021 - 23 | 11.1 | 12.0 | 22.6 | 6.2 | 18.2 | 11.0 | 10.3 | 7.2 | 14.0 | 13.4 | 17.5 | 10.9 | 13.0 | 11.1 | 13.1 | 13.8 | 9.3 |
The premature mortality rate among people with severe mental ill health has been increasing over time for both Hull and England (by around one-fifth between 2015-17 and 2021-23 for both Hull and England). As the indicator examines mortality rate among people who have had contact with secondary mental health services in the last five years preceding death, it is possible that changes over time to the way services are run and access to services could influence the rate. It is possible that this could explain the increases over time, although it is also possible that the severity of mental ill health of service users could have increased over time.
Overall, there were 3,314 deaths among people aged under 75 years registered during the three year period 2021 to 2023. There around 60 deaths among infants (aged under one year) and children aged 1-17 years so around 3,250 deaths among those aged 18-74 years.
There were 1,035 Hull residents aged 18-74 years who died prematurely who had contact with secondary mental health services in the five years preceding death whose deaths were registered during the three years 2021 to 2023.
So around one-third of all deaths among those aged 18-74 years in Hull registered during 2021 to 2023 have been in contact with secondary mental health services. The overall mortality rate is around 500 per 100,000 population, and the mortality rate for people in contact with secondary mental health services is just under 200 per 100,000 population, although the latter is out of all population and not the population who have been in contact with secondary mental health services so will be lower.
Compared with benchmark
Under 75 mortality rate from all causes (Persons <75 yrs)
|
Period
|
Kingston upon Hull |
Yorkshire and the Humber region (statistical)
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2001 - 03 | • | 3080 | 562.4 | 542.6 | 582.8 | 475.9 | 452.2 |
| 2002 - 04 | • | 3066 | 559.2 | 539.4 | 579.5 | 462.5 | 439.2 |
| 2003 - 05 | • | 3074 | 557.4 | 537.6 | 577.6 | 448.7 | 425.8 |
| 2004 - 06 | • | 3050 | 551.4 | 531.8 | 571.5 | 436.1 | 411.6 |
| 2005 - 07 | • | 3002 | 541.7 | 522.2 | 561.6 | 427.3 | 400.6 |
| 2006 - 08 | • | 2986 | 541.2 | 521.8 | 561.2 | 420.4 | 391.3 |
| 2007 - 09 | • | 2943 | 533.1 | 513.7 | 552.9 | 410.2 | 380.3 |
| 2008 - 10 | • | 2875 | 518.4 | 499.4 | 538.0 | 400.1 | 370.5 |
| 2009 - 11 | • | 2792 | 501.6 | 482.9 | 520.8 | 389.7 | 358.9 |
| 2010 - 12 | • | 2660 | 475.5 | 457.4 | 494.2 | 381.2 | 350.0 |
| 2011 - 13 | • | 2625 | 464.2 | 446.4 | 482.6 | 373.3 | 342.5 |
| 2012 - 14 | • | 2647 | 463.1 | 445.3 | 481.3 | 365.8 | 337.2 |
| 2013 - 15 | • | 2731 | 472.3 | 454.4 | 490.6 | 363.0 | 335.2 |
| 2014 - 16 | • | 2804 | 476.6 | 458.8 | 494.9 | 362.5 | 334.3 |
| 2015 - 17 | • | 2888 | 477.8 | 460.3 | 495.8 | 362.8 | 332.6 |
| 2016 - 18 | • | 2861 | 462.3 | 445.4 | 479.7 | 363.9 | 331.3 |
| 2017 - 19 | • | 2932 | 465.6 | 448.8 | 482.9 | 362.0 | 327.0 |
| 2018 - 20 | • | 3010 | 471.3 | 454.6 | 488.6 | 373.7 | 337.7 |
| 2019 - 21 | • | 3252 | 501.6 | 484.4 | 519.2 | 383.3 | 348.6 |
| 2020 - 22 | • | 3359 | 515.6 | 498.2 | 533.4 | 392.1 | 355.3 |
| 2021 - 23 | • | 3314 | 507.4 | 490.2 | 525.0 | 386.1 | 349.1 |
Source: OHID, based on Office for National Statistics data
Premature mortality in adults with severe mental illness (SMI) (Persons 18-74 yrs)
|
Period
|
Kingston upon Hull |
Yorkshire and the Humber region (statistical)
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2015 - 17 | • | 800 | 163.2 | 152.0 | 175.1 | 96.4 | 90.7 |
| 2016 - 18 | • | 820 | 164.1 | 153.0 | 175.8 | 99.8 | 94.9 |
| 2017 - 19 | • | 875 | 172.7 | 161.4 | 184.6 | 103.9 | 97.8 |
| 2018 - 20 | • | 890 | 173.4 | 162.1 | 185.2 | 109.0 | 103.6 |
| 2019 - 21 | • | 975 | 188.0 | 176.3 | 200.2 | 114.5 | 108.0 |
| 2020 - 22 | • | 1040 | 199.1 | 187.1 | 211.6 | 119.0 | 111.2 |
| 2021 - 23 | • | 1035 | 198.4 | 186.4 | 210.9 | 120.5 | 110.8 |
Source: NHS England and Office for National Statistics
Whilst there has been a slight increase in the premature mortality rate from cardiovascular diseases for people with severe mental ill health over time for England, the increase is relatively small increasing by 14% from 17.9 to 20.4 deaths per 100,000 population between 2015-17 and 2021-23. In contrast, the increase for Hull has been much greater increasing by 28% from 31.7 to 40.5 deaths per 100,000 population over the same time period.
There were 210 Hull residents aged 18-74 years who died prematurely from cardiovascular diseases who had contact with secondary mental health services in the five years preceding death whose deaths were registered during the three years 2021 to 2023. There were 774 premature cardiovascular disease deaths in total (most would have been among those aged 18-74 years) so over a quarter had been in contact with secondary mental health services in the five years prior to death.
Compared with benchmark
Under 75 mortality rate from cardiovascular disease (Persons <75 yrs)
|
Period
|
Kingston upon Hull |
Yorkshire and the Humber region (statistical)
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2001 - 03 | • | 941 | 176.4 | 165.3 | 188.1 | 147.6 | 138.0 |
| 2002 - 04 | • | 892 | 167.4 | 156.6 | 178.8 | 136.3 | 129.5 |
| 2003 - 05 | • | 849 | 159.7 | 149.1 | 170.9 | 127.7 | 120.9 |
| 2004 - 06 | • | 811 | 152.7 | 142.3 | 163.6 | 120.4 | 112.3 |
| 2005 - 07 | • | 762 | 142.9 | 132.9 | 153.5 | 113.9 | 105.1 |
| 2006 - 08 | • | 743 | 139.8 | 129.9 | 150.3 | 109.3 | 99.0 |
| 2007 - 09 | • | 705 | 132.1 | 122.4 | 142.3 | 103.0 | 93.1 |
| 2008 - 10 | • | 690 | 128.9 | 119.4 | 139.0 | 99.4 | 88.6 |
| 2009 - 11 | • | 639 | 118.0 | 108.9 | 127.6 | 94.3 | 84.0 |
| 2010 - 12 | • | 584 | 107.1 | 98.5 | 116.2 | 91.0 | 80.8 |
| 2011 - 13 | • | 564 | 102.1 | 93.7 | 110.9 | 86.9 | 77.8 |
| 2012 - 14 | • | 587 | 105.2 | 96.8 | 114.2 | 84.7 | 75.8 |
| 2013 - 15 | • | 603 | 106.8 | 98.3 | 115.7 | 83.6 | 74.7 |
| 2014 - 16 | • | 618 | 107.6 | 99.2 | 116.6 | 83.4 | 73.6 |
| 2015 - 17 | • | 621 | 104.9 | 96.8 | 113.6 | 82.7 | 72.7 |
| 2016 - 18 | • | 639 | 105.0 | 96.9 | 113.5 | 82.2 | 71.9 |
| 2017 - 19 | • | 659 | 106.0 | 98.0 | 114.4 | 80.4 | 70.7 |
| 2018 - 20 | • | 685 | 108.3 | 100.4 | 116.8 | 80.4 | 71.7 |
| 2019 - 21 | • | 713 | 111.3 | 103.3 | 119.8 | 82.2 | 73.1 |
| 2020 - 22 | • | 760 | 118.3 | 110.0 | 127.0 | 86.4 | 76.0 |
| 2021 - 23 | • | 774 | 119.8 | 111.5 | 128.6 | 88.1 | 77.1 |
Source: OHID, based on Office for National Statistics data
Premature mortality due to cardiovascular diseases in adults with severe mental illness (SMI) (Persons 18-74 yrs)
|
Period
|
Kingston upon Hull |
Yorkshire and the Humber region (statistical)
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2015 - 17 | • | 155 | 31.7 | 26.8 | 37.2 | 20.0 | 17.9 |
| 2016 - 18 | • | 165 | 33.4 | 28.4 | 38.9 | 20.2 | 18.4 |
| 2017 - 19 | • | 175 | 34.5 | 29.5 | 40.1 | 19.8 | 18.7 |
| 2018 - 20 | • | 190 | 37.1 | 32.0 | 42.8 | 19.8 | 18.9 |
| 2019 - 21 | • | 200 | 38.6 | 33.4 | 44.4 | 20.6 | 19.2 |
| 2020 - 22 | • | 215 | 41.8 | 36.4 | 47.8 | 21.8 | 19.9 |
| 2021 - 23 | • | 210 | 40.5 | 35.2 | 46.4 | 22.5 | 20.4 |
Source: NHS England and Office for National Statistics
There has been some year-on-year variability in the premature mortality rate from cancer among Hull residents who had severe mental ill health, but the mortality rate has consistently been higher than England throughout the entire period 2015-17 to 2021-23, and has increased in Hull over the last three years. Whilst there has been a very small increase in England over the last three years (from 20.3 to 20.5 deaths per 100,000 population) the increase in Hull has been greater (increasing from 31.5 to 38.8 per 100,000 population).
There were 200 Hull residents who died prematurely from cancer who had contact with secondary mental health services in the five years preceding death whose deaths were registered during the three years 2021 to 2023. There were 1,037 premature cancer disease deaths in total (most would have been among those aged 18-74 years) so just under one-fifth had been in contact with secondary mental health services in the five years prior to death.
Compared with benchmark
Under 75 mortality rate from cancer (Persons <75 yrs)
|
Period
|
Kingston upon Hull |
Yorkshire and the Humber region (statistical)
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2001 - 03 | • | 1095 | 206.2 | 194.1 | 218.8 | 178.7 | 169.4 |
| 2002 - 04 | • | 1107 | 207.7 | 195.6 | 220.4 | 176.3 | 166.2 |
| 2003 - 05 | • | 1071 | 200.4 | 188.5 | 212.9 | 170.6 | 162.7 |
| 2004 - 06 | • | 1088 | 203.6 | 191.6 | 216.2 | 167.0 | 160.0 |
| 2005 - 07 | • | 1065 | 199.5 | 187.7 | 212.0 | 165.2 | 157.8 |
| 2006 - 08 | • | 1089 | 204.7 | 192.6 | 217.3 | 164.2 | 155.7 |
| 2007 - 09 | • | 1081 | 202.9 | 190.9 | 215.5 | 161.6 | 153.2 |
| 2008 - 10 | • | 1064 | 198.5 | 186.7 | 210.9 | 159.1 | 150.6 |
| 2009 - 11 | • | 1062 | 197.2 | 185.4 | 209.6 | 158.3 | 148.5 |
| 2010 - 12 | • | 1046 | 192.6 | 181.0 | 204.8 | 157.4 | 146.5 |
| 2011 - 13 | • | 1058 | 191.7 | 180.2 | 203.8 | 155.0 | 144.4 |
| 2012 - 14 | • | 1043 | 186.2 | 175.0 | 198.0 | 151.7 | 141.6 |
| 2013 - 15 | • | 1063 | 187.9 | 176.6 | 199.6 | 148.5 | 138.9 |
| 2014 - 16 | • | 1031 | 179.4 | 168.5 | 190.8 | 146.4 | 137.1 |
| 2015 - 17 | • | 1053 | 179.5 | 168.7 | 190.8 | 143.7 | 134.9 |
| 2016 - 18 | • | 963 | 159.9 | 149.9 | 170.4 | 141.4 | 132.7 |
| 2017 - 19 | • | 988 | 160.8 | 150.9 | 171.2 | 137.9 | 129.7 |
| 2018 - 20 | • | 979 | 156.2 | 146.5 | 166.3 | 136.0 | 127.6 |
| 2019 - 21 | • | 1062 | 166.7 | 156.8 | 177.0 | 133.5 | 124.8 |
| 2020 - 22 | • | 1062 | 165.4 | 155.5 | 175.6 | 132.4 | 123.2 |
| 2021 - 23 | • | 1037 | 161.3 | 151.6 | 171.5 | 130.1 | 121.6 |
Source: OHID, based on Office for National Statistics data
Premature mortality due to cancer in adults with severe mental illness (SMI) (Persons 18-74 yrs)
|
Period
|
Kingston upon Hull |
Yorkshire and the Humber region (statistical)
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2015 - 17 | • | 170 | 36.4 | 31.1 | 42.4 | 19.1 | 18.6 |
| 2016 - 18 | • | 155 | 32.6 | 27.7 | 38.1 | 19.1 | 19.4 |
| 2017 - 19 | • | 170 | 34.5 | 29.5 | 40.1 | 19.3 | 20.2 |
| 2018 - 20 | • | 160 | 31.5 | 26.8 | 36.9 | 18.8 | 20.3 |
| 2019 - 21 | • | 180 | 35.9 | 30.9 | 41.5 | 19.5 | 20.3 |
| 2020 - 22 | • | 195 | 37.7 | 32.6 | 43.4 | 20.4 | 20.2 |
| 2021 - 23 | • | 200 | 38.8 | 33.6 | 44.6 | 21.4 | 20.5 |
Source: NHS England and Office for National Statistics
The premature mortality rate from liver disease among people with severe mental ill health has been consistently higher in Hull compared to England. The rate in England has gradually increased by 29% from 6.9 to 8.9 deaths per 100,000 population between 2015-17 and 2021-23. The increase in Hull over the same period has been slightly smaller, increasing by 22% from 11.5 to 14.0 deaths per 100,000 population although the majority of the increase in Hull has been in the last three years.
There were 70 Hull residents who died prematurely from liver disease who had contact with secondary mental health services in the five years preceding death whose deaths were registered during the three years 2021 to 2023. There were 174 premature liver disease deaths in total (all of them would have been among those aged 18-74 years) so around four in ten had been in contact with secondary mental health services in the five years prior to death.
Compared with benchmark
Under 75 mortality rate from liver disease (Persons <75 yrs)
|
Period
|
Kingston upon Hull |
Yorkshire and the Humber region (statistical)
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2001 - 03 | • | 85 | 15.1 | 12.1 | 18.7 | 14.7 | 16.1 |
| 2002 - 04 | • | 109 | 19.3 | 15.8 | 23.3 | 15.8 | 16.7 |
| 2003 - 05 | • | 134 | 23.4 | 19.6 | 27.8 | 16.9 | 17.0 |
| 2004 - 06 | • | 135 | 23.4 | 19.6 | 27.8 | 17.8 | 17.4 |
| 2005 - 07 | • | 145 | 25.1 | 21.1 | 29.6 | 18.0 | 17.8 |
| 2006 - 08 | • | 125 | 21.3 | 17.7 | 25.4 | 17.9 | 18.2 |
| 2007 - 09 | • | 135 | 23.0 | 19.2 | 27.2 | 17.9 | 18.2 |
| 2008 - 10 | • | 133 | 22.6 | 18.9 | 26.8 | 17.9 | 18.2 |
| 2009 - 11 | • | 148 | 25.2 | 21.3 | 29.6 | 19.1 | 18.3 |
| 2010 - 12 | • | 145 | 24.4 | 20.6 | 28.8 | 19.2 | 18.3 |
| 2011 - 13 | • | 142 | 23.5 | 19.8 | 27.8 | 19.2 | 18.2 |
| 2012 - 14 | • | 142 | 23.3 | 19.6 | 27.5 | 18.4 | 18.1 |
| 2013 - 15 | • | 134 | 22.1 | 18.5 | 26.2 | 18.2 | 18.3 |
| 2014 - 16 | • | 138 | 22.4 | 18.8 | 26.5 | 18.4 | 18.5 |
| 2015 - 17 | • | 141 | 22.4 | 18.9 | 26.5 | 19.4 | 18.8 |
| 2016 - 18 | • | 143 | 22.3 | 18.8 | 26.3 | 19.3 | 18.8 |
| 2017 - 19 | • | 142 | 21.9 | 18.4 | 25.8 | 20.2 | 18.8 |
| 2018 - 20 | • | 148 | 22.8 | 19.3 | 26.8 | 20.4 | 19.3 |
| 2019 - 21 | • | 151 | 23.3 | 19.8 | 27.4 | 22.0 | 20.2 |
| 2020 - 22 | • | 164 | 25.1 | 21.4 | 29.2 | 22.5 | 21.1 |
| 2021 - 23 | • | 174 | 26.6 | 22.8 | 30.9 | 22.9 | 21.5 |
Source: OHID, based on Office for National Statistics data
Premature mortality due to liver disease in adults with severe mental illness (SMI) (Persons 18-74 yrs)
|
Period
|
Kingston upon Hull |
Yorkshire and the Humber region (statistical)
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2015 - 17 | • | 60 | 11.5 | 8.7 | 14.8 | 7.0 | 6.9 |
| 2016 - 18 | • | 55 | 10.9 | 8.3 | 14.2 | 7.1 | 7.0 |
| 2017 - 19 | • | 60 | 11.1 | 8.4 | 14.3 | 7.7 | 7.2 |
| 2018 - 20 | • | 55 | 10.8 | 8.1 | 14.0 | 8.2 | 7.6 |
| 2019 - 21 | • | 65 | 12.1 | 9.3 | 15.5 | 8.9 | 8.1 |
| 2020 - 22 | • | 65 | 13.0 | 10.1 | 16.6 | 9.5 | 8.7 |
| 2021 - 23 | • | 70 | 14.0 | 10.9 | 17.6 | 9.8 | 8.9 |
Source: NHS England and Office for National Statistics
The premature mortality rate from respiratory disease among adults (aged 18-74 years) with severe mental ill health has been quite variable between 2015-17 and 2021-23. However, it is relatively difficult to interpret the trend over time as it could well have been impacted by the COVID-19 pandemic. In the overall population, there was a decrease in the mortality rate from respiratory disease as there was increased mortality from COVID-19 among the people who were at an increased risk of mortality from respiratory disease. So instead of dying from respiratory disease, some died from COVID-19 which meant that the mortality rates from respiratory disease were lower during the pandemic (COVID-19 does not fall into the respiratory disease category). The premature mortality rate from respiratory disease among adults (aged 18-74 years) with severe mental ill health did also decrease during the pandemic although the mortality rate has increased between 2020-22 and 2021-23 (mortality rates were highest from COVID-19 during 2020). There was also a slight reduction in the premature respiratory mortality rate for England during the pandemic but it was not as obvious as the decrease in Hull.
There were 115 Hull residents who died prematurely from respiratory disease who had contact with secondary mental health services in the five years preceding death whose deaths were registered during the three years 2021 to 2023. There were 342 premature respiratory disease deaths in total (all of them would have been among those aged 18-74 years) so around one-third ad been in contact with secondary mental health services in the five years prior to death.
Compared with benchmark
Under 75 mortality rate from respiratory disease (Persons <75 yrs)
|
Period
|
Kingston upon Hull |
Yorkshire and the Humber region (statistical)
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2001 - 03 | • | 317 | 60.5 | 54.0 | 67.6 | 44.9 | 39.9 |
| 2002 - 04 | • | 314 | 59.8 | 53.3 | 66.8 | 44.5 | 39.2 |
| 2003 - 05 | • | 300 | 57.4 | 51.1 | 64.3 | 43.8 | 38.8 |
| 2004 - 06 | • | 269 | 51.2 | 45.3 | 57.7 | 41.5 | 37.0 |
| 2005 - 07 | • | 273 | 52.1 | 46.0 | 58.6 | 41.4 | 36.5 |
| 2006 - 08 | • | 296 | 56.3 | 50.0 | 63.1 | 41.2 | 36.0 |
| 2007 - 09 | • | 324 | 61.7 | 55.1 | 68.8 | 41.9 | 35.4 |
| 2008 - 10 | • | 325 | 61.9 | 55.3 | 69.0 | 41.1 | 34.8 |
| 2009 - 11 | • | 328 | 62.8 | 56.2 | 70.1 | 40.2 | 33.7 |
| 2010 - 12 | • | 316 | 60.8 | 54.3 | 68.0 | 38.8 | 33.0 |
| 2011 - 13 | • | 317 | 60.0 | 53.5 | 67.0 | 38.7 | 32.7 |
| 2012 - 14 | • | 323 | 60.1 | 53.6 | 67.1 | 38.0 | 32.1 |
| 2013 - 15 | • | 338 | 61.2 | 54.8 | 68.2 | 37.9 | 32.6 |
| 2014 - 16 | • | 357 | 63.9 | 57.4 | 71.0 | 38.5 | 33.3 |
| 2015 - 17 | • | 362 | 63.2 | 56.8 | 70.1 | 39.2 | 33.8 |
| 2016 - 18 | • | 384 | 65.5 | 59.1 | 72.5 | 40.7 | 34.3 |
| 2017 - 19 | • | 401 | 66.5 | 60.1 | 73.3 | 40.7 | 33.8 |
| 2018 - 20 | • | 372 | 60.3 | 54.3 | 66.7 | 38.9 | 32.6 |
| 2019 - 21 | • | 338 | 53.6 | 48.1 | 59.7 | 35.5 | 29.8 |
| 2020 - 22 | • | 321 | 50.5 | 45.1 | 56.4 | 33.9 | 28.9 |
| 2021 - 23 | • | 342 | 53.9 | 48.3 | 59.9 | 35.9 | 30.3 |
Source: OHID, based on Office for National Statistics data
Premature mortality due to respiratory disease in adults with severe mental illness (SMI) (Persons 18-74 yrs)
|
Period
|
Kingston upon Hull |
Yorkshire and the Humber region (statistical)
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2015 - 17 | • | 105 | 22.2 | 18.1 | 27.0 | 11.7 | 11.5 |
| 2016 - 18 | • | 105 | 22.2 | 18.1 | 26.9 | 12.9 | 12.1 |
| 2017 - 19 | • | 120 | 24.5 | 20.3 | 29.4 | 13.7 | 12.4 |
| 2018 - 20 | • | 110 | 22.1 | 18.1 | 26.6 | 13.3 | 12.2 |
| 2019 - 21 | • | 100 | 19.5 | 15.8 | 23.7 | 12.0 | 11.1 |
| 2020 - 22 | • | 100 | 19.8 | 16.1 | 24.1 | 11.3 | 10.6 |
| 2021 - 23 | • | 115 | 22.6 | 18.6 | 27.1 | 12.0 | 11.1 |
Source: NHS England and Office for National Statistics
Percentage Excess Mortality Rate
Despite very high levels of premature mortality among people with severe mental ill health in Hull compared to England, the excess premature mortality rate for people with severe mental ill health is lower than England when expressed as the percentage increased risk due to severe mental ill health compared to those without severe mental ill health. This is likely because there is a much higher rate of premature mortality in Hull compared to England in the overall population, so that the differential in the premature mortality rate between people with and without severe mental ill health is smaller in Hull.
As for premature mortality, severe mental ill health is defined as having a referral to secondary mental health services in the five years preceding death (excluding learning disabilities and autism).
In Hull, people with severe mental illness had a premature mortality rate that was 159% higher (more than double) than the mortality rate of people without severe mental ill health for deaths registered during 2021-23, but people in England had a mortality rate that was 384% higher (almost four times higher).
Compared to the Hull’s population, people in Hull with severe mental illness had premature mortality rates from cardiovascular disease that were 114% higher, 50% higher for cancer, 256% higher for liver disease and 227% higher for respiratory disease.
Hull’s values are statistically significantly lower and ‘better’ than England. Strictly speaking, it is better that the differential in premature mortality rates between people with and without severe mental ill health is lower, however, it does not portray the full picture of mortality as illustrated above. Whilst all these (relative) percentages were lower in Hull compared to England, the absolute mortality rates among people with severe mental ill health was statistically significantly higher in Hull as illustrated above (around double that of England).
Compared with benchmark
| Indicator | Period | England | Yorkshire and the Humber region (statistical) | Kingston upon Hull | East Riding of Yorkshire | North East Lincolnshire | North Lincolnshire | York | North Yorkshire UA | Barnsley | Doncaster | Rotherham | Sheffield | Bradford | Calderdale | Kirklees | Leeds | Wakefield |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Excess under 75 mortality rate in adults with severe mental illness (SMI) (Persons 18-74 yrs) | 2021 - 23 | 383.7 | 335.7 | 158.6 | 325.5 | 350.1 | 314.7 | 478.8 | 429.2 | 300.6 | 429.7 | 404.9 | 374.3 | 266.8 | 344.3 | 317.4 | 337.5 | 319.5 |
Excess under 75 mortality rate due to cardiovascular disease in adults with severe mental illness (SMI) (Persons 18-74 yrs) | 2021 - 23 | 290.3 | 244.0 | 113.7 | 266.9 | 316.0 | 224.3 | 336.3 | 303.5 | 225.7 | 318.2 | 343.5 | 271.0 | 195.8 | 238.9 | 254.1 | 199.6 | 187.9 |
Excess under 75 mortality rate due to cancer in adults with severe mental illness (SMI) (Persons 18-74 yrs) | 2021 - 23 | 129.5 | 109.1 | 50.4 | 101.5 | 90.0 | 115.5 | 175.9 | 123.3 | 112.2 | 135.3 | 135.5 | 111.3 | 61.2 | 104.7 | 96.1 | 140.3 | 91.0 |
Excess under 75 mortality rate due to liver disease in adults with severe mental illness (SMI) (Persons 18-74 yrs) | 2021 - 23 | 555.9 | 519.4 | 255.5 | 528.2 | 741.7 | 536.4 | 1445.1 | 948.2 | 356.8 | 1133.3 | 612.8 | 647.3 | 306.1 | 263.4 | 540.4 | 350.5 | 374.2 |
Excess under 75 mortality rate due to respiratory disease in adults with severe mental illness (SMI) (Persons 18-74 yrs) | 2021 - 23 | 519.7 | 410.8 | 227.0 | 328.5 | 491.1 | 490.5 | 690.9 | 524.2 | 360.3 | 471.2 | 531.3 | 459.8 | 323.8 | 372.6 | 381.0 | 430.4 | 256.4 |
| Indicator | Period | England | Yorkshire and the Humber region (statistical) | Kingston upon Hull | East Riding of Yorkshire | North East Lincolnshire | North Lincolnshire | York | North Yorkshire UA | Barnsley | Doncaster | Rotherham | Sheffield | Bradford | Calderdale | Kirklees | Leeds | Wakefield |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Excess under 75 mortality rate in adults with severe mental illness (SMI) (Persons 18-74 yrs) | 2021 - 23 | 383.7 | 335.7 | 158.6 | 325.5 | 350.1 | 314.7 | 478.8 | 429.2 | 300.6 | 429.7 | 404.9 | 374.3 | 266.8 | 344.3 | 317.4 | 337.5 | 319.5 |
Excess under 75 mortality rate due to cardiovascular disease in adults with severe mental illness (SMI) (Persons 18-74 yrs) | 2021 - 23 | 290.3 | 244.0 | 113.7 | 266.9 | 316.0 | 224.3 | 336.3 | 303.5 | 225.7 | 318.2 | 343.5 | 271.0 | 195.8 | 238.9 | 254.1 | 199.6 | 187.9 |
Excess under 75 mortality rate due to cancer in adults with severe mental illness (SMI) (Persons 18-74 yrs) | 2021 - 23 | 129.5 | 109.1 | 50.4 | 101.5 | 90.0 | 115.5 | 175.9 | 123.3 | 112.2 | 135.3 | 135.5 | 111.3 | 61.2 | 104.7 | 96.1 | 140.3 | 91.0 |
Excess under 75 mortality rate due to liver disease in adults with severe mental illness (SMI) (Persons 18-74 yrs) | 2021 - 23 | 555.9 | 519.4 | 255.5 | 528.2 | 741.7 | 536.4 | 1445.1 | 948.2 | 356.8 | 1133.3 | 612.8 | 647.3 | 306.1 | 263.4 | 540.4 | 350.5 | 374.2 |
Excess under 75 mortality rate due to respiratory disease in adults with severe mental illness (SMI) (Persons 18-74 yrs) | 2021 - 23 | 519.7 | 410.8 | 227.0 | 328.5 | 491.1 | 490.5 | 690.9 | 524.2 | 360.3 | 471.2 | 531.3 | 459.8 | 323.8 | 372.6 | 381.0 | 430.4 | 256.4 |
The excess premature mortality rate among Hull adults with severe mental ill health has remained relatively constant between 2015-17 and 2021-23 with premature mortality rates between 160% and 170% higher among people aged 18-74 years with severe mental ill health compared to all people aged 18-74 years.
The premature mortality rate among Hull adults with severe mental ill health has increased in Hull over this period as illustrated above, but as the difference between the overall population and those with severe mental ill health has remained relatively constant, this must mean that the overall premature mortality rate for all people has increased in Hull (which it has since 2015-17 as illustrated above – although some of this increase may be associated with the COVID-19 pandemic).
Excess premature mortality for England has shown a slight increase over the same time period increasing from 350% higher to almost 390% higher among people with severe mental ill health compared to people without severe mental ill health.
Compared with benchmark
Excess under 75 mortality rate in adults with severe mental illness (SMI) (Persons 18-74 yrs)
|
Period
|
Kingston upon Hull |
Yorkshire and the Humber region (statistical)
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2015 - 17 | • | - | 170.7% | 148.2% | 195.2% | 331.2% | 350.6% |
| 2016 - 18 | • | - | 167.7% | 145.7% | 191.6% | 330.6% | 359.7% |
| 2017 - 19 | • | - | 172.7% | 150.9% | 196.4% | 341.8% | 377.0% |
| 2018 - 20 | • | - | 159.3% | 138.8% | 181.5% | 337.7% | 383.5% |
| 2019 - 21 | • | - | 155.9% | 136.6% | 176.9% | 338.1% | 385.9% |
| 2020 - 22 | • | - | 159.9% | 140.7% | 180.7% | 334.7% | 385.9% |
| 2021 - 23 | • | - | 158.6% | 139.4% | 179.3% | 335.7% | 383.7% |
Source: NHS England and Office for National Statistics
The excess premature mortality rate for cardiovascular disease for people aged 18-74 years with severe mental ill health when compared to people without severe mental ill health has reduced slightly in Hull over time from being 134% higher for 2015-17 to being 114% higher for 2021-23. However, as illustrated above, the premature mortality rate from cardiovascular diseases for people with severe mental ill health has increased by just under one-third in Hull over the same period. However, the premature cardiovascular mortality rate for all people has also increased over this period (by more than the increase among those in contact with secondary mental health services).
Compared with benchmark
Excess under 75 mortality rate due to cardiovascular disease in adults with severe mental illness (SMI) (Persons 18-74 yrs)
|
Period
|
Kingston upon Hull |
Yorkshire and the Humber region (statistical)
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2015 - 17 | • | - | 134.0% | 93.3% | 183.4% | 288.0% | 296.3% |
| 2016 - 18 | • | - | 134.9% | 95.2% | 182.7% | 282.2% | 300.8% |
| 2017 - 19 | • | - | 132.1% | 93.8% | 177.9% | 271.6% | 309.8% |
| 2018 - 20 | • | - | 135.8% | 98.2% | 180.6% | 261.5% | 301.0% |
| 2019 - 21 | • | - | 133.0% | 96.7% | 176.0% | 258.7% | 298.7% |
| 2020 - 22 | • | - | 131.6% | 96.7% | 172.6% | 253.2% | 292.2% |
| 2021 - 23 | • | - | 113.7% | 81.3% | 151.9% | 244.0% | 290.3% |
Source: NHS England and Office for National Statistics
The excess premature mortality rate from cancer for people aged 18-74 years with severe mental ill health compared to people without severe mental ill health has been relatively variable but has been about 40% although this did reduce during the COVID-19 pandemic. The percentage increased in the last year and was 50% for 2021-23.
Premature cancer rates for all people have decreased slightly (ignoring over the pandemic when it was much lower) but has increased marginally among people with severe mental ill health as illustrated above (between 2016-18 and 2021-23). So this has resulted in an increase in the relative difference between people without severe mental ill health and those with severe mental ill health (between 2016-18 to 2021-23).
Compared with benchmark
Excess under 75 mortality rate due to cancer in adults with severe mental illness (SMI) (Persons 18-74 yrs)
|
Period
|
Kingston upon Hull |
Yorkshire and the Humber region (statistical)
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2015 - 17 | • | - | 49.6% | 26.2% | 77.5% | 95.2% | 105.1% |
| 2016 - 18 | • | - | 41.7% | 18.7% | 69.1% | 91.4% | 109.7% |
| 2017 - 19 | • | - | 44.7% | 21.9% | 71.7% | 93.8% | 121.6% |
| 2018 - 20 | • | - | 28.8% | 8.0% | 53.7% | 87.6% | 122.4% |
| 2019 - 21 | • | - | 36.3% | 15.6% | 60.8% | 95.1% | 127.6% |
| 2020 - 22 | • | - | 42.1% | 21.0% | 66.9% | 100.4% | 127.0% |
| 2021 - 23 | • | - | 50.4% | 28.3% | 76.3% | 109.1% | 129.5% |
Source: NHS England and Office for National Statistics
The excess premature mortality rate from liver disease for people with severe mental ill health compared to those without severe mental ill health has been a little variable in Hull but has been consistently lower than England.
There was a 332% increase in the premature mortality rate from liver disease for people aged 18-74 years with severe mental ill health compared to people without severe mental ill health in Hull for 2015-17, but this has reduced to just over 200% for 2018-20 and is 256% higher for 2021-23. The number of deaths from liver disease is relatively low so the differential is quite variable over time. As noted above around 40% of all the premature deaths from liver disease in 2021-23 in Hull were among people in contact with secondary mental health services. So the differential between people aged 18-74 years with and without severe mental ill health is much greater being between two and three times higher among people with severe mental ill health.
Compared with benchmark
Excess under 75 mortality rate due to liver disease in adults with severe mental illness (SMI) (Persons 18-74 yrs)
|
Period
|
Kingston upon Hull |
Yorkshire and the Humber region (statistical)
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2015 - 17 | • | - | 331.9% | 204.6% | 512.2% | 511.5% | 547.2% |
| 2016 - 18 | • | - | 282.9% | 169.8% | 443.5% | 504.7% | 536.7% |
| 2017 - 19 | • | - | 282.0% | 169.4% | 441.5% | 511.4% | 541.7% |
| 2018 - 20 | • | - | 206.5% | 117.0% | 333.0% | 535.7% | 545.1% |
| 2019 - 21 | • | - | 234.6% | 139.9% | 366.6% | 522.2% | 549.2% |
| 2020 - 22 | • | - | 235.9% | 143.8% | 362.7% | 529.9% | 560.9% |
| 2021 - 23 | • | - | 255.5% | 160.6% | 384.9% | 519.4% | 555.9% |
Source: NHS England and Office for National Statistics
The excess premature mortality rate from respiratory disease for people aged 18-74 years with severe mental ill health compared to people without severe mental ill health has been quite variable over time particularly considering the period of time during the COVID-19 pandemic when premature mortality rates from respiratory disease reduced. However, the percentage has been around 200% (or three times) higher among people with severe mental ill health. The relative percentage difference is greater in 2021-23 with the premature respiratory disease mortality rate being 227% higher which is the highest since 2015-17.
Overall premature respiratory disease mortality rates in Hull have reduced between 2015-17 and 2021-23, and whilst there is no strong trend over time among people with severe mental ill health, the premature respiratory disease mortality rate is amongst the highest in 2021-23 which would explain the high relative difference in 2021-23.
Compared with benchmark
Excess under 75 mortality rate due to respiratory disease in adults with severe mental illness (SMI) (Persons 18-74 yrs)
|
Period
|
Kingston upon Hull |
Yorkshire and the Humber region (statistical)
|
England
|
||||
|---|---|---|---|---|---|---|---|
|
Count
|
Value
|
95%
Lower CI |
95%
Upper CI |
||||
| 2015 - 17 | • | - | 208.9% | 144.4% | 290.4% | 406.2% | 502.6% |
| 2016 - 18 | • | - | 175.6% | 118.9% | 246.9% | 431.9% | 510.6% |
| 2017 - 19 | • | - | 195.5% | 137.4% | 267.9% | 460.6% | 539.9% |
| 2018 - 20 | • | - | 184.7% | 126.7% | 257.6% | 460.2% | 549.4% |
| 2019 - 21 | • | - | 176.1% | 117.3% | 250.9% | 444.0% | 550.1% |
| 2020 - 22 | • | - | 206.7% | 141.0% | 290.3% | 423.6% | 530.5% |
| 2021 - 23 | • | - | 227.0% | 160.0% | 311.3% | 410.8% | 519.7% |
Source: NHS England and Office for National Statistics
Strategic Need and Service Provision
Mental health is a priority locally due to the huge and wide implications. People with mental illness need to be identified early and encouraged to seek help early so that the consequences in terms of the effects on the individual, their family and their employment are minimised. This will reduce the number of issues which escalate and so reduce the levels of need for crisis and/or medical interventions. For both children, young people and adults, help and support should be provided on an individual basis taking into account the person’s circumstances. This early help should be timely, appropriate and build in resilience to help people cope with life challenges. A culture across Hull that celebrates diversity, gives respect and has a zero tolerance on hate crime should be encouraged, so that people feel able to come forward and are not stigmatised by seeking help.
There is a need to work with partners to ensure that services are integrated, high quality and accessible in ways that offer people appropriate choices. People need to be seen quickly and there is a real need to reduce waiting times.
Mental illness is very common, and is generally more debilitating than most chronic physical conditions, yet only a quarter of those with mental illness such as depression are in treatment. NHS England has established a Parity of Esteem Programme in order to focus effort and resources on improving clinical services and health outcomes so that “if I become unwell I use services which assess and treat mental health disorders or conditions on a par with physical health illnesses”. There are three initial priorities for urgent focus: (i) improving access to psychological therapies; (ii) improving diagnosis and support for people with dementia; and (iii) improving awareness and focus on the duties within the Mental Capacity Act.
The Mental Health Crisis Care Concordat is a national agreement between services and agencies involved in the care and support of people in crisis. It sets out how organisations will work together better to make sure that people get the help they need when they are having a mental health crisis. Help is available for organisations and their partners to create and submit a mental health crisis declaration statement and an action plan to make the principles of the Crisis Care Concordat a reality in the local area.
The delivery model of Hull’s Early Help and Prevention offer is focused on a whole family approach which aims to identifies individuals or families with problems (such as those with severe mental ill health) and brings together different services and agencies to collectively look at what support is needed and then work together to deliver the required support in an coordinated way. The aim is to improve outcomes for the entire family as well as reducing demand in the system on more costly, acute and specialist services.
The COVID-19 pandemic has had a wide ranging effect on people affecting all aspects of life. It has been recognised that the pandemic adversely affected mental health and emotional wellbeing, and increased social isolation for some individuals. It is anticipated that there will be an increased need for mental health specialist services in the coming years. The effect on children and young people has been significant. Babies and pre-school children missed baby and toddler groups, nursery and pre-school and so had a lower level of social interaction with others than they would normally be expected to have. Anecdotal evidence suggests that the pandemic has impacted young children’s communication skills development including speech. A higher percentage of children at the end of reception year have been classified as ‘not ready’ for school. Children and young people missed a lot of school and interactions with friends, and reduced structure in their lives. Many children have fallen behind in their schoolwork and a higher percentage of children are not at the expected levels of educational attainment for their age. Young people at transition points – moving from school to further education or the workplace – have been one group significantly affected by the pandemic. The effects on this group include: increased levels of stress and worry associated with examinations being cancelled (and replaced by teacher assessments for qualifications); limited opportunities to attend face to face sessions and interact with peers contributing to feelings of social isolation and heightened levels of anxiety and mental health issues; lost opportunities to access work placements during the pandemic impacting on all young people but especially those who were vocationally unsure and for whom work experience would have been a truly insightful and motivational experience. Professionals working with this age group continue to report increased levels of mental health issues, social anxiety and feelings of ‘hopelessness’. Employment was significantly affected during the pandemic with many staff across different sectors being furloughed or made redundant. A significant number of working-age adults had high levels of uncertainty about their employment, and working-age and older people also had significant concerns over their physical health and COVID-19. The adverse effect on employment for some individuals has meant increased debt. Levels of domestic abuse, smoking and alcohol consumption all increased during the pandemic and lockdowns. The percentage of primary school children who are overweight has increased dramatically in England among the most deprived areas of the country, and it is likely that this has occurred locally too as well as increases in overweight and obesity among adults. There has been a dramatic effect on the NHS and caring sector. Waiting lists have increased which will affect the physical health and emotional wellbeing of many individuals. Friends and relatives of people who died throughout the pandemic (from COVID-19 and other conditions) may not have had the opportunity to see them prior to their death due to visiting restrictions in hospitals and care homes. Additionally, there was an impact on funerals due to strict limits on attendance numbers during lockdown periods which could affect the grieving process. All these factors will have significant impact on mental health and emotional wellbeing. The effects of the pandemic have not been felt evenly across society, and the pandemic has tended to have had a more adverse affect on people living in the most deprived areas thus increasing the inequalities gap.
A Mentally Healthy Hull strategy has been produced which looks at how, as a city, we can collectively boost good mental health and prevent and reduce the impact of mental health problems.
Resources
World Health Organization. Mental disorders, 2019. https://www.who.int/en/news-room/fact-sheets/detail/mental-disorders
Newton JN, Briggs ADM, Murray CJL, et al. Changes in health in England, with analysis by English regions and areas of deprivation, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet, 2015; 6736 (15): 195.
http://dx.doi.org/10.1016/S0140-6736(15)00195-6
Surrey and Borders Partnership NHS Foundation Trust, What is mental illness? Surrey and Borders Partnership NHS Foundation Trust: Leatherhead Surrey, 2014.
Public Health England (now Office for Health Improvement & Disparities). The burden of disease in England compared with 22 peer countries. A report for NHS England. Using data from the Global Burden of Disease 2017.
NHS England, Valuing mental health equally with physical health or “Parity of Esteem”. www.england.nhs.uk. 2015, NHS England: London.
Public Health England (now Office for Health Improvement & Disparities). Smoking cessation in secure mental health settings. Guidance for commissioners. 2015, Public Health England: London.
Public Health England (now Office for Health Improvement & Disparities). Severe Mental Illness and Physical Health Inequalities briefing in 2018. https://www.gov.uk/government/publications/severe-mental-illness-smi-physical-health-inequalities/severe-mental-illness-and-physical-health-inequalities-briefing
Hull’s Early Help and Prevention Strategy 2021-25. https://www.hull.gov.uk/downloads/file/1726/Hull_Early_Help_and_Prevention_Strategy_2021_25.pdf
How are you feeling today? THRIVE Hull. https://www.howareyoufeeling.org.uk/
THRIVE Framework. THRIVE Hull. https://www.howareyoufeeling.org.uk/thriving
HM Government and MIND, Mental Health Crisis Care Concordat. www.crisiscareconcordat.org.uk. 2015, HM Government and MIND: London.
Updates
This page was last updated / checked on 4 March 2025.
This page is due to be updated / checked in August 2025.